Quest for the right Drug
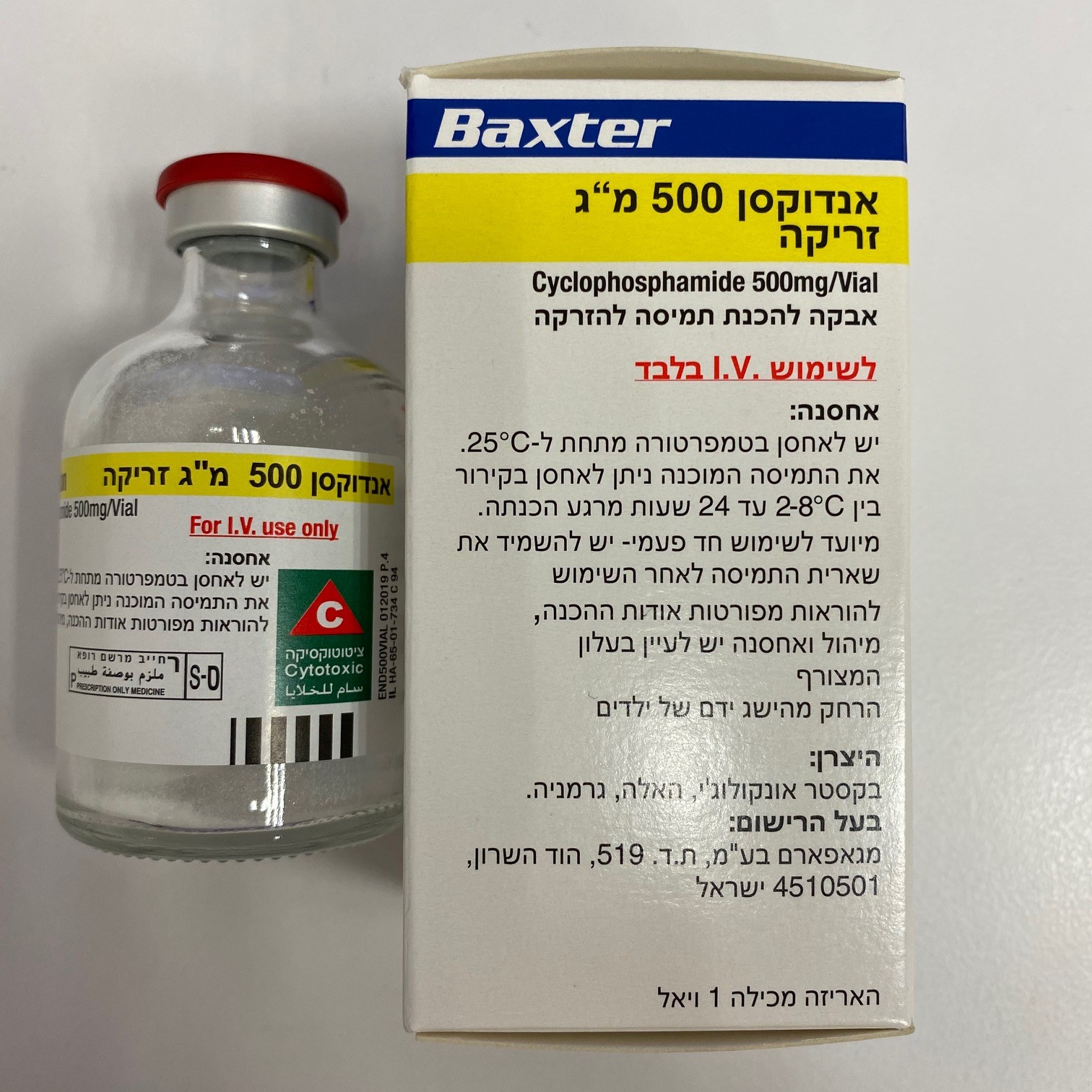
אנדוקסן 500 מ"ג זריקה ENDOXAN 500 MG INJECTION (CYCLOPHOSPHAMIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use WARNINGS Myelosuppression, immunosuppression, infections • Treatment with Endoxan can cause myelosuppression and significant suppression of immune response. • Cyclophosphamide-induced myelosuppression can cause leukopenia, neutropenia, thrombocytopenia (associated with a higher risk of bleeding) and anemia. • Severe immunosuppression has led to serious, sometimes fatal infections. Sepsis and septic shock have also been reported. Infections reported with cyclophosphamide include pneumonias as well as other bacterial, fungal, viral, protozoal and parasitic infections. • Latent infections can be reactivated. Reactivation has been reported for various bacterial, fungal, viral, protozoal, and parasitic infections. • Infections must be treated appropriately. • Antimicrobial prophylaxis may be indicated in certain cases of neutropenia at the discretion of the managing physician. • In the event of neutropenic fever, antibiotics and/or antifungals must be given. • Cyclophosphamide should be used with caution, if at all, in patients with severe impairment of bone marrow function and in patients with severe immunosuppression. • Unless essential, cyclophosphamide should not be administered to patients with a leukocyte count below 2500 cells/microlitre (cells/mm3 and/or a platelet count below 50,000 cells/microlitre (cells/mm3). • Cyclophosphamide treatment may not be indicated, or should be interrupted, or the dose reduced, in patients who have or who develop a serious infection. • In principle, the fall in the peripheral blood cell and thrombocyte count and the time taken to recover may increase with increasing doses of cyclophosphamide. • The nadirs of the reduction in leukocyte count and thrombocyte count are usually reached in weeks 1 and 2 of treatment. The bone marrow recovers relatively quickly, and the levels of peripheral blood cell counts normalize, as a rule, after approximately 20 days. • Severe myelosuppression must be expected particularly in patients pretreated with and/or receiving concomitant chemotherapy and/or radiation therapy. • Close hematological monitoring is required for all patients during treatment. Urinary tract and renal toxicity • Hemorrhagic cystitis, pyelitis, ureteritis, and hematuria have been reported with cyclophosphamide therapy. Bladder ulceration/necrosis, fibrosis/contracture and secondary malignancies may develop. • Urotoxicity may mandate interruption of treatment. • Cystectomy may become necessary due to fibrosis, bleeding, or secondary malignancy. • Cases of urotoxicity with fatal outcomes have been reported. • Urotoxicity can occur with short-term and long-term use of Endoxan. Hemorrhagic cystitis after single doses of cyclophosphamide has been reported. • Past or concomitant radiation or busulfan treatment may increase the risk of cyclophosphamide-induced hemorrhagic cystitis. • Cystitis is, in general, initially abacterial. Secondary bacterial colonization may follow. • Before starting treatment, it is necessary to exclude or correct any urinary tract obstructions (see section 4.3). • Urinary sediment should be checked regularly for the presence of erythrocytes and other signs of uro/nephrotoxicity. • Cyclophosphamide should be used with caution, if at all, in patients with active urinary tract infections. • Adequate treatment with mesna and/or strong hydration to force diuresis can markedly reduce the frequency and severity of bladder toxicity. It is important to ensure that patients empty the bladder at regular intervals. • Hematuria usually resolves in a few days after cyclophosphamide treatment is stopped, but it may persist. • It is usually necessary to discontinue cyclophosphamide therapy in instances of severe hemorrhagic cystitis. • Cyclophosphamide has also been associated with nephrotoxicity, including tubular necrosis. • Hyponatremia