Quest for the right Drug
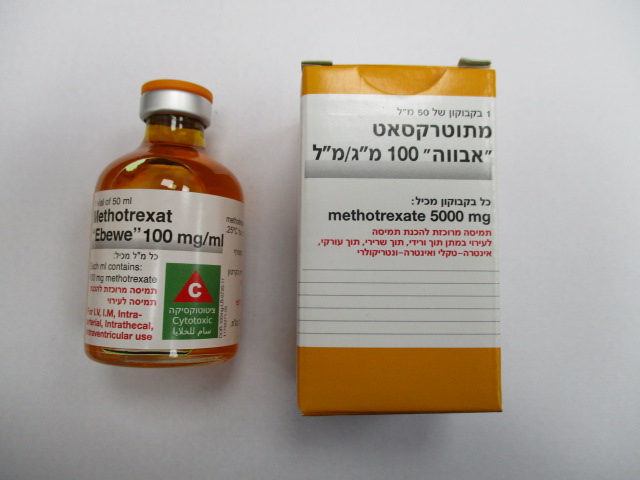
מתוטרקסאט " אבווה " 100 מ"ג/מ"ל METHOTREXAT "EBEWE" 100 MG/ML (METHOTREXATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-עורקי, תוך-ורידי, תוך חדרי, תוך-שדרתי : I.M, INTRA-ARTERIAL, I.V, INTRA VENTRICULAR, INTRATHECAL
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects In general, the incidence and severity of undesirable effects are dependent on the dose and duration of methotrexate treatment. Since serious adverse reactions can, however, occur even at a low dose and at any time during therapy, patients should be closely and frequently monitored by the doctor. Most undesirable effects are reversible if recognised soon enough. However, some of the serious adverse reactions listed below, can in very rare cases lead to sudden death. If undesirable effects appear, the dosage should be reduced as necessary according to their severity and intensity, or the therapy should be discontinued and appropriate countermeasures taken (see section 4.9). If methotrexate therapy is continued, this should be done with caution and after carefully evaluating the need for the therapy. The patients must be closely monitored for the possible recurrence of toxicity. Myelosuppression and mucositis are generally the dose-limiting toxic effects. Their severity depends on the dosage, method and duration of methotrexate administration. Mucositis appears approximately 3–7 days after methotrexate administration, while leukopenia and thrombocytopenia appear 5–13 days after methotrexate administration. Myelosuppression and mucositis are generally reversible within 14 days in patients with no impairment to the elimination mechanisms. The most commonly reported undesirable effects include thrombocytopenia, leukopenia, headache, vertigo, coughing, anorexia, diarrhoea, abdominal pain, nausea, vomiting, inflammation, and ulcerations of the mucosa in the mouth and the throat (especially in the first 24–48 hours after administering methotrexate), increased liver enzymes and bilirubin, alopecia, reduced creatinine clearance, fatigue and malaise. Ulcerations of the oral mucosa are usually the first clinical signs of toxicity. The following frequencies are used for classifying undesirable effects: Very common: ≥ 1/10 Common: ≥1/100, <1/10 Uncommon: ≥1/1,000, <1/100 Rare: ≥1/10,000, <1/1,000 Very rare: <1/10,000 Not known (cannot be estimated from the available data) Infections and infestations Common: herpes zoster Uncommon: opportunistic infections that may have a fatal outcome Rare: sepsis (including a fatal outcome) Very rare: herpes simplex, hepatitis, cryptococcosis, histoplasmosis, cytomegalovirus infections (including pneumonia), disseminated herpes simplex, nocardiosis, pneumocystis jirovecii pneumonia* Not known: pneumonia, reactivation of hepatitis B infection, exacerbation of hepatitis C infection Neoplasms benign, malignant and unspecified (including cysts and polyps) Uncommon: malignant lymphoma* Very rare: tumour lysis syndrome* Blood and lymphatic system disorders* Very common: leukopenia, thrombocytopenia Common: anaemia, pancytopenia, bone marrow suppression, agranulocytosis Rare: megaloblastic anaemia Very rare: aplastic anaemia, eosinophilia, neutropenia, lymphadenopathy (partially reversible), and lymphoproliferative disorders (partially reversible) Immune system disorders Uncommon: allergic reactions up to and including anaphylactic shock, immunosuppression Very rare: hypogammaglobulinaemia Metabolism and nutrition disorders Uncommon: diabetes mellitus Psychiatric disorders Uncommon: depression Rare: mood swings, transient perception disorders Nervous system disorders Very common: headaches, dizziness Common: drowsiness, paraesthesia Uncommon: hemiparesis, confusion, seizures (in parenteral administration), leukoencephalopathy/encephalopathy* (in parenteral administration) Rare: paresis, speech disorders including dysarthria and aphasia, myelopathy (after lumbar application) Very rare: muscle weakness and pain in the extremities, dysgeusia (metallic taste), acute aseptic meningitis (paralysis, vomiting), cranial nerve syndrome, hypoaesthesia Not known: neurotoxicity, arachnoiditis, paraplegia, stupor, ataxia, dementia, increase in cerebrospinal fluid pressure The intravenous use of methotrexate may lead to acute encephalitis and acute encephalopathy with fatal outcome. Eye disorders Common: conjunctivitis Rare: visual disturbances (partially serious), severe retinal vein thrombosis Very rare: periorbital oedema, blepharitis, epiphora, photophobia, temporary blindness, loss of vision. Cardiac disorders Very rare: pericarditis, pericardial effusion, pericardial tamponade Vascular disorders Uncommon: vasculitis, allergic vasculitis Rare: hypotension, thromboembolic events (including arterial and cerebral thrombosis, thrombophlebitis, deep vein thrombosis) Respiratory, thoracic and mediastinal disorders* Very common: cough Common: pulmonary complications due to interstitial alveolitis/pneumonia and the fatalities caused by them (regardless of the dose or duration of treatment with methotrexate) Uncommon: pulmonary fibrosis, pleural effusion Rare: pharyngitis, respiratory arrest, pulmonary embolism Very rare: chronic interstitial pulmonary disease, asthma-like reactions such as coughing, dyspnoea and pathological changes in lung function tests Not known: chest pain, hypoxia, pulmonary alveolar bleeding (reported in use of methotrexate in rheumatic and related indications) Gastrointestinal disorders* Very common: anorexia, diarrhoea (especially in the first 24–48 hours after using methotrexate), abdominal pains, nausea, vomiting, inflammation and ulceration of the mucosa in the mouth and the throat (especially in the first 24–48 hours after using methotrexate) Uncommon: gastrointestinal ulcerations and bleeding, pancreatitis Rare: enteritis, gingivitis, melaena Very rare: haematemesis Not known: non-infectious peritonitis, toxic megacolon, colon perforation, glossitis Hepatobiliary disorders* Very common: increase in liver enzymes (ALAT [GPT], ASAT [GOT]), alkaline phosphatase and bilirubin Uncommon: hepatotoxicity, hepatic steatosis, chronic liver fibrosis and liver cirrhosis, serum albumin decrease Rare: acute hepatitis Very rare: acute hepatic necrosis, acute hepatolysis, hepatic failure Skin and subcutaneous tissue disorders* Very common: alopecia Common: exanthema, erythema, pruritus, photosensitivity, skin ulcerations Uncommon: severe toxic manifestations: herpetiform skin eruptions, Stevens-Johnson syndrome*, toxic epidermal necrolysis (Lyell's syndrome)*, urticaria, increased skin pigmentation, nodulosis, painful erosions of psoriatic plaques, impaired wound healing Rare: acne, petechiae, ecchymosis, erythema multiforme, erythematous skin rashes, increased pigment changes of the nails, onycholysis Very rare: furunculosis, telangiectasia, acute paronychia Not known: Drug Rash with Eosinophilia and Systemic Symptoms (DRESS), exfoliative dermatitis Musculoskeletal and connective tissue disorders Uncommon: arthralgia, myalgia and osteoporosis Rare: stress fracture Not known: Osteonecrosis of the jaw (secondary to lymphoproliferative diseases) Renal and urinary disorders* Very common: decreased creatinine clearance Uncommon: nephropathy, kidney failure, cystitis with ulcerations (eventually with haematuria), bladder voiding disorders, dysuria, oliguria, anuria Rare: hyperuricemia, increased serum urea and creatinine concentrations, azotaemia Very rare: haematuria, proteinuria Pregnancy, puerperium and perinatal conditions Uncommon: foetal malformations Rare: abortion Very rare: foetal death Reproductive system and breast disorders Uncommon: vaginal ulcerations and inflammations Rare: transient oligospermia, transient irregular menstrual cycles Very rare: impaired oogenesis/spermatogenesis*, infertility*, menstrual disorders , loss of libido, impotence, vaginal discharge, gynecomastia Not known: urogenital dysfunction General disorders and administration site reactions Very common: exhaustion, malaise Uncommon: pyrexia, in intramuscular administration of methotrexate, local adverse reactions (burning sensation) or damage (sterile abscess formation, destruction of adipose tissue) may appear at the injection site. Not known: injection site necrosis, chills, oedema * For information on severe undesirable effects see section 4.4. Adverse reactions to intrathecal administration of methotrexate CNS toxicity may occur after intrathecal administration of methotrexate and may manifest in different forms: - acute chemical arachnoiditis (inflammation of the arachnoid membrane), which can manifest as headache, back pain, neck stiffness and fever, for example; - subacute myelopathy, characterised by e.g. paraparesis/paraplegia (with the involvement of one or more spinal nerve roots); - chronic leukoencephalopathy, which can manifest as confusion, irritability, sleepiness, ataxia, dementia, convulsions and coma, for example. This CNS toxicity may advance up to and including death. There are indications that the combined use of cranial irradiation and intrathecal methotrexate increases the incidence of leukoencephalopathy. Intrathecal administration of methotrexate should be followed by close monitoring for signs of neurotoxicity (meningitis, transient or persistent paralysis, encephalopathy). The intrathecal and intravenous use of methotrexate may lead to acute encephalitis and acute encephalopathy with fatal outcome. There have been reports of patients with periventricular CNS lymphoma who developed cerebral herniation after intrathecal application of methotrexate. Adverse reactions to intramuscular administration of methotrexate After intramuscular use of methotrexate, local adverse reactions (such as a burning sensation) or tissue damage (such as sterile abscess formation, adipose tissue necrosis) can appear. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il/

שימוש לפי פנקס קופ''ח כללית 1994
Leukemias, non-hodgkin's lymphomas, breast, head and lung carcinoma, choriocarcinoma, osteogenic sarcoma. Severe psoriasis, rheumatoid arthritis unresponsive to conventional therapy, mycosis fungoides
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
