Quest for the right Drug
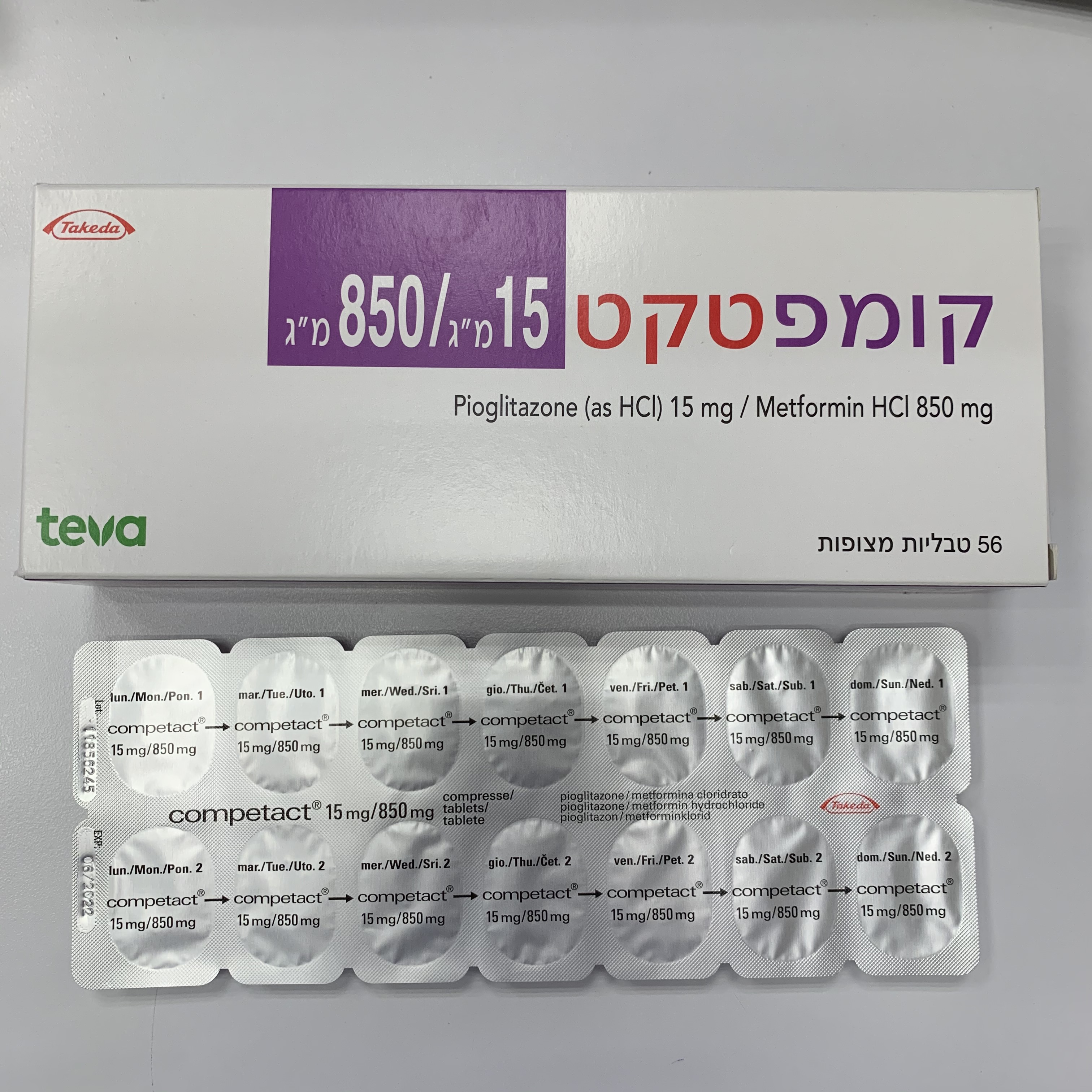
קומפטקט 15 מ"ג / 850 מ"ג COMPETACT 15 MG / 850 MG (METFORMIN HYDROCHLORIDE, PIOGLITAZONE AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs used in diabetes, combinations of oral blood glucose lowering drugs, ATC code: A10BD05. Competact combines two antihyperglycaemic active substances with complementary mechanisms of action to improve glycaemic control in patients with type 2 diabetes mellitus: pioglitazone, a member of the thiazolidinedione class and metformin hydrochloride, a member Competact 15mg/850mg MF 05/2019 Notification of the biguanide class. Thiazolidinediones act primarily by reducing insulin resistance and biguanides act primarily by decreasing endogenous hepatic glucose production. Pioglitazone and metformin combination The fixed dose combination tablet of pioglitazone 15 mg/metformin 850 mg BID (N=201), pioglitazone 15 mg BID (N=189), and metformin 850 mg BID (N=210) were evaluated in type 2 diabetes mellitus patients with mean baseline HbA1C of 9.5% in a randomised double-blind, parallel-group study. Previous anti-diabetic medicinal products were discontinued for 12 weeks prior to baseline measurements. After 24 weeks of treatment, the primary endpoint of mean change from baseline in HbA1c was -1.83% in the combination group versus -0.96% in the pioglitazone group (p< 0.0001) and -0.99% in the metformin group (p< 0.0001). The safety profile seen in this study reflected the known adverse reactions seen with the individual products and did not suggest any new safety issues. Pioglitazone Pioglitazone effects may be mediated by a reduction of insulin resistance. Pioglitazone appears to act via activation of specific nuclear receptors (peroxisome proliferator activated receptor gamma) leading to increased insulin sensitivity of liver, fat and skeletal muscle cells in animals. Treatment with pioglitazone has been shown to reduce hepatic glucose output and to increase peripheral glucose disposal in the case of insulin resistance. Fasting and postprandial glycaemic control is improved in patients with type 2 diabetes mellitus. The improved glycaemic control is associated with a reduction in both fasting and postprandial plasma insulin concentrations. A clinical trial of pioglitazone vs. gliclazide as monotherapy was extended to two years in order to assess time to treatment failure (defined as appearance of HbA1c 8.0% after the first six months of therapy). Kaplan-Meier analysis showed shorter time to treatment failure in patients treated with gliclazide, compared with pioglitazone. At two years, glycaemic control (defined as HbA1c 8.0%) was sustained in 69% of patients treated with pioglitazone, compared with 50% of patients on gliclazide. In a two-year study of combination therapy comparing pioglitazone with gliclazide when added to metformin, glycaemic control measured as mean change from baseline in HbA1c was similar between treatment groups after one year. The rate of deterioration of HbA1c during the second year was less with pioglitazone than with gliclazide. In a placebo controlled trial, patients with inadequate glycaemic control despite a three month insulin optimisation period were randomised to pioglitazone or placebo for 12 months. Patients receiving pioglitazone had a mean reduction in HbA1c of 0.45% compared with those continuing on insulin alone, and a reduction of insulin dose in the pioglitazone treated group. HOMA analysis shows that pioglitazone improves beta cell function as well as increasing insulin sensitivity. Two-year clinical studies have shown maintenance of this effect. In one year clinical trials, pioglitazone consistently gave a statistically significant reduction in the albumin/creatinine ratio compared to baseline. The effect of pioglitazone (45 mg monotherapy vs. placebo) was studied in a small 18-week trial in type 2 diabetics. Pioglitazone was associated with significant weight gain. Visceral fat was significantly decreased, while there was an increase in extra-abdominal fat mass. Similar changes in body fat distribution on pioglitazone have been accompanied by an improvement in insulin sensitivity. In most clinical trials, reduced total plasma triglycerides and free fatty acids, and increased HDL-cholesterol levels were observed as compared to placebo, with small, but not clinically significant increases in LDL-cholesterol levels. In clinical trials of up to two years duration, pioglitazone reduced total plasma triglycerides and free fatty acids, and increased Competact 15mg/850mg MF 05/2019 Notification HDL-cholesterol levels, compared with placebo, metformin or gliclazide. Pioglitazone did not cause statistically significant increases in LDL-cholesterol levels compared with placebo, whilst reductions where observed with metformin and gliclazide. In a 20-week study, as well as reducing fasting triglycerides, pioglitazone reduced postprandial hypertriglyceridaemia through an effect on both absorbed and hepatically synthesised triglycerides. These effects were independent of pioglitazone’s effects on glycaemia and were statistically significantly different to glibenclamide. In PROactive, a cardiovascular outcome study, 5,238 patients with type 2 diabetes mellitus and pre-existing major macrovascular disease were randomised to pioglitazone or placebo in addition to existing antidiabetic and cardiovascular therapy, for up to 3.5 years. The study population had an average age of 62 years; the average duration of diabetes was 9.5 years. Approximately one third of patients were receiving insulin in combination with metformin and/or a sulphonylurea. To be eligible patients had to have had one or more of the following: myocardial infarction, stroke, percutaneous cardiac intervention or coronary artery bypass graft, acute coronary syndrome, coronary artery disease, or peripheral arterial obstructive disease. Almost half of the patients had a previous myocardial infarction and approximately 20% had had a stroke. Approximately half of the study population had at least two of the cardiovascular history entry criteria. Almost all subjects (95%) were receiving cardiovascular medicinal products (beta blockers, ACE inhibitors, angiotensin II antagonists, calcium channel blockers, nitrates, diuretics, acetylsalicylic acid, statins, fibrates). Although the study failed regarding its primary endpoint, which was a composite of all-cause mortality, non-fatal myocardial infarction, stroke, acute coronary syndrome, major leg amputation, coronary revascularisation and leg revascularisation, the results suggest that there are no long-term cardiovascular concerns regarding use of pioglitazone. However, the incidence of oedema, weight gain and heart failure were increased. No increase in mortality from heart failure was observed. Metformin Metformin is a biguanide with antihyperglycaemic effects, lowering both basal and postprandial plasma glucose. It does not stimulate insulin secretion and therefore does not produce hypoglycaemia. Metformin may act via three mechanisms: - by reduction of hepatic glucose production by inhibiting gluconeogenesis and glycogenolysis - in muscle, by modestly increasing insulin sensitivity, improving peripheral glucose uptake and utilisation - by delaying intestinal glucose absorption. Metformin stimulates intracellular glycogen synthesis by acting on glycogen