Quest for the right Drug
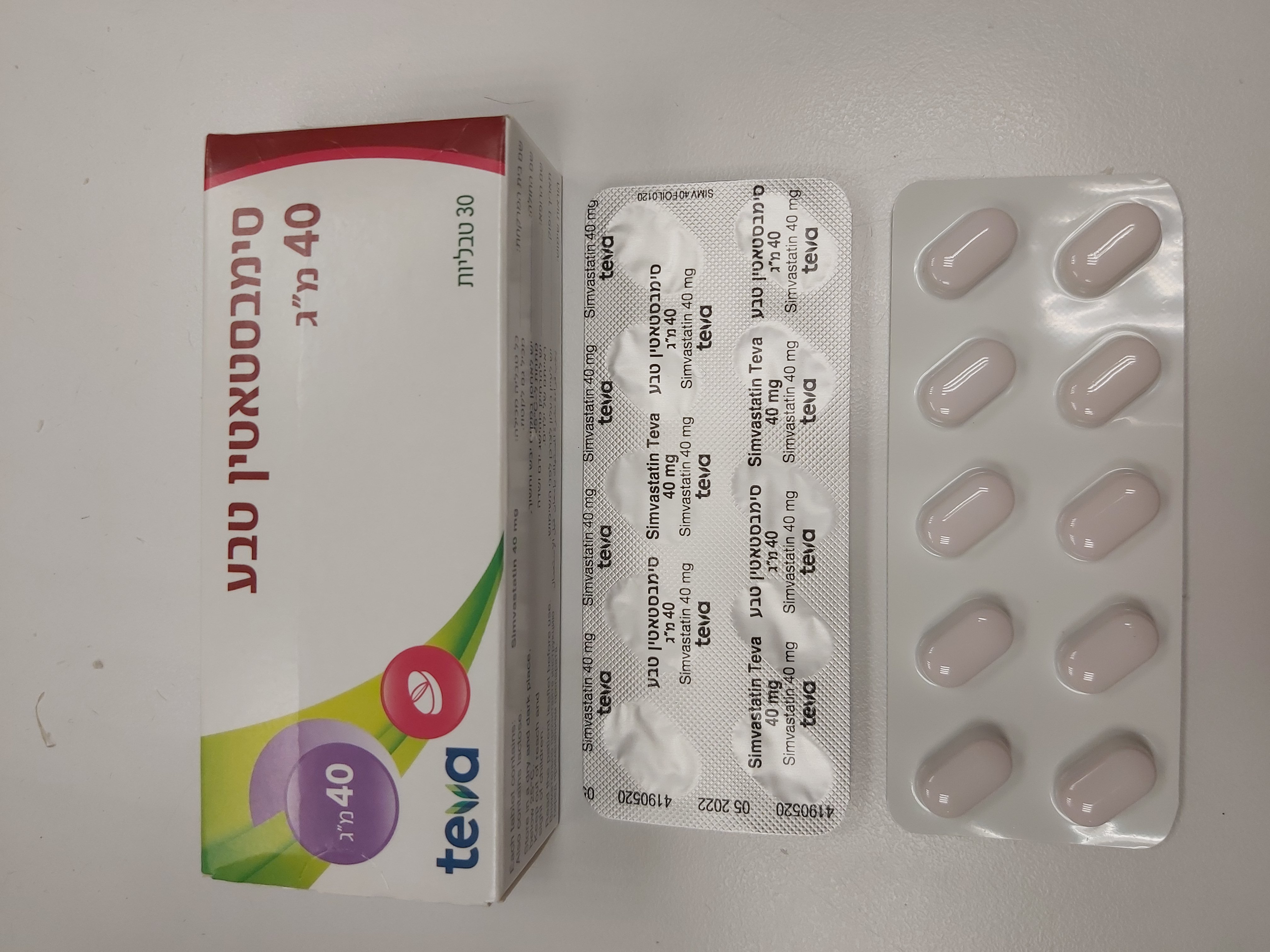
סימבסטאטין טבע ® 40 מ"ג SIMVASTATIN TEVA ® 40 MG (SIMVASTATIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Myopathy/Rhabdomyolysis Simvastatin, like other inhibitors of HMG-CoA reductase, occasionally causes myopathy manifested as muscle pain, tenderness or weakness with creatine kinase (CK) above ten times the upper limit of normal (ULN). Myopathy sometimes takes the form of rhabdomyolysis with or without acute renal failure secondary to myoglobinuria, and very rare fatalities have occurred. The risk of myopathy is increased by high levels of HMG-CoA reductase inhibitory activity in plasma (i.e., elevated simvastatin and simvastatin acid plasma levels), which may be due, in part, to interacting drugs that interfere with simvastatin metabolism and/or transporter pathways (see section 4.5). As with other HMG-CoA reductase inhibitors, the risk of myopathy/rhabdomyolysis is dose-related. In a clinical trial database, in which 41,413 patients were treated with simvastatin, 24,747 (approximately 60%) of whom were enrolled in studies with a median follow-up of at least 4 years, the incidence of myopathy was approximately 0.03%, 0.08% and 0.61% at 20, 40 and 80 mg/day, respectively. In these trials, patients were carefully monitored and some interacting medicinal products were excluded. In a clinical trial in which patients with a history of myocardial infarction were treated with simvastatin 80 mg/day (mean follow-up 6.7 years), the incidence of myopathy was approximately 1.0% compared with 0.02% for patients on 20 mg/day. Approximately half of these myopathy cases occurred during the first year of treatment. The incidence of myopathy during each subsequent year of treatment was approximately 0.1% (see sections 4.8 and 5.1). The risk of myopathy is greater in patients on simvastatin 80 mg compared with other statin-based therapies with similar LDL-C-lowering efficacy. Therefore, the 80-mg dose of simvastatin should only be used in patients with severe hypercholesterolemia and at high risk for cardiovascular complications who have not achieved their treatment goals on lower doses and when the benefits are expected to outweigh the potential risks. In patients taking simvastatin 80 mg for whom an interacting agent is needed, a lower dose of simvastatin or an alternative statin-based regimen with less potential for drug-drug interactions should be used (see below Measures to reduce the risk of myopathy caused by medicinal product interactions and sections 4.2, 4.3, and 4.5). In a clinical trial in which patients at high risk of cardiovascular disease were treated with simvastatin 40 mg/day (median follow-up 3.9 years), the incidence of myopathy was approximately 0.05 % for non-Chinese patients (n =7367) compared with 0.24 % for Chinese patients (n = 5468). While the only Asian population assessed in this clinical trial was Chinese, caution should be used when prescribing simvastatin to Asian patients and the lowest dose necessary should be employed. Reduced function of transport proteins Reduced function of hepatic OATP transport proteins can increase the systemic exposure of simvastatin and increase the risk of myopathy and rhabdomyolysis. Reduced function can occur as the result of inhibition by interacting medicines (e.g. ciclosporin) or in patients who are carriers of the SLCO1B1 c.521T>C genotype. Patients carrying the SLCO1B1 gene allele (c.521T>C) coding for a less active OATP1B1 protein have an increased systemic exposure of simvastatin and increased risk of myopathy. The risk of high dose (80 mg) simvastatin related myopathy is about 1 % in general, without genetic testing. Based on the results of the SEARCH trial, homozygote C allele carriers (also called CC) treated with 80 mg have a 15% risk of myopathy within one year, while the risk in heterozygote C allele carriers (CT) is 1.5%. The corresponding risk is 0.3% in patients having the most common genotype (TT) (see section 5.2). Where available, genotyping for the presence of the C allele should be considered as part of the benefit-risk assessment prior to prescribing 80 mg simvastatin for individual patients and high doses avoided in those found to carry the CC genotype. However, absence of this gene upon genotyping does not exclude that myopathy can still occur. Creatine Kinase measurement Creatine Kinase (CK) should not be measured following strenuous exercise or in the presence of any plausible alternative cause of CK increase as this makes value interpretation difficult. If CK levels are significantly elevated at baseline (> 5 x ULN), levels should be re- measured within 5 to 7 days later to confirm the results. Before the treatment All patients starting therapy with simvastatin, or whose dose of simvastatin is being increased, should be advised of the risk of myopathy and told to report promptly any unexplained muscle pain, tenderness or weakness. Caution should be exercised in patients with pre-disposing factors for rhabdomyolysis. In order to establish a reference baseline value, a CK level should be measured before starting a treatment in the following situations: • Elderly (age ≥ 65 years). • Female gender. • Renal impairment. • Uncontrolled hypothyroidism. • Personal or familial history of hereditary muscular disorders. • Previous history of muscular toxicity with a statin or fibrate. • Alcohol abuse. In such situations, the risk of treatment should be considered in relation to possible benefit, and clinical monitoring is recommended. If a patient has previously experienced a muscle disorder on a fibrate or a statin, treatment with a different member of the class should only be initiated with caution. If CK levels are significantly elevated at baseline (> 5 x ULN), treatment should not be started. Whilst on treatment If muscle pain, weakness or cramps occur whilst a patient is receiving treatment with a statin, their CK levels should be measured. If these levels are found, in the absence of strenuous exercise, to be significantly elevated (>5 x ULN), treatment should be stopped. If muscular symptoms are severe and cause daily discomfort, even if CK levels are <5 x ULN, treatment discontinuation may be considered. If myopathy is suspected for any other reason, treatment should be discontinued. There have been very rare reports of an immune-mediated necrotizing myopathy (IMNM) during or after treatment with some statins. IMNM is clinically characterized by persistent proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment (see section 4.8). If symptoms resolve and CK levels return to normal, then re-introduction of the statin or introduction of an alternative statin may be considered at the lowest dose and with close monitoring. A higher rate of myopathy has been observed in patients titrated to the 80 mg dose (see section 5.1). Periodic CK measurements are recommended as they may be useful to identify subclinical cases of myopathy. However, there is no assurance that such monitoring will prevent myopathy. Therapy with simvastatin should be temporarily stopped a few days prior to elective major surgery and when any major medical or surgical condition supervenes. In few cases, statins have been reported to induce de novo or aggravate pre-existing myasthenia gravis or ocular myasthenia (see section 4.8). Simvastatin should be discontinued in case of aggravation