Quest for the right Drug
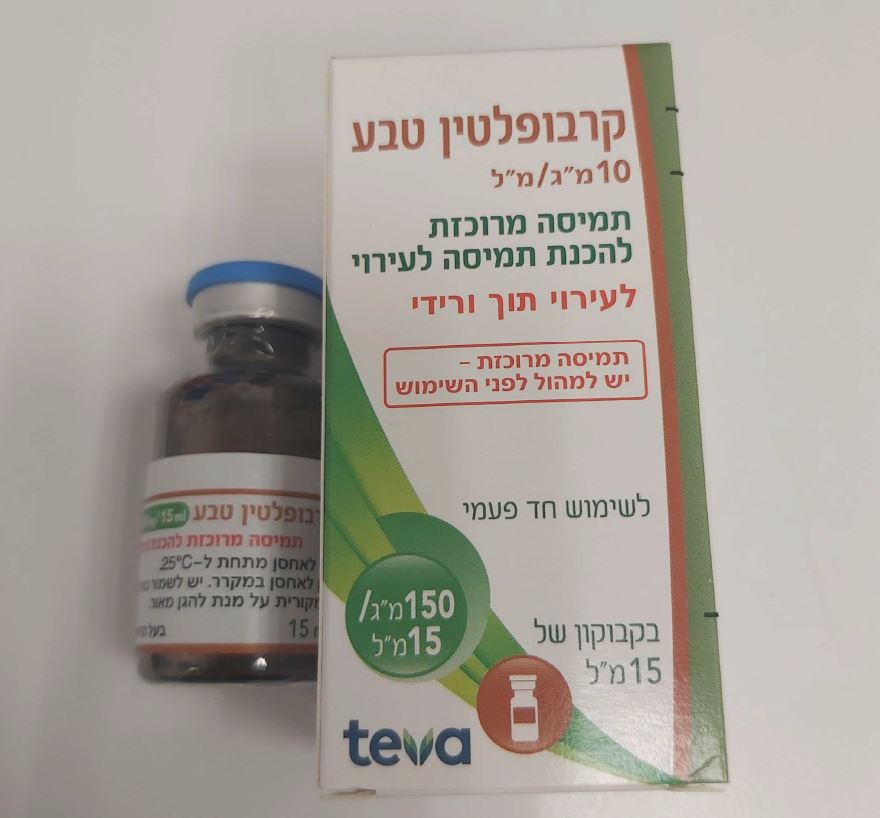
קרבופלטין טבע CARBOPLATIN TEVA (CARBOPLATIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Carboplatin should be used only by physicians experienced with cancer chemotherapeutic drugs. Blood counts as well as renal and hepatic function tests must be done regularly and the drug should be discontinued if abnormal depression of the bone marrow or abnormal renal or hepatic function is seen. Hematologic toxicity Leukopenia, neutropenia, and thrombocytopenia are dose-dependent and dose-limiting. Peripheral blood counts should be monitored during carboplatin treatment frequently and, in case of toxicity, until recovery is achieved. Median day of nadir is day 21 in patients receiving single agent carboplatin and day 15 in patients receiving carboplatin in combination with other chemotherapeutic agents. In general, single intermittent courses of carboplatin should not be repeated until leukocyte, neutrophil, and platelet counts have returned to normal. Therapy should not be repeated until 4 weeks after the previous carboplatin course and/or until the neutrophil count is at least 2,000 cells/mm3 and the platelet count is at least 100,000 cells/mm3. Anaemia is frequent and cumulative, requiring very rarely a transfusion. Hemolytic anaemia with the presence of serologic drug-induced antibodies has been reported in patients treated with carboplatin. This event can be fatal. Severity of myelosuppression is increased in patients with prior treatment (in particular with cisplatin) and/or impaired kidney function. Initial carboplatin dosages in these groups of patients should be appropriately reduced (see section 4.2) and the effects carefully monitored through frequent blood counts between courses. Carboplatin combination therapy with other myelosuppressive forms of treatment must be planned very carefully with respect to dosages and timing in order to minimise additive effects. Myelosuppressive effects may be additive to those of concomitant chemotherapy. Patients with severe and persistent myelosuppression are at high risk of infectious complications including fatal outcomes (see section 4.8). If any of these events occurs, carboplatin dosing should be interrupted and dose modification or discontinuation should be considered. Acute promyelocytic leukaemia and myelodysplastic syndrome (MDS)/ acute myeloid leukemia (AML) have been reported years after therapy with carboplatin and other antineoplastic treatments. Nausea and vomiting Carboplatin can cause nausea and vomiting. Pre-medication with antiemetics and slower drug administration have been reported to be useful in reducing the incidence and intensity of these effects. Haemolytic-uraemic syndrome (HUS) Haemolytic-uraemic syndrome (HUS) is a life-threatening side effect. Carboplatin should be discontinued at the first signs of any evidence of microangiopathic haemolytic anaemia, such as rapidly falling haemoglobin with concomitant thrombocytopenia, elevation of serum bilirubin, serum creatinine, blood urea nitrogen, or LDH. Renal failure may not be reversible with discontinuation of therapy and dialysis may be required. Carboplatin Teva EM 12/2023 Notification Hypersensitivity reactionsAs with other platinum-based drugs, allergic reactions appearing most often during perfusion may occur and necessitate discontinuation of the perfusion and an appropriate symptomatic treatment. Cross reactions, sometimes fatal, have been reported with all the platinum compounds (see section 4.3 and section 4.8). There have been reports of hypersensitivity reactions which progressed to Kounis syndrome (acute allergic coronary arteriospasm that can result in myocardial infarction, see section 4.8). Renal