Quest for the right Drug
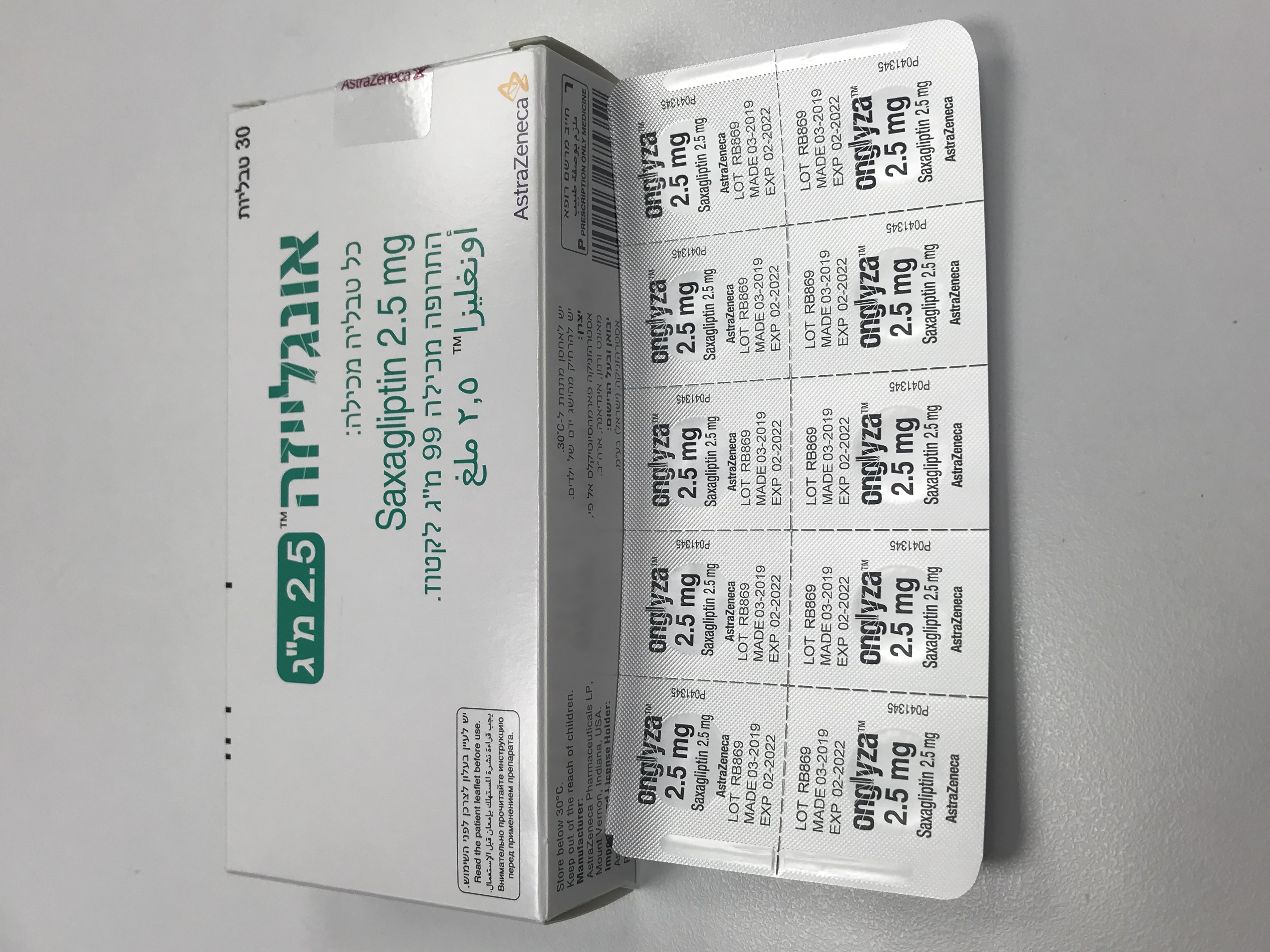
אונגלייזה 2.5 מ"ג ONGLYZA 2.5 MG (SAXAGLIPTIN AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group; Drugs used in diabetes. Dipeptidyl peptidase 4 (DPP-4) inhibitors, ATC code: A10BH03 Mechanism of action and pharmacodynamic effects Saxagliptin is a highly potent (Ki: 1.3 nM), selective, reversible, competitive, DPP-4 inhibitor. In patients with type 2 diabetes, administration of saxagliptin led to inhibition of DPP-4 enzyme activity for a 24-hour period. After an oral glucose load, this DPP-4 inhibition resulted in a 2-to 3-fold increase in circulating levels of active incretin hormones, including glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP), decreased glucagon concentrations and increased glucose-dependent beta-cell responsiveness, which resulted in higher insulin and C-peptide concentrations. The rise in insulin from pancreatic beta-cells and the decrease in glucagon from pancreatic alpha-cells were associated with lower fasting glucose concentrations and reduced glucose excursion following an oral glucose load or a meal. Saxagliptin improves glycaemic control by reducing fasting and postprandial glucose concentrations in patients with type 2 diabetes. Clinical efficacy and safety In randomised, controlled, double-blind clinical trials (including developmental and postmarketing experience), over 17,000 patients with type 2 diabetes have been treated with saxagliptin. Glycaemiccontrol A total of 4,148 patients with type 2 diabetes, including 3,021 patients treated with, saxagliptin were randomised in 6 double-blind, controlled clinical safety and efficacy studies conducted to evaluate the effects of saxagliptin on glycaemic control. Treatment with saxagliptin 5 mg once daily produced clinically relevant and statistically significant improvements in haemoglobin A1c (HbA1c), fasting plasma glucose (FPG) and postprandial glucose (PPG) compared to placebo in monotherapy, in combination with metformin (initial or add-on therapy), in combination with a sulphonylurea, and in combination with a thiazolidinedione (see Table 2). There was also no apparent change in body weight associated with saxagliptin. Reductions in HbA1c were seen across subgroups including gender, age, race, and baseline body mass index (BMI) and higher baseline HbA1c was associated with a greater adjusted mean change from baseline with saxagliptin. Saxagliptin as monotherapy Two double-blind, placebo-controlled studies of 24-week duration were conducted to evaluate the efficacy and safety of saxagliptin monotherapy in patients with type 2 diabetes. In both studies, once- daily treatment with saxagliptin provided significant improvements in HbA1c. (see table 2) The findings of these studies were confirmed with two subsequent 24-week regional (Asian) monotherapy studies comparing saxagliptin 5 mg with placebo. Saxagliptin add-on to metformin therapy An add-on to metformin placebo-controlled study of 24-week duration was conducted to evaluate the efficacy and safety of saxagliptin in combination with metformin in patients with inadequate glycaemic control (HbA1c 7-10%) on metformin alone. Saxagliptin (n=186) provided significant improvements in HbA1c, FPG and PPG compared to placebo (n=175). Improvements in HbA1c, PPG, and FPG following treatment with saxagliptin 5 mg plus metformin were sustained up to Week 102. The HbA1c change for saxagliptin 5 mg plus metformin (n=31) compared to placebo plus metformin (n=15) was -0.8% at Week 102. Saxagliptin add-on to metformin compared with SU add-on to metformin A 52-week study was conducted to evaluate the efficacy and safety of saxagliptin 5 mg in combination with metformin (428 patients) compared with sulphonylurea (glipizide, 5 mg titrated as needed to 20 mg, mean dose of 15 mg) in combination with metformin (430 patients) in 858 patients with inadequate glycaemic control (HbA1c 6.5%-10%) on metformin alone. The mean metformin dose was approximately 1900 mg in each treatment group. After 52 weeks, the saxagliptin and glipizide groups had similar mean reductions from baseline in HbA1c in the per-protocol analysis (-0.7% vs. –0.8%, respectively, mean baseline HbA1c of 7.5% for both groups). The intent-to-treat analysis showed consistent results. The reduction in FPG was slightly less in the saxagliptin-group and there were more discontinuations (3.5% vs. 1.2%) due to lack of efficacy based on FPG criteria during the first 24 weeks of the study. Saxagliptin also resulted in a significantly lower proportion of patients with hypoglycaemia, 3% (19 events in 13 subjects) vs. 36.3% (750 events in 156 patients) for glipizide. Patients treated with saxagliptin exhibited a significant decrease from baseline in body weight compared to a weight gain in patients administered glipizide (-1.1 vs. +1.1 kg). Saxagliptin add-on to metformin compared with sitagliptin add-on to metformin An 18-week study was conducted to evaluate the efficacy and safety of saxagliptin 5 mg in combination with metformin (403 patients), compared with sitagliptin 100 mg in combination with metformin (398 patients) in 801 patients with inadequate glycaemic control on metformin alone. After 18 weeks, saxagliptin was non-inferior to sitagliptin in mean reduction from baseline in HbA1c in both the per- protocol and the full analysis sets . The reductions from baseline in HbA1c respectively for saxagliptin and sitagliptin in the primary per-protocol analysis were -0.5% (mean and median) and -0.6% (mean and median). In the confirmatory full analysis set, mean reductions were -0.4% and -0.6% respectively for saxagliptin and sitagliptin, with median reductions of -0.5% for both groups. Saxagliptin in combination with metformin as initial therapy A 24-week study was conducted to evaluate the efficacy and safety of saxagliptin 5 mg in combination with metformin as initial combination therapy in treatment-naive patients with inadequate glycaemic control (HbA1c 8-12%). Initial therapy with the combination of saxagliptin 5 mg plus metformin (n=306) provided significant improvements in HbA1c, FPG and PPG compared to with either saxagliptin (n=317) or metforminalone (n=313) as initial therapy. Reductions in HbA1c from baseline to Week 24 were observed in all evaluated subgroups defined by baseline HbA1c, with greater reductions observed in patients with a baseline HbA1c ≥10% (see Table 2). Improvements in HbA1c, PPG and FPG following initial therapy with saxagliptin 5 mg plus metformin were sustained up to Week 76. The HbA1c change for saxagliptin 5 mg plus metformin (n=177) compared to metformin plus placebo (n=147) was -0.5% at Week 76. Saxagliptin add-on to glibenclamide therapy An add-on placebo-controlled study of 24-week duration was conducted to evaluate the efficacy and safety of saxagliptin in combination with glibenclamide in patients with inadequate glycaemic control at enrollment (HbA1c 7.5-10%) on a sub-maximal dose of glibenclamide alone. Saxagliptin in combination with a fixed, intermediate dose of a sulphonylurea (glibenclamide 7.5 mg) was compared to titration to a higher dose of glibenclamide (approximately 92% of patients in the placebo plus glibenclamide group were up-titrated to a final total daily dose of 15 mg). Saxagliptin (n=250) provided significant improvements in HbA1c, FPG and PPG compared to titration to a higher dose of glibenclamide (n=264). Improvements in