Quest for the right Drug
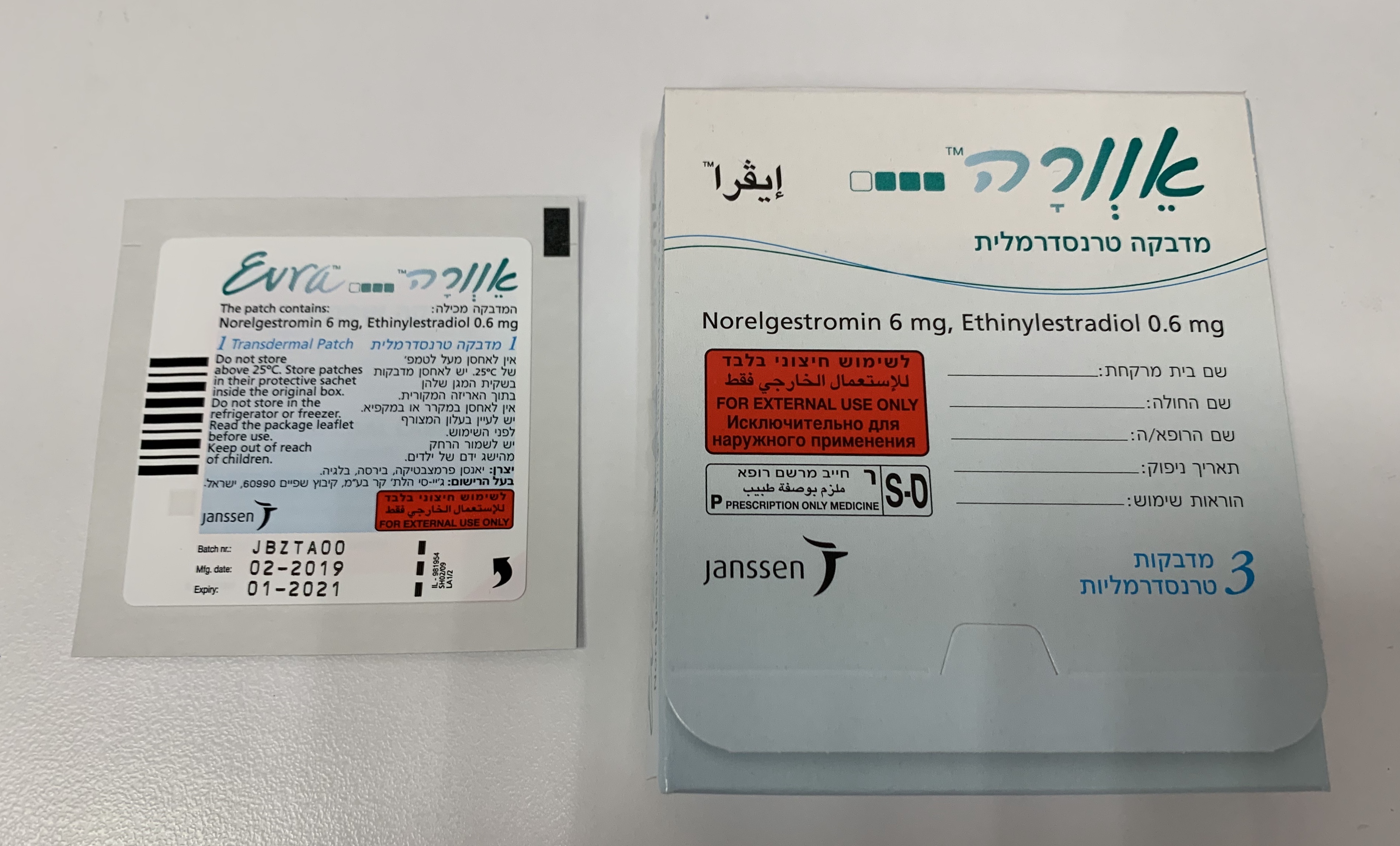
אוורה EVRA (ETHINYLESTRADIOL, NORELGESTROMIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
בין-עורי : TRANSDERMAL
צורת מינון:
מדבקות : PATCHES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Warnings If any of the conditions/risk factors mentioned below is present, the suitability of EVRA should be discussed with the woman. In the event of aggravation, or first appearance of any of the conditions or risk factors, the woman should be advised to contact her doctor to determine whether the use of EVRA should be discontinued. There is no clinical evidence indicating that a transdermal patch is, in any aspect, safer than combined oral contraceptives. EVRA is not indicated during pregnancy (see section 4.6). Risk of venous thromboembolism (VTE) The use of any combined hormonal contraceptive (CHC) increases the risk of venous thromboembolism (VTE) compared with no use. Products that contain levonorgestrel, norgestimate or norethisterone are associated with the lowest risk of VTE. Other products such as EVRA may have up to twice this level of risk. The decision to use any product other than one with the lowest VTE risk should be taken only after a discussion with the woman to ensure she understands the risk of VTE with EVRA, how her current risk factors influence this risk, and that her VTE risk is highest in the first ever year of use. There is also some evidence that the risk is increased when a CHC is re-started after a break in use of 4 weeks or more. In women who do not use a CHC and are not pregnant about 2 out of 10,000 will develop a VTE over the period of one year. However, in any individual woman the risk may be far higher, depending on her underlying risk factors (see below). It is estimated that out of 10,000 women who use a low dose CHC that contains levonorgestrel, about 6 1 will develop a VTE in one year. Studies have suggested that the incidence of VTE in women who used EVRA is up to 2-fold higher than in users of CHCs that contain levonorgestrel. This corresponds to between about 6 and 12 VTEs in a year out of 10,000 women who use EVRA. In both cases, the number of VTEs per year is fewer than the number expected in women during pregnancy or in the postpartum period. VTE may be fatal in 1-2% of cases. Number of VTE events per 10,000 women in one year Extremely rarely, thrombosis has been reported to occur in CHC users in other blood vessels, e.g. hepatic, mesenteric, renal or retinal veins and arteries. 1 Mid-point of range of 5-7 per 10,000 WY, based on a relative risk for CHCs containing levonorgestrel versus non-use of approximately 2.3 to 3.6 Risk factors for VTE The risk for venous thromboembolic complications in CHC users may increase substantially in a woman with additional risk factors, particularly if there are multiple risk factors (see table). EVRA is contraindicated if a woman has multiple risk factors that put her at high risk of venous thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors – in this case her total risk of VTE should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3). Table: Risk factors for VTE Risk factor Comment Obesity (body mass index over Risk increases substantially as BMI rises. 30 kg/m²) Particularly important to consider if other risk factors also present. Prolonged immobilisation, major In these situations it is advisable to discontinue the surgery, any surgery to the legs or use of the patch (in the case of elective surgery at pelvis, neurosurgery, or major trauma least four weeks in advance) and not resume until two weeks after complete remobilisation. Another Note: temporary immobilisation method of contraception should be used to avoid including air travel > 4 hours can also unintentional pregnancy. be a risk factor for VTE, particularly Antithrombotic treatment should be considered if in women with other risk factors EVRA has not been discontinued in advance Positive family history (venous If a hereditary predisposition is suspected, the thromboembolism ever in a sibling or woman should be referred to a specialist for advice parent at relatively early age) before deciding about any CHC use Other medical