toxicity In patients with impaired renal function, the effect of carboplatin on the haematopoietic system is more pronounced and longer-acting than in patients with normal renal function. In this risk group, therapy with carboplatin must be performed with special caution (see section 4.2). Neurologic toxicity Although peripheral neurologic toxicity is generally common and mild, limited to paraesthesia and decrease of osteotendinous reflexes, its frequency is increased in patients older than 65 years and/or in patients previously treated with cisplatin. Monitoring and neurological examinations should be carried out at regular intervals. Visual disturbances, including loss of vision, have been reported after the use of carboplatin in doses higher than those recommended in patients with renal impairment. Vision appears to recover totally or to a significant extent within weeks of stopping these high doses. Geriatric use In studies involving combination therapy with carboplatin and cyclophosphamide, elderly patients treated with carboplatin were more likely to develop severe thrombocytopenia than younger patients. Because renal function is often decreased in the elderly, renal function should be considered when determining dosage (see section 4.2). Reversible Posterior Leukoencephalopathy Syndrome (RPLS) Cases of Reversible Posterior Leukoencephalopathy Syndrome (RPLS) have been reported in patients receiving carboplatin in combination chemotherapy. RPLS is a rare, reversible after treatment discontinuation, rapidly evolving neurological condition, which can include seizure, hypertension, headache, confusion, blindness, and other visual and neurological disturbances (see section 4.8). Diagnosis of RPLS is based upon confirmation by brain imaging, preferably MRI (Magnetic Resonance Imaging). Venoocclusive liver disease Cases of hepatic venoocclusive disease (sinusoidal obstruction syndrome) have been reported, some of which were fatal. Patients should be monitored for signs and symptoms of abnormal liver function or portal hypertension which do not obviously result from liver metastases. Tumour lysis syndrome (TLS) In post-marketing experience tumour lysis syndrome (TLS) has been reported in patients following the use of carboplatin alone or in combination with other chemotherapeutic agents. Patients at high risk of TLS, such as patients with high proliferative rate, high tumour burden, and high sensitivity to cytotoxic agents, should be monitored closely and appropriate precaution taken. Other Auditory defects have been reported during carboplatin therapy. Ototoxicity may be more pronounced in children. Cases of hearing loss with a delayed onset have been reported in paediatric patients. A long-term audiometric follow-up in this population is recommended. Carboplatin Teva EM 12/2023 Notification Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents, including carboplatin, may result in serious or fatal infections. Vaccination with a live vaccine should be avoided in patients receiving carboplatin. Killed or inactivated vaccines may be administered; however, the response to such vaccines may be diminished. Men and women should use effective methods of contraception (see section 4.6). Paediatric population Safety and efficacy of carboplatin in paediatric patients have not been established.
Effects on Driving
4.7 Effects on ability to drive and use machines No studies on the effects on the ability to drive and use machines have been performed. However, carboplatin may cause nausea, vomiting, vision abnormalities and ototoxicity; therefore, patients should be warned on the potential effect of these events on the ability to drive or to use machines.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