HbA1c and PPG following treatment with saxagliptin 5 mg were sustained up to Week 76. The HbA1c change for saxagliptin 5 mg (n=56) compared to uptitrated glibenclamide plus placebo (n=27) was -0.7% at Week 76. Saxagliptin add-on combination therapy with insulin (with or without metformin) A total of 455 patients with type 2 diabetes participated in a 24-week randomised, double-blind, placebo- controlled study to evaluate the efficacy and safety of saxagliptin in combination with a stable dose of insulin (baseline mean: 54.2 Units) in patients with inadequate glycaemic control (HbA1c 7.5% and 11%) on insulin alone (n=141) or on insulin in combination with a stable dose of metformin (n=314). Saxagliptin 5 mg add-on to insulin with or without metformin provided significant improvements after 24 weeks in HbA1c and PPG compared with placebo add-on to insulin with or without metformin. Similar HbA1c reductions versus placebo were achieved for patients receiving saxagliptin 5 mg add-on to insulin regardless of metformin use (−0.4% for both subgroups). Improvements from baseline HbA1c were sustained in the saxagliptin add-on to insulin group compared to the placebo add-on to insulin group with or without metformin at Week 52. The HbA1c change for the saxagliptin group (n=244) compared to placebo (n=124) was -0.4% at Week 52. Saxagliptin add-on to thiazolidinedione therapy A placebo-controlled study of 24-week duration was conducted to evaluate the efficacy and safety of saxagliptin in combination with a thiazolidinedione (TZD) in patients with inadequate glycaemic control (HbA1c 7-10.5%) on TZD alone. Saxagliptin (n=183) provided significant improvements in HbA1c, FPG and PPG compared to placebo (n=180). Improvements in HbA1c, PPG and FPG following treatment with saxagliptin 5 mg were sustained up to Week 76. The HbA1c change for saxagliptin 5 mg (n=82) compared to TZD plus placebo (n=53) was -0.9% at Week 76. . Patients with renal impairment A 12-week, multi-centre, randomised, double-blind, placebo-controlled study was conducted to evaluate the treatment effect of saxagliptin 2.5 mg once daily compared with placebo in 170 patients (85 patients on saxagliptin and 85 on placebo) with type 2 diabetes (HbA1c 7.0-11%) and renal impairment (moderate [N=90]; severe [N=41]; or ESRD [N=39]). In this study, 98.2% of the patients received other antihyperglycaemic treatments (75.3% on insulin and 31.2% on oral antihyperglycaemics; some received both). Saxagliptin significantly decreased HbA1c compared with placebo; the HbA1c change for saxagliptin was -0.9% at Week 12 (HbA1c change of -0.4% for placebo). Improvements in HbA1c following treatment with saxagliptin 2.5 mg were sustained up to Week 52, however the number of patients who completed 52 weeks without modification of other antihyperglycaemic treatment was low (26 subjects in the saxagliptin group versus 34 subjects in the placebo group). The incidence of confirmed hypoglycaemic events was somewhat higher in the saxagliptin group (9.4%) versus placebo group (4.7%) although the number of subjects with any hypoglycaemic event did not differ between the treatment groups. There was no adverse effect on renal function as determined by estimated glomerular filtration rate or CrCL at Week 12 and Week 52. Table 2. Key efficacy results of Onglyza 5 mg per day in placebo-controlled monotherapy trials and in add-on combination therapy trials Mean change2 Mean from baseline Placebo-corrected baseline HbA1c (%) at mean change in HbA1c Week 24 HbA1c (%) at Week (%) 24 (95% CI) MONOTHERAPY STUDIES • Study CV181011 (n=103) 8.0 -0.5 -0.6 (-0.9, -0.4) 3 • Study CV181038 (n=69) 7.9 -0.7 (morning) -0.4 (-0.7, -0.1) 4 (n=70) 7.9 -0.6 (evening) -0.4 (-0.6, -0.1) 5 ADD-ON/COMBINATION STUDIES • Study CV181014: add-on to metformin -0.8 (-1.0, -0.6) 3 8.1 -0.7 (n=186) • Study CV181040: add-on to SU1 (n=250) 8.5 -0.6 -0.7 (-0.9, -0.6) 3 • Study CV181013: add-on to TZD (n=183) 8.4 -0.9 -0.6 (-0.8, -0.4) 3 • Study CV181039: initial combination with Metformin 6 Overall population (n=306) 9.4 -2.5 -0.5 (-0.7, -0.4) 7 Baseline HbA1c ≥10% strata (n=107) 10.8 -3.3 -0.6 (-0.9, -0.3) 8 Study CV181057: Add-on to insulin 8.7 -0.7 (+/- metformin)Overall population (n=300) n=Randomized patients (primary efficacy-intention-to-treat analysis). 1 Placebo group had uptitration of glibenclamidefrom 7.5 to 15 mg total daily dose. 2 Adjusted mean change from baseline adjusted for baseline value (ANCOVA). 3 p<0.0001 compared to placebo. 4 p=0.0059 compared to placebo. 5 p=0.0157 compared to placebo. 6 Metformin was uptitrated from 500 to 2000 mg per day as tolerated. 7 Mean HbA1c change is the difference between the saxagliptin+metformin and metformin alone groups (p<0.0001). 8 Mean HbA1c change is the difference between the saxagliptin+metformin and metformin alone groups. Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus-Thrombolysis in Myocardial Infarction (SAVOR) study SAVOR was A cv outcome trial in 16,492 patients with HbA1c ≥6.5% and <12% (12959 with established CV disease, 3533 with multiple risk factorsonly) who were . randomised to saxagliptin (n=8280) or placebo (n=8212) added to regional standards of care for HbA1c and CV risk factors. The study populationincluded those ≥65 years, (n=8561) and ≥75 years ≥(n=2330), with normal or mild renal impairment (n=13,916) as well as moderate (n=2240) or severe (n=336) renal impairment. The primary safety (noninferiority) and efficacy (superiority) endpoint was a composite endpoint consisting of the time-tofirst occurrence of any of the following major adverse CV events (MACE): CV death, nonfatal myocardial infarction, or nonfatal ischemic stroke. after a mean follow up of 2 years, the trial met its primary safety endpoint demonstrating saxagliptin does not increase the cardiovascular risk in patientswith type 2 diabetes compared to placebo when added to current background therapy, no benefit was observed for MACE or all-cause mortality. Table 3: Primary and Secondary Clinical Endpoints by Treatment Group in the SAVOR Study * Saxagliptin Placebo (N=8280) (N=8212) Subjects with Event rate Subjects Hazard events per 100 with events Event rate per Ratio Endpoint n (%) patient-yrs n (%) 100 patient-yrs (95% CI)† Primary composite 613 3.76 609 3.77 1.00 endpoint: MACE (7.4) (7.4) (0.89, 1.12)‡,§, # Secondary composite 1059 6.72 1034 6.60 1.02 endpoint: MACE plus (12.8) (12.6) (0.94, 1.11)¶ All-cause mortality 420 2.50 378 2.26 1.11 (5.1) (4.6) (0.96, 1.27)¶ * Intent-to-treat population † Hazard ratio adjusted for baseline renal function category and baseline CVD risk category. ‡ p-value <0.001 for noninferiority (based on HR <1.3) compared to placebo. § p-value = 0.99 for superiority (based on HR <1.0) compared to placebo. # Events accumulated consistently over time, and the event rates for ONGLYZA and placebo did not diverge notably over time. ¶ Significance not tested. One component of the secondary composite endpoint, hospitalization for heart failure, occurred at a greater rate in the saxagliptin group (3.5%) compared with the placebo group (2.8%), with nominal statistical significance (favouring placebo [HR = 1.27; (95% CI 1.07, 1.51); P = 0.007]. Clinically relevant factors predictive of increased relative risk with saxagliptin treatment could not be definitively identified. Subjects at higher risk for hospitalization for heart failure, irrespective of treatment assignment, could