Quest for the right Drug
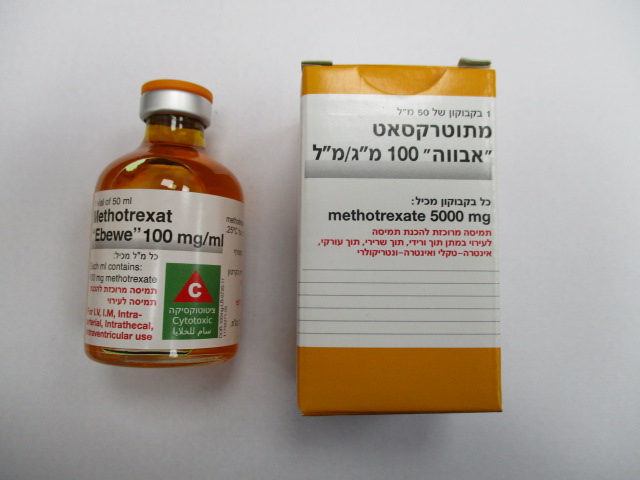
מתוטרקסאט " אבווה " 100 מ"ג/מ"ל METHOTREXAT "EBEWE" 100 MG/ML (METHOTREXATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-עורקי, תוך-ורידי, תוך חדרי, תוך-שדרתי : I.M, INTRA-ARTERIAL, I.V, INTRA VENTRICULAR, INTRATHECAL
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, antimetabolites, folic acid analogues, ATC code: L01BA01 Mechanism of action As a folic acid analogue, methotrexate is classified as an antimetabolite. It competitively inhibits the enzyme dihydrofolate reductase. This enzyme has to reduce dihydrofolic acid to tetrahydrofolic acid, before it can be used for the transport of a carbon group in the synthesis of purine nucleotides and thymidylates. Thus, methotrexate actively interferes with DNA synthesis and repair and cell replication. Clinical efficacy and safety Highly proliferating tissues such as malignant cells, bone marrow, foetal cells, skin epithelium and mucosa are generally more susceptible to this effect of methotrexate. Since cell proliferation is usually higher in malignant growths than in normal tissue, methotrexate may have a lasting effect on malignant growth without causing irreversible damage to normal tissue.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption 100% in intravenous and intramuscular administration. After oral administration, methotrexate is absorbed from the gastrointestinal tract. When administered in low doses (7.5 mg/m2 to 80 mg/m2 body surface area), methotrexate has a mean bioavailability of approximately 70%, although considerable inter- and intra-individual variations are possible (25–100%). Peak serum concentration is achieved within 1–2 hours. Subcutaneous, intravenous and intramuscular administration demonstrated similar bioavailability. Approximately 50% of methotrexate is bound to serum proteins. After distribution, high concentrations can be found in the form of polyglutamates, particularly in the liver, kidneys and spleen, which can be retained for weeks or months. After intrathecal administration of methotrexate, absorption into the plasma component is slow and results in a possibly toxic plasma concentration being maintained over a longer period. Distribution After intravenous application the initial volume of distribution is approximately 0.18 l/kg (18% of the body weight), and 0.4 to 0.8 l/kg (40% to 80% of the body weight) under steady state conditions. Methotrexate competes with reduced folates for the active carrier-mediated cell membrane transport. In serum concentrations of more than 100 µmol/l the intracellular concentration is predominantly achieved by passive diffusion. The plasma protein binding of methotrexate is approx. 50%. The highest concentrations of methotrexate are found in the kidneys, the gallbladder, the spleen, the liver, the skin and in the small and large intestine. Methotrexate slowly enters into the ‘third space’ (pleural effusions and ascites) and is only released slowly, which may cause an increase in toxicity. In oral or parenteral administration in therapeutic doses methotrexate does not pass the blood–cerebrospinal fluid barrier. Only after intrathecal administration or high-dose therapy were therapeutically effective doses found in the cerebrospinal fluid. When administered in small doses, methotrexate passes into the cerebrospinal fluid in minimal amounts only; at high doses (300 mg/kg body weight), concentrations of between 4 and 7 μg/ml have been measured in the cerebrospinal fluid. The mean terminal half-life is 6–7 hours, with considerable variation (3–17 hours). In patients with a third space (pleural effusion, ascites), the half-life can be increased by up to four-fold. Biotransformation After absorption, methotrexate undergoes hepatic and intracellular biotransformation to polyglutamates, which can be transformed back into methotrexate with hydrolase enzymes. These polyglutamates act as inhibitors of dihydrofolate reductase and thymidylate synthetase. Small amounts of methotrexate polyglutamate may remain in the tissues for a longer period. The retention and the prolonged duration of effect of these active metabolites varies by cell, tissue and tumour type. In usual dosages, a small amount is metabolised to 7-hydroxymethotrexate, while in higher doses, the accumulation of this metabolite may be significant. Water solubility of 7-hydroxymethotrexate is three to five times lower than of the original compound. The terminal half-life is approx. 3‒10 hours in the administration of low methotrexate doses (30 mg/m2 BSA). The terminal half-life in high-dose therapy is 8–15 hours. Elimination Methotrexate elimination is predominantly renal, by glomerular filtration, and active secretion in proximal tubules. It depends on the dose and the administration form. After intravenous administration, 80‒90% of the administered dose is eliminated unchanged via the urine within 24‒30 hours. Biliary elimination is limited, reaching a maximum of 10% of the administered dose. Methotrexate undergoes pronounced enterohepatic circulation, so that a maximum of 10% of the administered dose is eliminated through faeces. After intravenous injection, methotrexate undergoes a distribution phase lasting a few minutes. Methotrexate is eliminated during the second, 12- to 24-hour phase with a plasma half-life of 2 to 3 hours, and during the third phase with a plasma half-life of 12 to 24 hours. In impaired renal function, delayed elimination must be expected, which may lead to severe undesirable effects. The correlation between methotrexate clearance and endogenous creatinine clearance was found to be good. Elimination restrictions in hepatic impairment are currently not known. Methotrexate passes the placental barrier in rats and monkeys.

שימוש לפי פנקס קופ''ח כללית 1994
Leukemias, non-hodgkin's lymphomas, breast, head and lung carcinoma, choriocarcinoma, osteogenic sarcoma. Severe psoriasis, rheumatoid arthritis unresponsive to conventional therapy, mycosis fungoides
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