of symptoms. Recurrences when the same or a different statin was (re-) administered have been reported. Measures to reduce the risk of myopathy caused by medicinal product interactions (see also section 4.5) The risk of myopathy and rhabdomyolysis is significantly increased by concomitant use of simvastatin with potent inhibitors of CYP3A4 (such as itraconazole, ketoconazole, posaconazole, voriconazole, erythromycin, clarithromycin, telithromycin, HIV protease inhibitors (e.g. nelfinavir), boceprevir, telaprevir, nefazodone, medicinal products containing cobicistat), as well as gemfibrozil, ciclosporin and danazol. Use of these medicinal products is contraindicated (see section 4.3). The risk of myopathy and rhabdomyolysis is also increased by concomitant use of amiodarone, amlodipine, verapamil, or diltiazem with certain doses of simvastatin (see sections 4.2 and 4.5). For patients with HoFH, this risk may be increased by concomitant use of lomitapide with simvastatin. Consequently, regarding CYP3A4 inhibitors, the use of simvastatin concomitantly with itraconazole, ketoconazole, posaconazole, voriconazole, HIV protease inhibitors (e.g. nelfinavir), boceprevir, telaprevir, erythromycin, clarithromycin, telithromycin, nefazodone, and medicinal products containing cobicistat is contraindicated (see sections 4.3 and 4.5). If treatment with potent CYP3A4 inhibitors (agents that increase AUC approximately 5 fold or greater) is unavoidable, therapy with simvastatin must be suspended (and use of an alternative statin considered) during the course of treatment. Moreover, caution should be exercised when combining simvastatin with certain other less potent CYP3A4 inhibitors: fluconazole, verapamil, diltiazem (see sections 4.2 and 4.5). Concomitant intake of grapefruit juice and simvastatin should be avoided. The use of simvastatin with gemfibrozil is contraindicated (see section 4.3). Due to the increased risk of myopathy and rhabdomyolysis, the dose of simvastatin should not exceed 10 mg daily in patients taking simvastatin with other fibrates, except fenofibrate (See sections 4.2 and 4.5.). Caution should be used when prescribing fenofibrate with simvastatin, as either agent can cause myopathy when given alone. Simvastatin must not be co-administered with systemic formulations of fusidic acid or within 7 days of stopping fusidic acid treatment. In patients where the use of systemic fusidic acid is considered essential, statin treatment should be discontinued throughout the duration of fusidic acid treatment. There have been reports of rhabdomyolysis (including some fatalities) in patients receiving fusidic acid and statins in combination (see section 4.5). The patient should be advised to seek medical advice immediately if they experience any symptoms of muscle weakness, pain or tenderness. Statin therapy may be re-introduced seven days after the last dose of fusidic acid. In exceptional circumstances, where prolonged systemic fusidic acid is needed, e.g., for the treatment of severe infections, the need for co-administration of simvastatin and fusidic acid should only be considered on a case by case basis and under close medical supervision. The combined use of simvastatin at doses higher than 20 mg daily with amiodarone, amlodipine, should be avoided. The combined use of simvastatin at doses higher than 10 mg daily with verapamil, or diltiazem should be avoided. In patients with HoFH, the combined use of simvastatin at doses higher than 40 mg daily with lomitapide must be avoided (see sections 4.2, 4.3 and 4.5). Patients taking other medicines labelled as having a moderate inhibitory effect on CYP3A4 concomitantly with simvastatin, particularly higher