be identified by known risk factors for heart failure such as baseline history of heart failure or impaired renal function. However, subjects on saxagliptin with a history of heart failure or impaired renal function at baseline were not at an increased risk relative to placebo for the primary or secondary composite endpoints or all-cause mortality. Another secondary endpoint all-cause mortality, occurred at a rate of 5.1% in the saxagliptin group and 4.6% in the placebo group (see Table 4). CV deaths were balanced across the treatment groups. There was a numerical imbalance in non-CV death, with more events on saxagliptin (1.8%) than placebo (1.4%) [HR = 1.27; ( 95% CI: 1.00, 1.62); P = 0.051]. A1C was lower with saxagliptin compared to in an exploratory analysis. Paediatric population The European Medicines Agency has deferred the obligation to submit the results of studies with Onglyza in one or more subsets of the paediatric population in the treatment of type 2 diabetes mellitus (see section 4.2 for information on paediatric use) Elderly population In the SAVOR study subgroups over 65 and over 75 years of age, efficacy and safety were consistent with the overall study population. GENERATION was a 52-week glycaemic control study in 720 elderly patients, the mean age was 72.6 years; 433 subjects (60.1%) were < 75 years of age, and 287 subjects (39.9%) were ≥ 75 years of age. Primary endpoint was the proportion of patients reaching HbA1c < 7% without confirmed or severe hypoglycaemia. There appeared to be no difference in percentage responders: 37.9% (saxagliptin) and 38.2% (glimepiride) achieved the primary endpoint. A lower proportion of patients in the saxagliptin group (44.7%) compared to the glimepiride group (54.7%) achieved an HbA1c target of 7.0%. A lower proportion of patients in the saxagliptin group (1.1%) compared to the glimepiride group (15.3%) experienced a confirmed or severe hypoglycaemic event.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of saxagliptin and its major metabolite were similar in healthy subjects and in patients with type 2 diabetes. Absorption Saxagliptin was rapidly absorbed after oral administration in the fasted state, with maximum plasma concentrations (Cmax) of saxagliptin and its major metabolite attained within 2 and 4 hours (Tmax), respectively. The Cmax and AUC values of saxagliptin and its major metabolite increased proportionally with the increment in the saxagliptin dose, and this dose-proportionality was observed in doses up to 400 mg. Following a 5 mg single oral dose of saxagliptin to healthy subjects, the mean plasma AUC values for saxagliptin and its major metabolite were 78 ng·h/ml and 214 ng·h/ml, respectively. The corresponding plasma Cmax values were 24 ng/ml and 47 ng/ml, respectively. The intra-subject coefficients of variation for saxagliptin Cmax and AUC were less than 12%. The inhibition of plasma DPP-4 activity by saxagliptin for at least 24 hours after oral administration of saxagliptin is due to high potency, high affinity, and extended binding to the active site. Interaction with food Food had relatively modest effects on the pharmacokinetics of saxagliptin in healthy subjects. Administration with food (a high-fat meal) resulted in no change in saxagliptin Cmax and a 27% increase in AUC compared with the fasted state. The time for saxagliptin to reach Cmax (Tmax) was increased by approximately 0.5 hours with food compared with the fasted state. These changes were not considered to be clinically meaningful. Distribution The in vitro protein binding of saxagliptin and its major metabolite in human serum is negligible. Thus, changes in blood protein levels in various disease states (e.g., renal