conditions associated Cancer, systemic lupus erythematosus, haemolytic with VTE uraemic syndrome, chronic inflammatory bowel disease (Crohn's disease or ulcerative colitis) and sickle cell disease Increasing age Particularly above 35 years There is no consensus about the possible role of varicose veins and superficial thrombophlebitis in the onset or progression of venous thrombosis. The increased risk of thromboembolism in pregnancy, and particularly the 6 week period of the puerperium, must be considered (for information on "Pregnancy and lactation" see section 4.6). Symptoms of VTE (deep vein thrombosis and pulmonary embolism) In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC. Symptoms of deep vein thrombosis (DVT) can include: - unilateral swelling of the leg and/or foot or along a vein in the leg; - pain or tenderness in the leg which may be felt only when standing or walking, - increased warmth in the affected leg; red or discoloured skin on the leg. Symptoms of pulmonary embolism (PE) can include: - sudden onset of unexplained shortness of breath or rapid breathing; - sudden coughing which may associated with haemoptysis; - sharp chest pain; - severe light headedness or dizziness; - rapid or irregular heartbeat. Some of these symptoms (e.g. “shortness of breath”, “coughing”) are non-specific and might be misinterpreted as more common or less severe events (e.g. respiratory tract infections). Other signs of vascular occlusion can include: sudden pain, swelling and slight blue discoloration of an extremity. If the occlusion occurs in the eye symptoms can range from painless blurring of vision which can progress to loss of vision. Sometimes loss of vision can occur almost immediately. Risk of arterial thromboembolism (ATE) Epidemiological studies have associated the use of CHCs with an increased risk for arterial thromboembolism (myocardial infarction) or for cerebrovascular accident (e.g. transient ischaemic attack, stroke). Arterial thromboembolic events may be fatal. Risk factors for ATE The risk of arterial thromboembolic complications or of a cerebrovascular accident in CHC users increases in women with risk factors (see table). EVRA is contraindicated if a woman has one serious or multiple risk factors for ATE that puts her at high risk of arterial thrombosis (see section 4.3). If a woman has more than one risk factor, it is possible that the increase in risk is greater than the sum of the individual factors - in this case her total risk should be considered. If the balance of benefits and risks is considered to be negative a CHC should not be prescribed (see section 4.3). Table: Risk factors for ATE Risk factor Comment Increasing age Particularly above 35 years Smoking Women should be advised not to smoke if they wish to use a CHC. Women over 35 who continue to smoke should be strongly advised to use a different method of contraception. Hypertension Obesity (body mass index over 30 kg/m2) Risk increases substantially as BMI rises. Particularly important in women with additional risk factors Positive family history (arterial If a hereditary predisposition is suspected, the thromboembolism ever in a sibling or parent woman should be referred to a specialist for at relatively early age e.g. below 50). advice before deciding about any CHC use Migraine An increase in frequency or severity of migraine during CHC use (which may be prodromal of a cerebrovascular event) may be a reason for immediate discontinuation Other medical conditions associated with Diabetes mellitus, hyperhomocysteinaemia, adverse vascular events valvular heart disease and atrial fibrillation, dyslipoproteinaemia, systemic lupus erythematosus. Symptoms of ATE In the event of symptoms women should be advised to seek urgent medical attention and to inform the healthcare professional that she is taking a CHC. Symptoms of a cerebrovascular accident can include: - sudden numbness or weakness of the face, arm or leg, especially on one side of the body; - sudden trouble walking, dizziness, loss of balance or coordination; - sudden confusion, trouble speaking or understanding; - sudden trouble seeing in one or both eyes; - sudden, severe or prolonged headache with no known