Quest for the right Drug
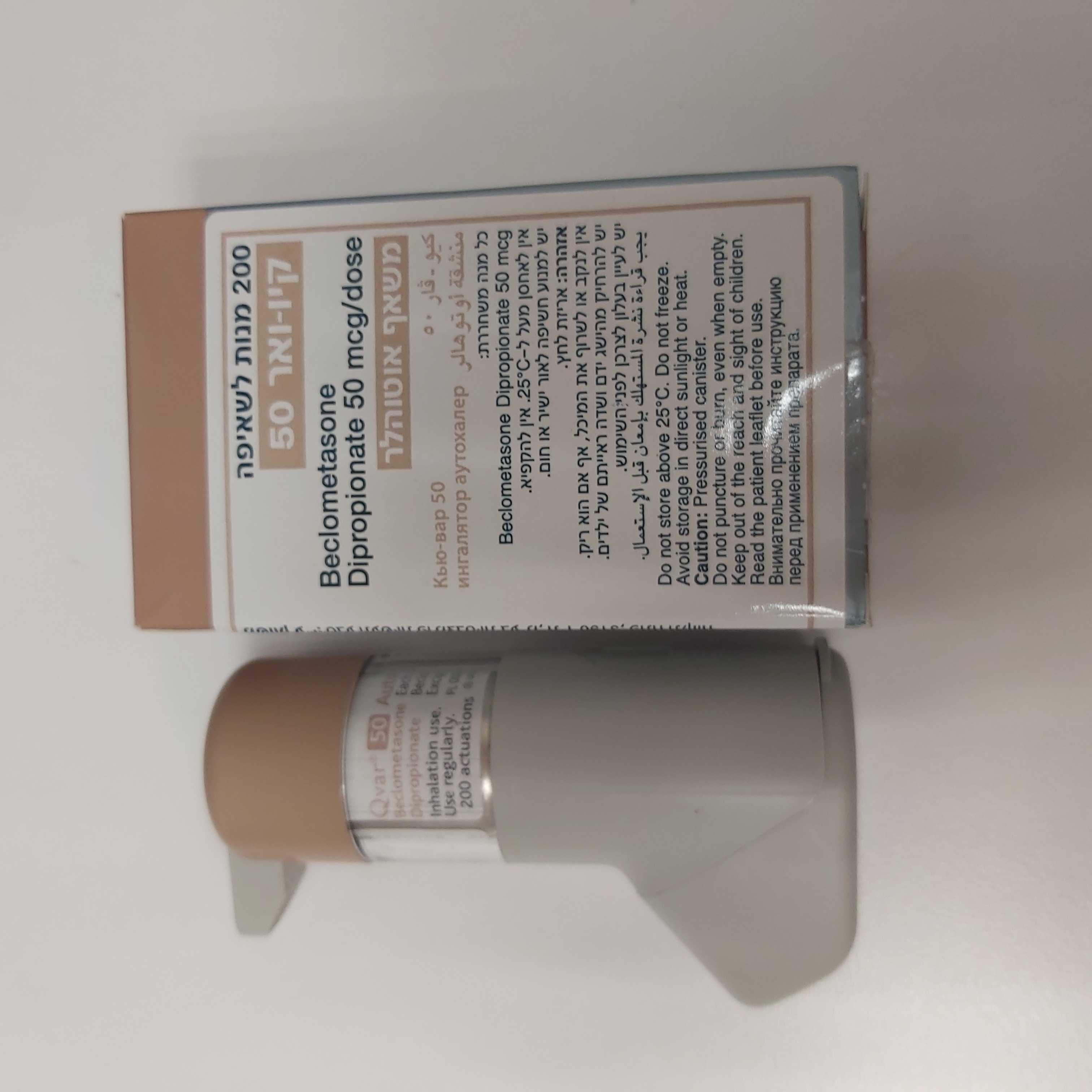
קיו-ואר 50 QVAR 50 (BECLOMETASONE DIPROPIONATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
שאיפה : INHALATION
צורת מינון:
משאף : INHALER
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4. Special warnings and precautions for use Patients should be properly instructed on the use of the inhaler to ensure that the drug reaches the target areas within the lungs. To be effective, Qvar must be used by patients on a regular basis, even when patients do not have asthma symptoms. When symptoms are controlled, maintenance Qvar therapy should be reduced in a stepwise manner to the minimum effective dose. Inhaled steroid treatment should not be stopped abruptly. Patients with asthma are at risk of acute attacks and should have regular assessments of their asthma control including pulmonary function tests. Qvar is not indicated for the immediate relief of asthma attacks. Patients therefore need to have relief medication (inhaled short-acting bronchodilator) available for such circumstances. Severe asthma exacerbations should be managed in the usual way. Subsequently, it may be necessary to increase the dose of extrafine beclometasone dipropionate up to the maximum daily dose. Systemic steroid treatment may be needed and/or an antibiotic, if there is an infection, together with β-agonist therapy, as needed. Severe asthma requires regular medical assessment, including lung-function testing, as there is a risk of severe attacks and even death. Patients should be instructed to seek medical attention as soon as possible for review of beclometasone dipropionate therapy, if their peak flow falls, if symptoms persist or worsen or if their short-acting relief bronchodilator treatment becomes less effective, or more inhalations than usual are required, this may indicate deterioration of asthma control. If this occurs, patients should be assessed and the need for increased anti-inflammatory therapy considered (eg. higher doses of inhaled corticosteroid or a course of oral corticosteroid.) Treatment with Qvar should not be stopped abruptly. Patients who have received systemic steroids for long periods of time or at high doses, or both, need special care and subsequent management when being transferred to inhaled steroid therapy. Patients should have stable asthma before being given inhaled steroids in addition to the usual maintenance dose of systemic steroid. Withdrawal of systemic steroids should be gradual, starting about seven days after the introduction of inhaled steroid therapy. For daily oral doses of prednisolone of 10mg or less, dose reduction in 1mg steps, at intervals of not less than one week is recommended. For patients on daily maintenance doses of oral prednisolone greater than 10mg, larger weekly reductions in the dose might be acceptable. The dose reduction scheme should be chosen to correlate with the magnitude of the maintenance systemic steroid dose. Most patients can be successfully transferred to inhaled steroids with maintenance of good respiratory function, but special care is necessary for the first few months after the transfer, until the hypothalamic-pituitary-adrenal (HPA) axis has sufficiently recovered to enable the patient to cope with stressful emergencies such as trauma, surgery or serious infections. In addition, it may be advisable to provide such patients with a supply of corticosteroid tablets to use in these circumstances. The dose of inhaled steroids should be increased at this time and then gradually reduced to the maintenance level after the systemic steroid has been discontinued. As recovery from impaired adrenocortical function, caused by prolonged systemic