Quest for the right Drug
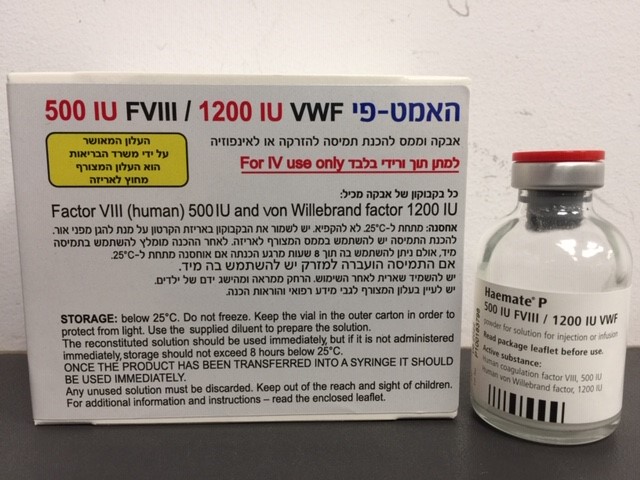
האמט פי 500IU FVIII / 1200IU VWF HAEMATE P 500 IU FVIII / 1200 IU VWF (FACTOR VIII (HUMAN), VON WILLEBRAND FACTOR)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה וממס להכנת תמיסה להזרקהאינפוזיה : POWDER AND SOLVENT FOR SOLUTION FOR INJECTION/INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
5. DOSAGE AND ADMINISTRATION Treatment of VWD and haemophilia A should be supervised by a physician experienced in the treatment of haemostatic disorders. Posology von Willebrand's disease: It is important to calculate the dose using the number of IU of VWF:RCo specified. Generally, 1 IU/kg VWF:RCo raises the circulating level of VWF:RCo by 0.02 IU/ml (2 %). Levels of VWF:RCo of > 0.6 IU/ml (60%) and of FVIII:C of > 0.4 IU/ml (40%) should be achieved. Usually 40 - 80 IU/kg of von Willebrand factor (VWF:RCo) and 20 - 40 IU FVIII:C/kg of body weight (BW) are recommended to achieve haemostasis. An initial dose of 80 IU/kg von Willebrand factor may be required, especially in patients with type 3 von Willebrand disease where maintenance of adequate levels may require greater doses than in other types of von Willebrand disease. Prevention of haemorrhage in case of surgery or severe trauma: For prevention of excessive bleeding during or after surgery, the injection should start 1 to 2 hours before the surgical procedure. An appropriate dose should be re-administered every 12 - 24 hours. The dose and duration of the treatment depend on the clinical status of the patient, the type and severity of bleeding, and both VWF:RCo and FVIII:C levels. When using a FVIII-containing von Willebrand factor product, the treating physician should be aware that continued treatment may cause an excessive rise in FVIII:C. After 24 - 48 hours of treatment, in order to avoid an uncontrolled rise in FVIII:C, reduced doses and/or prolongation of the dose interval should be considered. Paediatric population Dosing in children is based on body weight and is therefore generally based on the same guidelines as for adults. The frequency of administration should always be oriented to the clinical effectiveness in the individual case. Haemophilia A It is important to calculate the dose using the number of IU of FVIII:C specified. The dosage and duration of the substitution therapy depend on the severity of the factor VIII deficiency, on the location and extent of the bleeding, and on the patient’s clinical condition. The number of units of factor VIII administered is expressed in International Units (IU), which are related to the current WHO standard for factor VIII products. Factor VIII activity in plasma is expressed either as a percentage (relative to normal human plasma) or in IU (relative to an International Standard for factor VIII in plasma). One IU of factor VIII activity is equivalent to that quantity of factor VIII in one ml of normal human plasma. On demand treatment The calculation of the required dosage of factor VIII is based on the empirical finding that 1 IU factor VIII per kg body weight raises the plasma factor VIII activity by about 2 % (2 IU/dl) of normal activity. The required dosage is determined using the following formula: Required units = body weight [kg] x desired factor VIII rise [% or IU/dl] x 0.5. The amount to be administered and the frequency of administration should always be oriented to the clinical effectiveness in the individual case. In the case of the following haemorrhagic events, the factor VIII activity should not fall below the given plasma activity level (in % of normal or IU/dl) within the corresponding period. The following table can be used to guide dosing in bleeding episodes and surgery: Degree of haemorrhage/ Type Factor VIII level Frequency of doses (hours) / of surgical procedure required (% or IU/dl) Duration of therapy (days) Haemorrhage Early haemarthrosis, muscle 20 - 40 Repeat every 12 - 24 hours. bleeding or oral bleeding At least 1 day, until the bleeding episode as indicated by pain is resolved or healing is achieved. More extensive haemarthrosis, 30 - 60 Repeat infusion every muscle bleeding or haematoma 12 - 24 hours for 3 - 4 days or more until pain and acute disability are resolved. Life-threatening haemorrhages 60 - 100 Repeat infusion every 8 - 24 hours until threat is resolved. Surgery Minor 30 - 60 Every 24 hours, at least 1 day, including tooth extraction until healing is achieved. Major 80 - 100 Repeat infusion every (pre- and 8 - 24 hours until adequate postoperative) wound healing, then therapy for at least another 7 days to maintain a factor VIII activity of 30% - 60% (IU/dl). HAEMATE P Prophylaxis For long-term prophylaxis against bleeding in patients with severe haemophilia A, the usual doses are 20 to 40 IU of factor VIII per kg body weight at intervals of 2 to 3 days. In some cases, especially in younger patients, shorter dosage intervals or higher doses may be necessary. During the course of treatment, appropriate determination of factor VIII levels is advised to guide the dose to be administered and the frequency of repeated