synthase. Metformin increases the transport capacity of specific types of membrane glucose transporters (GLUT-1 and GLUT-4). In humans, independently of its action on glycaemia, metformin has favourable effects on lipid metabolism. This has been shown at therapeutic doses in controlled, medium-term or long-term clinical studies: metformin reduces total cholesterol, LDLc and triglyceride levels. The prospective randomised (UKPDS) study has established the long-term benefit of intensive blood glucose control in type 2 diabetes mellitus. Analysis of the results for overweight patients treated with metformin after failure of diet alone showed: - a significant reduction of the absolute risk of any diabetes-related complication in the metformin group (29.8 events/1,000 patient-years) versus diet alone (43.3 events/1,000 Competact 15mg/850mg MF 05/2019 Notification patient-years), p=0.0023, and versus the combined sulphonylurea and insulin monotherapy groups (40.1 events/1,000 patient-years), p=0.0034 - a significant reduction of the absolute risk of any diabetes-related mortality: metformin 7.5 events/1,000 patient-years, diet alone 12.7 events/1,000 patient-years, p=0.017 - a significant reduction of the absolute risk of overall mortality: metformin 13.5 events/1,000 patient-years versus diet alone 20.6 events/1,000 patient-years, (p=0.011), and versus the combined sulphonylurea and insulin monotherapy groups 18.9 events/1,000 patient-years (p=0.021) - a significant reduction in the absolute risk of myocardial infarction: metformin 11 events/1,000 patient-years, diet alone 18 events/1,000 patient-years, (p=0.01). Paediatric population The European Medicines Agency has waived the obligation to submit the results of studies with Competact in all subsets of the paediatric population in type 2 Diabetes Mellitus. See section 4.2 for information on paediatric use.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Competact Bioequivalence studies in healthy volunteers have shown Competact to be bioequivalent to the administration of pioglitazone and metformin given as separate tablets. Food had no effect on the AUC and Cmax of pioglitazone when Competact was administered to healthy volunteers. However, in the case of metformin, in the fed state the mean AUC and C max were lower (13% and 28% respectively). Tmax was delayed by food by approximately 1.9 h for pioglitazone and 0.8 h for metformin. The following statements reflect the pharmacokinetic properties of the individual active substances of Competact. Pioglitazone Absorption Following oral administration, pioglitazone is rapidly absorbed, and peak plasma concentrations of unchanged pioglitazone are usually achieved 2 hours after administration. Proportional increases of the plasma concentration were observed for doses from 2-60 mg. Steady state is achieved after 4-7 days of dosing. Repeated dosing does not result in accumulation of the compound or metabolites. Absorption is not influenced by food intake. Absolute bioavailability is greater than 80%. Distribution The estimated volume of distribution in humans is 0.25 L/kg. Pioglitazone and all active metabolites are extensively bound to plasma protein (> 99%). Biotransformation Pioglitazone undergoes extensive hepatic metabolism by hydroxylation of aliphatic methylene groups. This is predominantly via cytochrome P450 2C8 although other isoforms may be involved to a lesser degree. Three of the six identified metabolites are active (M-II, M-III, and M-IV). When activity, concentrations and protein binding are taken into account, pioglitazone and metabolite M-III contribute equally to efficacy. On this basis M-IV contribution to efficacy is approximately three-fold that of pioglitazone, whilst the relative efficacy of M-II is minimal. Competact 15mg/850mg MF 05/2019 Notification In vitro studies have shown no evidence that pioglitazone inhibits any subtype of cytochrome P450. There is no induction of the main inducible P450 isoenzymes 1A, 2C8/9, and 3A4 in man. Interaction studies have shown that pioglitazone has no relevant effect on either the pharmacokinetics or pharmacodynamics of digoxin, warfarin, phenprocoumon and metformin. Concomitant administration of pioglitazone with gemfibrozil (an inhibitor of cytochrome P450 2C8) or with rifampicin (an inducer of cytochrome P450 2C8) is reported to increase or decrease, respectively, the plasma concentration of pioglitazone (see section 4.5). Elimination Following oral administration of radiolabelled pioglitazone to man, recovered label was mainly in faeces (55%) and a lesser amount in urine (45%). In animals, only a small amount of unchanged pioglitazone can be detected in either urine or faeces. The mean plasma elimination half-life of unchanged pioglitazone in man is 5 to 6 hours and for its total active metabolites 16 to 23 hours. Elderly Steady state pharmacokinetics are similar in patients age 65 and over and young subjects. Patients with renal impairment In patients with renal impairment, plasma concentrations of pioglitazone and its metabolites are lower than those seen in subjects with normal renal function, but oral clearance of parent substance is similar. Thus free (unbound) pioglitazone concentration is unchanged. Patients with hepatic impairment Total plasma concentration of pioglitazone is unchanged, but with an increased volume of distribution. Intrinsic clearance is therefore reduced, coupled with a higher unbound fraction of pioglitazone. Metformin Absorption After an oral dose of metformin, t max is reached in 2.5 h. Absolute bioavailability of a 500 mg metformin tablet is approximately 50-60% in healthy subjects. After an oral dose, the non-absorbed fraction recovered in faeces was 20-30%. After oral administration, metformin absorption is saturable and incomplete. It is assumed that the pharmacokinetics of metformin absorption is non-linear. At the usual metformin doses and dosing schedules, steady state plasma concentrations are reached within 24-48 h and are generally less than 1 g/mL. In controlled clinical trials, maximum metformin plasma levels (Cmax) did not exceed 4 g/mL, even at maximum doses. Food decreases the extent and slightly delays the absorption of metformin. Following administration of a dose of 850 mg, a 40% lower plasma peak concentration, a 25% decrease in AUC and a 35 min prolongation of time to peak plasma concentration was observed. The clinical relevance of this decrease is unknown. Distribution Plasma protein binding is negligible. Metformin partitions into erythrocytes. The blood peak is lower than the plasma peak and appears at approximately the same time. The red blood cells most likely represent a secondary compartment of distribution. The mean Vd ranged between 63-276 l. Competact 15mg/850mg MF 05/2019 Notification Biotransformation Metformin is excreted unchanged in the urine. No metabolites have been identified in humans. Elimination Renal clearance of metformin is 400 mL/min, indicating that metformin is eliminated by glomerular filtration and tubular secretion. Following an oral dose, the apparent terminal elimination half-life is approximately 6.5 h. When renal function is impaired, renal clearance is decreased in proportion to that of creatinine and thus the elimination half-life is prolonged, leading to increased levels of metformin in plasma.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