steroid therapy is slow, adrenocortical function should be monitored regularly. Patients should be advised that they may feel unwell in a non-specific way during systemic steroid withdrawal despite maintenance of, or even improved respiratory function. Patients should be advised to persevere with their inhaled product and to continue withdrawal of systemic steroids, even if feeling unwell, unless there is evidence of HPA axis suppression. Discontinuation of systemic steroids may also cause exacerbation of allergic diseases such as atopic eczema and rhinitis. These should be treated as required with topical therapy, including corticosteroids and/or antihistamines. Beclometasone dipropionate, like other inhaled steroids, is absorbed into the systemic circulation from the lungs. Beclometasone dipropionate and its metabolites may exert detectable suppression of adrenal function. Within the dose range 100-800 micrograms daily, clinical studies with Qvar have demonstrated mean values for adrenal function and responsiveness within the normal range. However, systemic effects of inhaled corticosteroids may occur, particularly at high doses prescribed for prolonged periods. These effects are much less likely to occur than with oral corticosteroids. Possible systemic effects include Cushing’s syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decrease in bone mineral density, cataract, glaucoma, blurred vision, and more rarely, a range of psychological or behavioural effects including psychomotor hyperactivity, sleep disorders, anxiety, depression or aggression (particularly in children). Therefore, it is important that the dose of inhaled corticosteroid is reviewed regularly and is titrated to the lowest dose at which effective control of asthma is maintained. It is recommended that the height of children receiving prolonged treatment with inhaled corticosteroids is regularly monitored. If growth is slowed, therapy should be reviewed with the aim of reducing the dose of inhaled corticosteroid, if possible, to the lowest dose at which effective control of asthma is maintained. In addition, consideration should be given to referring the patient to a paediatric respiratory specialist. Prolonged treatment with high doses of inhaled corticosteroids, particularly higher than the recommended doses, may result in clinically significant adrenal suppression and acute adrenal crisis. Situations that could potentially trigger acute adrenal crisis include trauma, surgery, infection or any rapid reduction in dose. Presenting symptoms are typically vague and may include anorexia, abdominal pain, weight loss, tiredness, headache, nausea, vomiting, decreased level of consciousness, hypotension, hypoglycaemia and seizures. Additional systemic corticosteroid cover should be considered during periods of stress or elective surgery. Like other corticosteroids, caution is necessary in patients with active or latent pulmonary tuberculosis. As with other inhalation therapy, paradoxical bronchospasm may occur with an immediate increase in wheezing and shortness of breath after dosing. Paradoxical bronchospasm responds to a fast-acting bronchodilator and should be treated straightaway. Beclometasone dipropionate should be discontinued immediately, the patient should be assessed and alternative therapy instituted if necessary. Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Patients should be advised that this product contains small amounts of ethanol. At the normal doses, the amounts of ethanol are negligible and do not pose a risk to patients (see section 4.5).
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
Bronchial asthma
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