infusions. In the case of major surgical interventions in particular, a precise monitoring of the substitution therapy by means of coagulation analysis (plasma factor VIII activity) is indispensable. Individual patients may vary in their response to factor VIII, achieving different levels of in vivo recovery and demonstrating different half-lives. Patients should be monitored for the development of factor VIII inhibitors. Previously untreated patients The safety and efficacy of Haemate P in previously untreated patients have not yet been established. Paediatric population There are no data available from clinical studies regarding the dosage of Haemate P in children. Method of administration For intravenous use. Reconstitute the product as described in section 5.1. The reconstituted preparation should be warmed to room or body temperature before administration. Inject slowly intravenously at a rate comfortable for the patient. Once the product is transferred into the syringe, it should be used immediately. In case larger amounts of the factor have to be administered, this can also be done by infusion. For this purpose, transfer the reconstituted product into an approved infusion system. The injection or infusion rate should not exceed 4 ml per minute. Observe the patient for any immediate reaction. If any reaction takes place that might be related to the administration of Haemate P, the rate of infusion should be decreased or the application should be stopped, as required by the clinical condition of the patient. Page 4 of 25 HAEMATE P 5.1 Reconstitution Bring the solvent to room temperature. Ensure Haemate P and solvent vial flip-caps are removed and the stoppers are treated with an antiseptic solution and allowed to dry prior to opening the Mix2Vial package. 1. Open the Mix2Vial package by peeling off the lid. Do not remove the Mix2Vial from the blister package! 1 2. Place the solvent vial on an even, clean surface and hold the vial tight. Take the Mix2Vial together with the blister package and push the spike of the blue adapter end straight down through the solvent vial stopper. 2 3. Carefully remove the blister package from the Mix2Vial set by holding at the rim, and pulling vertically upwards. Make sure that you only pull away the blister package and not the Mix2Vial set. 3 4. Place the Haemate P vial on an even and firm surface. Invert the solvent vial with the Mix2Vial set attached and push the spike of the transparent adapter end straight down through the Haemate P vial stopper. The solvent will automatically flow into the Haemate P vial. 4 Page 5 of 25 HAEMATE P 5. With one hand, grasp the Haemate P-side of the Mix2Vial set and with the other hand, grasp the solvent side and unscrew the set carefully into two pieces to avoid excessive build-up of foam when dissolving the Haemate P. Discard the solvent vial with the blue Mix2Vial adapter attached. 5 6. Gently swirl the Haemate P vial with the transparent adapter attached until the substance is fully dissolved. Do not shake. 6 7. Draw air into an empty, sterile syringe. While the Haemate P vial is upright, connect the syringe to the Mix2Vial´s Luer Lock fitting. Inject air into the Haemate P vial. 7 Withdrawal and application 8. While keeping the syringe plunger pressed, turn the system upside down and draw the solution into the syringe by pulling the plunger back slowly. 8 9. Now that the solution has been transferred into the syringe, firmly hold on to the barrel of the syringe (keeping the syringe plunger facing down) and disconnect the transparent Mix2Vial adapter from the syringe. 9 For injection of Haemate P, the use of plastic disposable syringes is recommended as the ground glass surfaces of all-glass syringes tend to stick with solutions of this type. Administer solution slowly intravenously (see section 5), taking care to ensure that no blood enters the syringe filled with product. Any unused product or waste material should be disposed of in accordance with national requirements. Page 6 of 25 HAEMATE P 5.2 Administration HAEMATE P is for intravenous use only. The solution should be clear or slightly opalescent. After filtering/withdrawal, the reconstituted product should be inspected visually for particulate matter and discoloration prior to administration. Even if the directions for use for the reconstitution procedure are precisely followed, it is not uncommon for a few flakes or particles to remain. The filter included in the Mix2Vial device removes those particles completely. Filtration does not influence dosage calculations. Do not use visibly cloudy solutions or solutions still containing flakes or particles after filtration. From a microbiological point of view and as Haemate P contains no preservative, the reconstituted product should be used immediately. If it is not administered immediately, storage shall not exceed 3 hours below 25°C. Once the product has been transferred into a syringe, it should be used immediately. Discard the administration equipment and any unused HAEMATE P after use.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