cause; - loss of consciousness or fainting with or without seizure. Temporary symptoms suggest the event is a transient ischaemic attack (TIA). Symptoms of myocardial infarction (MI) can include: - pain, discomfort, pressure, heaviness, sensation of squeezing or fullness in the chest, arm, or below the breastbone; - discomfort radiating to the back, jaw, throat, arm, stomach; - feeling of being full, having indigestion or choking; - sweating, nausea, vomiting or dizziness; - extreme weakness, anxiety, or shortness of breath; - rapid or irregular heartbeats. Women using combined contraceptives should be emphatically advised to contact their physician in case of possible symptoms of thrombosis. In case of suspected or confirmed thrombosis, hormonal contraceptive use should be discontinued. Adequate contraception should be initiated because of the teratogenicity of anti-coagulant therapy (coumarins). Tumours An increased risk of cervical cancer in long-term users of COCs has been reported in some epidemiological studies, but there continues to be controversy about the extent to which this finding is attributable to the confounding effects of sexual behaviour and other factors such as human papilloma virus (HPV). A meta-analysis of 54 epidemiological studies reported that there is a slightly increased risk (RR = 1.24) of having breast cancer diagnosed in women who are currently using COCs. The excess risk gradually disappears during the course of the 10 years after cessation of COC use. Because breast cancer is rare in women under 40 years of age, the excess number of breast cancer diagnoses in current and recent COC users is small in relation to the overall risk of breast cancer. The breast cancers diagnosed in ever-users tend to be less advanced clinically than the cancers diagnosed in never- users. The observed pattern of increased risk may be due to an earlier diagnosis of breast cancer in COC users, the biological effects of COCs or a combination of both. In rare cases, benign liver tumours, and even more rarely, malignant liver tumours have been reported in users of COCs. In isolated cases, these tumours have led to life-threatening intra- abdominal haemorrhages. Therefore a hepatic tumour should be considered in the differential diagnosis when severe upper abdominal pain, liver enlargement or signs of intra-abdominal haemorrhage occur in women using EVRA. ALT elevations During clinical trials with patients treated for hepatitis C virus infections (HCV) with the medicinal products containing ombitasvir/paritaprevir/ritonavir and dasabuvir with or without ribavirin, transaminase (ALT) elevations higher than 5 times the upper limit of normal (ULN) occurred significantly more frequent in women using ethinyl estradiol-containing medications such as combined hormonal contraceptives (CHCs) (see sections 4.3 and 4.5). Psychiatric Disorders Depressed mood and depression are well-known undesirable effects of hormonal contraceptive use (see section 4.8). Depression can be serious and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment. Other conditions - Contraceptive efficacy may be reduced in women weighing equal or greater than 90 kg (see sections 4.2 and 5.1). - Women with hypertriglyceridaemia, or a family history thereof, may be at an increased risk of pancreatitis when using combined hormonal contraceptives. - Although small increases of blood pressure have been reported in many women using hormonal contraceptives, clinically relevant increases are rare. A definitive relationship between hormonal contraceptive use and clinical hypertension has not been established. If, during the use of combined hormonal contraceptives in pre-existing hypertension, constantly elevated blood pressure values or a significant increase in blood pressure do not respond adequately to antihypertensive treatment, the combined hormonal contraceptive must be withdrawn. Combined hormonal contraceptive use may be resumed if normotensive values can be achieved with antihypertensive therapy. - The following conditions have been reported to occur or deteriorate with both pregnancy and COC use, but the evidence of an association with COC use is inconclusive: Jaundice