simvastatin doses, may have an increased risk of myopathy. When co-administering simvastatin with a moderate inhibitor of CYP3A4 (agents that increase AUC approximately 2-5 fold), a dose adjustment of simvastatin may be necessary. For certain moderate CYP3A4 inhibitors e.g. diltiazem, a maximum dose of 20 mg simvastatin is recommended (see section 4.2). Simvastatin is a substrate of the Breast Cancer Resistant Protein (BCRP) efflux transporter. Concomitant administration of products that are inhibitors of BCRP (e.g., elbasvir and grazoprevir) may lead to increased plasma concentrations of simvastatin and an increased risk of myopathy; therefore, a dose adjustment of simvastatin should be considered depending on the prescribed dose. Co-administration of elbasvir and grazoprevir with simvastatin has not been studied; however, the dose of simvastatin should not exceed 20 mg daily in patients receiving concomitant medication with products containing elbasvir or grazoprevir (see section 4.5). Rare cases of myopathy/rhabdomyolysis have been associated with concomitant administration of HMG-CoA reductase inhibitors and lipid-modifying doses (≥ 1 g/day) of niacin (nicotinic acid), either of which can cause myopathy when given alone. In a clinical trial (median follow-up 3.9 years) involving patients at high risk of cardiovascular disease and with well-controlled LDL-C levels on simvastatin 40 mg/day with or without ezetimibe 10 mg, there was no incremental benefit on cardiovascular outcomes with the addition of lipid-modifying doses (≥1 g/day) of niacin (nicotinic acid). Therefore, physicians contemplating combined therapy with simvastatin and lipid-modifying doses (≥ 1 g/day) of niacin (nicotinic acid) or products containing niacin should carefully weigh the potential benefits and risks and should carefully monitor patients for any signs and symptoms of muscle pain, tenderness, or weakness, particularly during the initial months of therapy and when the dose of either medicinal product is increased. In addition, in this trial, the incidence of myopathy was approximately 0.24% for Chinese patients on simvastatin 40 mg or ezetimibe/simvastatin 10/40 mg compared with 1.24% for Chinese patients on simvastatin 40 mg or ezetimibe/simvastatin 10/40 mg co-administered with modified-release nicotinic acid/laropiprant 2000 mg/40 mg. While the only Asian population assessed in this clinical trial was Chinese, because the incidence of myopathy is higher in Chinese than in non-Chinese patients, co- administration of simvastatin with lipid-modifying doses (≥1 g/day) of niacin (nicotinic acid) is not recommended in Asian patients. Acipimox is structurally related to niacin. Although acipimox was not studied, the risk for muscle related toxic effects may be similar to niacin. Daptomycin Cases of myopathy and/or rhabdomyolysis have been reported with HMG-CoA reductase inhibitors (e.g. simvastatin) co-administered with daptomycin. Caution should be used when prescribing HMG- CoA reductase inhibitors with daptomycin, as either agent can cause myopathy and/or rhabdomyolysis when given alone. Consideration should be given to temporarily suspend simvastatin in patients using daptomycin unless the benefits of concomitant administration outweigh the risk. Consult the prescribing information of daptomycin to obtain further information about this potential interaction with HMG-CoA reductase inhibitors (e.g. simvastatin) and for further guidance related to monitoring. (See section 4.5.). Hepatic effects In clinical studies, persistent increases (to > 3 x ULN) in serum transaminases have occurred in a few adult patients who received simvastatin. When simvastatin was interrupted or discontinued in these patients, the transaminase levels usually fell slowly to pre-treatment levels. It is recommended that liver function tests be performed before treatment begins and thereafter when clinically indicated. Patients titrated to the 80 mg dose should receive an additional test prior to titration, 3 months after titration to the 80 mg dose, and periodically thereafter (e.g., semi-annually) for the first year of treatment. Special attention should be paid to patients who develop elevated serum transaminase levels, and in these patients, measurements should be repeated promptly and then performed more frequently. If the transaminase levels show evidence of progression, particularly if they rise to 3 x ULN and are persistent, simvastatin should be discontinued. Note that ALT may emanate from muscle, therefore ALT rising with CK may indicate myopathy (see above Myopathy/Rhabdomyolysis). There have been rare post-marketing reports of fatal and non-fatal hepatic failure in patients taking statins, including simvastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinaemia or jaundice occurs during treatment with simvastatin, promptly interrupt therapy. If an alternate etiology is not found, do not restart simvastatin. The product should be used with caution in patients who consume substantial quantities of alcohol. As with other lipid-lowering agents, moderate (<3 x ULN) elevations of serum transaminases have been reported following therapy with simvastatin. These changes appeared soon after initiation of therapy with simvastatin, were often transient, were not accompanied by any symptoms and interruption of treatment was not required. Diabetes Mellitus Some evidence suggests that statins as a class raise blood glucose and in some patients at high risk of future diabetes, may produce a level of hyperglycaemia where formal diabetes care is appropriate. This risk, however, is outweighed by the reduction in vascular risk with statins and therefore should not be a reason for stopping statin treatment. Patients at risk (fasting glucose 5.6 to 6.9 mmol/L, BMI > 30 kg/m2, raised triglycerides, hypertension) should be monitored both clinically and biochemically according to national guidelines. Interstitial lung disease Exceptional cases of interstitial lung disease have been reported with some statins, especially with long term therapy (see section 4.8). Presenting features can include dyspnoea, nonproductive cough and deterioration in general health (fatigue, weight loss and fever). If it is suspected a patient has developed interstitial lung disease, statin therapy should be discontinued. Excipient(s) Lactose Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicine.
Effects on Driving
4.7 Effects on ability to drive and use machines Simvastatin has no or negligible influence on the ability to drive and use machines. However, when driving vehicles or operating machines, it should be taken into account that dizziness has been reported rarely in post-marketing experiences.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| 09/03/1999 | ליפידים | ATORVASTATIN, CERIVASTATIN, FLUVASTATIN, LOVASTATIN, PRAVASTATIN, SIMVASTATIN, ROSUVASTATIN | היפרליפידמיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
09/03/1999
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
07.03.22 - עלון לצרכן אנגלית 07.03.22 - עלון לצרכן עברית 07.03.22 - עלון לצרכן ערבית 29.01.24 - עלון לצרכן עברית 04.04.24 - עלון לצרכן אנגלית 04.04.24 - עלון לצרכן עברית 04.04.24 - עלון לצרכן ערבית 18.04.12 - החמרה לעלון 26.11.20 - החמרה לעלון 11.04.21 - החמרה לעלון 20.02.22 - החמרה לעלון 28.11.13 - החמרה לעלון 29.01.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
סימבסטאטין טבע ® 40 מ"ג