Quest for the right Drug
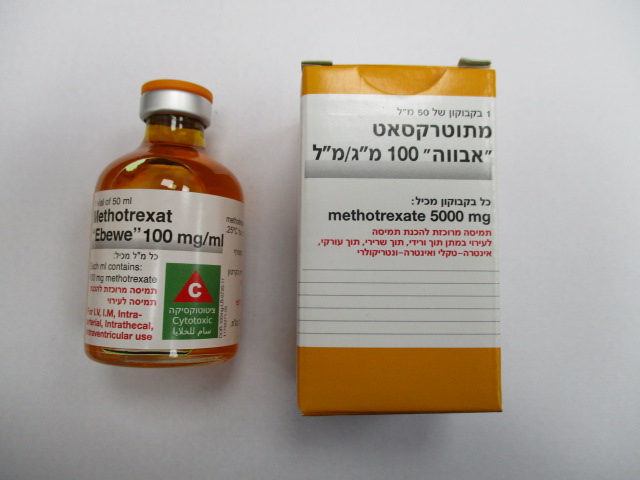
מתוטרקסאט " אבווה " 100 מ"ג/מ"ל METHOTREXAT "EBEWE" 100 MG/ML (METHOTREXATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-עורקי, תוך-ורידי, תוך חדרי, תוך-שדרתי : I.M, INTRA-ARTERIAL, I.V, INTRA VENTRICULAR, INTRATHECAL
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Interactions : אינטראקציות
4.5 Interaction with other medicinal products and other forms of interaction
The use of nitrous oxide ("laughing gas") potentiates the effect of methotrexate on folate metabolism, yielding increased toxicity such as severe, unpredictable myelosuppression, stomatitis and increased severe unpredictable neurotoxicity with intrathecal administration.
Whilst this effect can be alleviated by administering calcium folinate, the concomitant use of methotrexate and nitrous oxide should be avoided.
Concomitant administration of L-asparaginase has an antagonistic effect on methotrexate.
Disease-modifying antirheumatic drugs (DMARD) and non-steroidal anti-inflammatory drugs (NSAIDs) should not be administered before or during high-dose methotrexate therapy.
Concomitant use of certain NSAIDs and high-dose methotrexate therapy led to increased and persistent methotrexate serum levels, with some fatal outcomes due to severe haematological (bone marrow suppression and aplastic anaemia) and gastrointestinal toxicity.
In animal studies, NSAIDs including salicylic acid have been found to decrease the tubular secretion of methotrexate and thus to an increase of its toxicity due to increased methotrexate levels.Therefore, NSAIDs and low-dose methotrexate should only be used concomitantly with caution. In the presence of risk factors, such as an impaired renal function (even in cases of threshold values), the concomitant administration of non-steroidal anti-inflammatory drugs is not advised.
Increased methotrexate toxicity has not been investigated when methotrexate is used concomitantly with other basic therapeutic drugs (e.g. gold compounds, penicillamine, hydroxychloroquine, sulphasalazine, azathioprine, cyclosporine), and a potentiation of the toxic effects of methotrexate cannot be ruled out.
The concomitant use of proton pump inhibitors (omeprazole, pantoprazole, or lansoprazole) may lead to a delay in or inhibition of the renal elimination of methotrexate and thus to increased methotrexate plasma levels, with clinical signs and symptoms of methotrexate toxicity.
Concomitant administration of proton pump inhibitors with high-dose methotrexate should therefore be avoided, and especially in patients with impaired renal function.
Hepatotoxicity may be increased with regular consumption of alcohol or if hepatotoxic medicinal products are administered, e.g. azathioprine, leflunomide, retinoids and sulphasalazine.
Patients who take additional hepatotoxic medicinal products should be closely monitored. Alcohol consumption should be avoided during treatment with methotrexate.
Due to the displacement of methotrexate from plasma protein binding, the following medicinal products may increase the bioavailability of methotrexate (indirect dose increase), causing an increased toxicity of methotrexate: amidopyrine derivatives, para-aminobenzoic acid, barbiturates, doxorubicin, oral contraceptives, phenylbutazone, phenytoin, probenecid, salicylates, sulphonamides, tetracyclines, tranquillisers, sulfonylurea, penicillins, pristinamycin, and chloramphenicol. Concomitant use of methotrexate should therefore be closely monitored.
A decrease in tubular secretion with a consequent increase of methotrexate toxicity, especially at low doses, can be caused by the following medicinal products: para-aminohippuric acid, NSAIDs, probenecid, salicylate, sulphonamides and other weak organic acids. Concomitant use of methotrexate should therefore be closely monitored.
Penicillins and sulphonamides can reduce the renal clearance of methotrexate in individual cases, which may result in increased serum concentrations of methotrexate with simultaneous haematological and gastrointestinal toxicity.
Tubular renal secretion is reduced by ciprofloxacin. Concomitant use of methotrexate with this medicinal product should be monitored carefully.
Oral antibiotics such as tetracyclines, chloramphenicol, and non-absorbable broad-spectrum antibiotics can reduce the intestinal resorption of methotrexate, or interfere with the enterohepatic circulation, by inhibition of the intestinal flora or suppression of the bacterial metabolism of methotrexate.