and/or pruritus related to cholestasis; gallbladder disease including cholecystitis and cholelithiasis; porphyria; systemic lupus erythematosus; haemolytic ureamic syndrome; Sydenham’s chorea; herpes gestationis; otosclerosis-related hearing loss. - Acute or chronic disturbances of liver function may necessitate the discontinuation of combined hormonal contraceptives until markers of liver function return to normal. Recurrence of cholestatic-related pruritus, which occurred during a previous pregnancy or previous use of sex steroids necessitates the discontinuation of combined hormonal contraceptives. - Although combined hormonal contraceptives may have an effect on peripheral insulin resistance and glucose tolerance, there is no evidence for a need to alter the therapeutic regimen in diabetes during use of combined hormonal contraceptives. However, diabetic women should be carefully observed, particularly in the early stage of EVRA use. - Worsening of endogenous depression, of epilepsy, of Crohn’s disease and of ulcerative colitis has been reported during COC use. - Chloasma may occasionally occur with the use of hormonal contraception, especially in Users with a history of chloasma gravidarum. Users with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation while using EVRA. Chloasma is often not fully reversible. Medical examination/consultation Prior to the initiation or reinstitution of EVRA a complete medical history (including family history) should be taken and pregnancy should be ruled out. Blood pressure should be measured and a physical examination should be performed guided by the contra-indications (see section 4.3) and warnings (see section 4.4). It is important to draw a woman’s attention to the information on venous and arterial thrombosis, including the risk of EVRA compared with other CHCs, the symptoms of VTE and ATE, the known risk factors and what to do in the event of a suspected thrombosis. The woman should also be instructed to carefully read the user leaflet and to adhere to the advice given. The frequency and nature of examinations should be based on established practice guidelines and be adapted to the individual woman. Women should be advised that hormonal contraceptives do not protect against HIV infections (AIDS) and other sexually transmissible diseases. Bleeding irregularities With all combined hormonal contraceptives, irregular blood loss (spotting or breakthrough bleeding) can occur, especially during the initial months of usage. For this reason, a medical opinion on irregular blood loss will only be useful after an adjustment period of approximately three cycles. If breakthrough bleeding persists, or breakthrough bleeding occurs after previously regular cycles, while EVRA has been used according to the recommended regimen, a cause other than EVRA should be considered. Non-hormonal causes should be considered and, if necessary, adequate diagnostic measures taken to rule out organic disease or pregnancy. This may include curettage. In some women withdrawal bleeding may not occur during this transdermal patch free period. If EVRA has been taken according to the directions described in section 4.2, it is unlikely that the woman is pregnant. However, if EVRA has not been taken according to these directions prior to the first missed withdrawal bleed or if two withdrawal bleeds are missed, pregnancy must be ruled out before EVRA use is continued. Some users may experience amenorrhoea or oligomenorrhoea after discontinuing hormonal contraception, especially when such a condition was pre-existent.
Effects on Driving
4.7 Effects on ability to drive and use machines EVRA has no or negligible influence on the ability to drive and use machines.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
רישום
130 21 30818 00
מחיר
0 ₪
מידע נוסף
עלון מידע לצרכן
04.04.21 - עלון לצרכן אנגלית 04.04.21 - עלון לצרכן עברית 04.04.21 - עלון לצרכן ערבית 08.09.22 - עלון לצרכן אנגלית 08.09.22 - עלון לצרכן עברית 08.09.22 - עלון לצרכן ערבית 29.11.11 - החמרה לעלון 04.12.11 - החמרה לעלון 16.07.12 - החמרה לעלון 01.06.16 - החמרה לעלון 19.12.17 - החמרה לעלון 09.10.20 - החמרה לעלון 04.04.21 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אוורה