associated with increased total body water, acute water intoxication, and a syndrome resembling SIADH (syndrome of inappropriate antidiuretic hormone secretion) have been reported in association with cyclophosphamide administration. Fatal outcomes have been reported. Cardiotoxicity: Use in patients with cardiac disease • Myocarditis and myopericarditis, which may be accompanied by pericardial effusion and cardiac tamponade, have been reported with cyclophosphamide therapy and have led to severe, sometimes fatal congestive heart failure. • Histopathologic examination has primarily shown hemorrhagic myocarditis. Hemopericardium has occurred secondary to hemorrhagic myocarditis and myocardial necrosis. • Acute cardiac toxicity has been reported with a single dose of less than 2 mg/kg cyclophosphamide. • Following exposure to treatment regimens that included cyclophosphamide, supraventricular arrhythmias (including atrial fibrillation and flutter) as well as ventricular arrhythmias (including severe QT prolongation associated with ventricular tachyarrhythmias) have been reported in patients with and without other signs of cardiotoxicity. • The risk of cyclophosphamide cardiotoxicity may be increased for example following high doses of cyclophosphamide, in patients of advanced age, and in patients with previous radiation treatment of the cardiac region and/or previous or concomitant treatment with other cardiotoxic agents (see section 4.5). • Particular caution is necessary in patients with risk factors for cardiotoxicity and in patients with pre-existing cardiac disease. Pulmonary toxicity • Pneumonitis and pulmonary fibrosis have been reported during and following treatment with cyclophosphamide. Pulmonary veno-occlusive disease and other forms of pulmonary toxicity have also been reported. • Pulmonary toxicity leading to respiratory failure has been reported. • While the incidence of cyclophosphamide-associated pulmonary toxicity is low, prognosis for affected patients is poor. • Late onset of pneumonitis (more than 6 months after initiation of cyclophosphamide treatment) appears to be associated with particularly high mortality. Pneumonitis may develop even years after treatment with cyclophosphamide. • Acute pulmonary toxicity has been reported after a single cyclophosphamide dose. Secondary malignancies • As with all cytotoxic therapies, treatment with cyclophosphamide involves the risk of secondary tumors and their precursors as late sequelae. • The risk of urinary tract cancer as well as the risk of myelodysplastic alterations, partly progressing to acute leukemias, is increased. Other malignancies reported after use of cyclophosphamide or regimens with cyclophosphamide include lymphoma, thyroid cancer, and sarcomas. • In some cases, the second malignancy developed several years after cyclophosphamide treatment had been discontinued. Malignancy has also been reported after in utero exposure. Veno-occlusive liver disease • Veno-occlusive liver disease (VOLD) has been reported in patients receiving cyclophosphamide. • Cytoreductive therapy in preparation for bone marrow transplantation consisting of cyclophosphamide in combination with whole-body irradiation, busulfan or other agents has been identified as a major risk factor for the development of VOLD (see section 4.5). After cytoreductive therapy, the clinical syndrome typically develops 1 to 2 weeks after transplantation and is characterized by sudden weight gain, painful hepatomegaly, ascites and hyperbilirubinemia/jaundice. • However, VOLD has also been reported to develop gradually in patients receiving long- term low-dose immunosuppression with cyclophosphamide. • As a complication of VOLD, hepatorenal syndrome and multiple organ failure may develop. Fatal outcome of cyclophosphamide-associated VOLD has been reported. • Risk factors predisposing a patient to the development of VOLD with high-dose cytoreductive therapy include: - preexisting disturbances of hepatic function, - previous