or hepatic impairment) are not expected to alter the disposition of saxagliptin. Biotransformation The biotransformation of saxagliptin is primarily mediated by cytochrome P450 3A4/5 (CYP3A4/5). The major metabolite of saxagliptin is also a selective, reversible, competitive DPP-4 inhibitor, half as potent as saxagliptin. Elimination The mean plasma terminal half-life (t1/2) values for saxagliptin and its major metabolite are 2.5 hours and 3.1 hours respectively, and the mean t1/2 value for plasma DPP-4 inhibition was 26.9 hours. Saxagliptin is eliminated by both renal and hepatic pathways. Following a single 50 mg dose of 14C-saxagliptin, 24%, 36%, and 75% of the dose was excreted in the urine as saxagliptin, its major metabolite, and total radioactivity respectively. The average renal clearance of saxagliptin (∼230 ml/min) was greater than the average estimated glomerular filtration rate (∼120 ml/min), suggesting some active renal excretion. For the major metabolite, renal clearance values were comparable to estimated glomerular filtration rate. A total of 22% of the administered radioactivity was recovered in faeces representing the fraction of the saxagliptin dose excreted in bile and/or unabsorbed medicinal product from the gastrointestinal tract. Linearity The Cmax and AUC of saxagliptin and its major metabolite increased proportionally to the saxagliptin dose. No appreciable accumulation of either saxagliptin or its major metabolite was observed with repeated once-daily dosing at any dose level. No dose-and time-dependence was observed in the clearance of saxagliptin and its major metabolite over 14 days of once-daily dosing with saxagliptin at doses ranging from 2.5 mg to 400 mg. Special populations Renal impairment A single-dose, open-label study was conducted to evaluate the pharmacokinetics of a 10 mg oral dose of saxagliptin in subjects with varying degrees of chronic renal impairment compared to subjects with normal renal function. The study included patients with renal impairment classified on the basis of creatinine clearance (based on the Cockcroft-Gault formula) a mild (>50 to ≤80 ml/min), moderate (≥30 to ≤50 ml/min), or severe ( ≤30 ml/min) as well as patients with ESRD on haemodialysis The degree of renal impairment did not affect the Cmax of saxagliptin or its major metabolite. In subjects with mild renal impairment, the mean AUC values of saxagliptin and its major metabolite were 1.2- and 1.7- fold higher, respectively, than mean AUC values in subjects with normal renal function. Because increases of this magnitude are not clinically relevant, dose adjustment in patients with mild renal impairment is not recommended. In subjects with moderate or severe renal impairment or in subjects with ESRD on haemodialysis, the AUC values of saxagliptin and its major metabolite were up to 2.1- and 4.5-fold higher, respectively, than AUC values in subjects with normal renal function. The dose of Onglyza should be reduced to 2.5 mg once daily in patients with moderate or severe renal impairment (see sections 4.2 and 4.4). Hepatic impairment In subjects with mild (Child-Pugh Class A), moderate (Child-Pugh Class B), or severe (Child-Pugh Class C) hepatic impairment the exposures to saxagliptin were 1.1-, 1.4- and 1.8-fold higher, respectively, and the exposures to BMS-510849 were 22%, 7%, and 33% lower, respectively, than those observed in healthy subjects. Elderly patients (≥65 years) Elderly (65-80 years) had about 60% higher saxagliptin AUC than young patients (18-40 years). This is not considered clinically meaningful, therefore, no dose adjustment for Onglyza is recommended on the basis of age alone.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