In cases of (pre-)treatment with medicinal products which may have adverse effects on the bone marrow (e.g. aminopyridine derivatives, chloramphenicol, phenytoin, pyrimethamine, sulphonamides, trimethoprim/sulfamethoxazole, cytostatics), the possibility of severe impairment of haematopoiesis should be taken into account during methotrexate therapy.
Concomitant use of medicinal products that cause a folate deficiency (e.g. sulphonamides, trimethoprim/sulfamethoxazole) may increase methotrexate toxicity. Particular caution should therefore also be exercised in the presence of existing folic acid deficiency. On the other hand, concomitant use of folinic acid-based medicinal products as well as vitamin supplements which contain folic acid or its derivatives, may impair methotrexate efficacy.
Although the combination of methotrexate and sulphasalazine may potentiate the methotrexate effect because of the inhibition of the folic acid synthesis by sulphasalazine — and therefore increased side effects — these were observed in the course of several patient trials only in rare isolated cases.
Methotrexate can reduce clearance of theophylline.Theophylline levels must therefore be monitored during concomitant treatment with methotrexate.
Excessive consumption of beverages containing caffeine or theophylline (coffee, soft drinks containing caffeine, black tea) should be avoided during methotrexate therapy, since the efficacy of methotrexate may be reduced due to possible interaction between methotrexate and methylxanthines at the adenosine receptors.
The combined administration of methotrexate and leflunomide may increase the risk of pancytopenia.
Concomitant use of methotrexate and mercaptopurine may lead to increased plasma levels of mercaptopurine. Therefore, concomitant use may require dose adjustment.
In the context of concomitant administration of triamterene and methotrexate, cases of bone marrow suppression and decreased folate levels have been described.
Radiotherapy during the administration of methotrexate may increase the risk of soft tissue or bone necrosis.
Cholestyramine may increase the non-renal elimination of methotrexate by interrupting the enterohepatic circulation.
In concomitant use of erythrocyte concentrates and methotrexate special monitoring of the patient is required. Increased toxicity due to prolonged high serum concentrations of methotrexate may occur in patients who receive blood transfusions for 24 hours after methotrexate infusions.
In isolated cases, corticosteroids caused disseminated herpes zoster in patients with herpes zoster or post-herpetic neuralgia when methotrexate was administered concomitantly.
High doses of calcium folinate may reduce the efficacy of intrathecally administered methotrexate.
Anaesthetics based on nitric oxide potentiate the effect of methotrexate on folic acid metabolism and cause increased toxicity, such as severe, unpredictable myelosuppression, stomatitis, and neurotoxicity in intrathecal use. This can be reduced by the administration of calcium folinate.
Pyrimethamine or co-trimoxazole used in combination with methotrexate may cause pancytopenia, probably due to the additive inhibition of dihydrofolate reductase by these substances and methotrexate. See above for interactions between sulphonamides and methotrexate.
Regular alcohol consumption and administration of additional hepatotoxic medicinal products increase the probability of hepatotoxic adverse effects of methotrexate.
Administration of additional haematotoxic medicinal products (e.g. metamizole) increases the probability of severe haematotoxic effects of methotrexate.
The pharmacokinetic interactions between methotrexate, anticonvulsants (reduced methotrexate blood levels), and 5-fluorouracil (increased half-life of 5-fluorouracil) must be taken into consideration.
Particularly in the event of orthopaedic surgery, where the risk of infection is very high, a combination of methotrexate with immunomodulatory agents must be used with caution.
Delayed methotrexate clearance should be taken into account in combination with other cytostatic agents.
A decrease in phenytoin plasma levels has been observed in patients with acute lymphoblastic leukaemia during induction therapy that included high-dose methotrexate with calcium folinate rescue in addition to prednisone, vincristine and 6-mercaptopurine.
The administration of procarbazine during high-dose methotrexate therapy increases the risk of renal impairment.
Concomitant therapy with intravenous cytarabine and intrathecal methotrexate can increase the risk of severe neurological undesirable effects ranging from headache to paralysis, coma and stroke-like episodes.
An increase in nephrotoxicity may occur in the combination of high-dose methotrexate with a potentially nephrotoxic chemotherapeutic agent, e.g. cisplatin.
On account of its possible effect on the immune system, methotrexate can lead to false vaccine and test results (immunological procedures to evaluate the immune reaction).
During methotrexate therapy concomitant vaccination with live vaccines must not be carried out (see sections 4.3 and 4.4).
Methotrexate may increase the effects of coumarin-like oral anticoagulants (acenocoumarol, phenprocoumon), resulting in increased prothrombin time due to the decreased breakdown of coumarin derivatives.
Concomitant administration of levetiracetam and methotrexate has been reported to decrease methotrexate clearance, resulting in increased/prolonged blood methotrexate concentration to potentially toxic levels. Blood methotrexate and levetiracetam levels should be carefully monitored in patients treated concomitantly with the two medicinal products.

שימוש לפי פנקס קופ''ח כללית 1994
Leukemias, non-hodgkin's lymphomas, breast, head and lung carcinoma, choriocarcinoma, osteogenic sarcoma. Severe psoriasis, rheumatoid arthritis unresponsive to conventional therapy, mycosis fungoides
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