radiation treatment of the abdomen and a - low performance scores. Genotoxicity • Cyclophosphamide is genotoxic and mutagenic, both in somatic and in male and female germ cells. Therefore, women should not become pregnant, and men should not father a child during treatment with cyclophosphamide. • Both women and men should wait at least 6 to 12 months after stopping Cyclophosphamide before attempting to conceive or father a child. • Animal study data indicate that exposure of oocytes during follicular development may result in a decreased rate of implantations and viable pregnancies, and in an increased risk of malformations. This effect should be considered in case of intended fertilization or pregnancy after discontinuation of cyclophosphamide therapy. The exact duration of follicular development in humans is not known but may be longer than 12 months. • Sexually active women and men should use an effective method of contraception during this period of time (see section 4.6.). • Fertility, see section 4.6 Anaphylactic reactions, cross-sensitivity with other alkylating agents Anaphylactic reactions including those with fatal outcomes have been reported in association with cyclophosphamide. Possible cross-sensitivity with other alkylating agents has been reported. Impairment of wound healing Cyclophosphamide may interfere with normal wound healing. PRECAUTIONS Alopecia • Alopecia has been reported and may occur more commonly with increasing doses. • Alopecia may progress to baldness. • The hair can be expected to grow back after treatment with the drug or even during continued drug treatment but may differ in texture or color. Nausea and vomiting • Administration of cyclophosphamide may cause nausea and vomiting. • Current guidelines on the use of antiemetics for prevention and relief of nausea and vomiting should be considered. • Alcohol consumption may increase cyclophosphamide-induced vomiting and nausea. Stomatitis • Administration of cyclophosphamide may cause stomatitis (oral mucositis). • Current guidelines on measures for prevention and relief of stomatitis should be considered. Para-venous injection • The cytostatic effect of cyclophosphamide occurs after its activation, which takes place mainly in the liver. Therefore, the risk of tissue injury from accidental para-venous injection is low. • In the event of accidental para-venous injection of cyclophosphamide, the infusion should be stopped immediately, and the extravascular cyclophosphamide solution should be aspirated with the cannula in place. Other measures may need to be instituted as appropriate. Use in adrenalectomized patients Patients with adrenal insufficiency may require an increase in corticoid substitution dose when exposed to stress from toxicity due to cytostatics, including cyclophosphamide. Use in Patients with Renal Impairment In patients with renal impairment, particularly in patients with severe renal impairment, decreased renal excretion may result in increased plasma levels of cyclophosphamide and its metabolites. This may result in increased toxicity and should be considered when determining the dosage in such patients. See Section 4.2. Use in Patients with Hepatic Impairment Severe hepatic impairment may be associated with decreased activation of cyclophosphamide. This may alter the effectiveness of cyclophosphamide treatment and should be considered when selecting the dose and interpreting response to the dose selected.
Effects on Driving
4.7 Effects on ability to drive and use machines Patients undergoing treatment with cyclophosphamide may experience undesirable effects (including, e.g., dizziness, blurred vision, visual impairment) which could affect the ability to drive or use machines. The decision to drive or operate machinery should be made on an individual basis.

שימוש לפי פנקס קופ''ח כללית 1994
Hodgkin's disease, malignant lymphomas, multiple myeloma, mycosis fungoides, neuroblastoma, autoimmune disease
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף