Quest for the right Drug
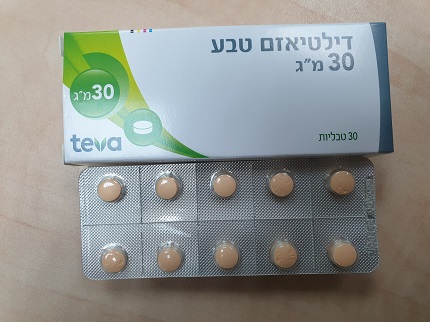
דילטיאזם טבע 30 מ"ג DILTIAZEM TEVA 30 MG (DILTIAZEM HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
Adverse Reactions Adverse reactions are generally not serious and rarely require discontinuation of therapy or dosage adjustment. In clinical trials of diltiazem and diltiazem SR formulations involving over 3200 patients, the most common events (i.e, greater than 1%) were edema (4.6%), headache (4.9% ), dizziness (3.5%), asthenia (2.7%), first degree AV block (2.2%), bradycardia (1.6%), flushing (1.5%), nausea (1.4%), rash (1.3%), dyspepsia (1.2%), palpitations, lower limb oedema, constipation, gastric pain, malaise and erythema. In addition, the following events were reported infrequently (less than 1%) in angina or hypertension trials. Cardiovascular System Peripheral edema, hypotension, palpitations, syncope, AV block (1st, 2nd or 3rd degree), bradycardia, congestive heart failure, arrhythmia (unspecified), pulmonary edema, angina, tachycardia, abnormal ECG, ventricular extrasystoles. Central Nervous System Dizziness, lightheadedness, nervousness, sleep disturbances, psychiatric disturbances (depression, amnesia, paranoia, psychosis, hallucinations, personality changes), headache, weakness, shakiness, jitteriness, paresthesia, somnolence, asthenia, insomnia, abnormal dreams, tinnitus, tremor/hand tremor. Gastrointestinal Anorexia, nausea, diarrhea, constipation, abdominal discomfort, abdominal cramps, dyspepsia, disgeusia, hepatic enzyme increase (AST, ALT, LDH, ALP), vomiting, dry mouth, thirst, weight increase.. Dermatological Dermatitis, rash, pruritus, urticaria, hair loss, photosensitivity (including lichenoid keratosis at sun exposed skin areas),,erythema multiforme, Stevens-Johnson syndrome. Hematopoietic Leukopenia, petechiae, ecchymosis, purpura, bruising, hematoma. Other Flushing, nasal congestion, chest congestion, sinusitis, rhinitis, gingival hyperplasia, micturition disorders (e.g. polyuria, nocturia, dysuria), sexual difficulties, impotence, shortness of breath, dyspnea, wheezing, joint stiffness, pain, arthritis, gynecomastia, hyperglycemia, hyperuricemia, weight gain, vomiting epistaxis, anorexia, muscle cramps, CPK increase, osteoarticular pain. In addition to the adverse effects listed above, the following have been reported: gait abnormality, tremor, amblyopia, eye irritation, bundle branch block, and amnesia. The following postmarketing events have been reported infrequently in patients receiving diltiazem: mood changes (including deprerssion), sino-atrial block, congestive heart failure, photosensitivity, hepatitis, musculo-cutaneous reactions such as simple erythema or occasionally desquamative erythema with or without fever, angioneurotic edema, symptoms of vasodilation (such as flushing, lower limb edema, sweating), alopecia, erythema multiforme (including rare cases of Steven- Johnson's syndrome), exfoliative dermatitis, extrapyramidal symptoms, acute generalized exanthematous pustular dermatitis, orthostatic hypotension, malaise, gastric pain, gingival hyperplasia, hemolytic anemia, increased bleeding time, leukopenia, purpura, retinopathy and thrombocytopenia. Very rare cases of toxic epidermal necrolysis have also been reported In addition, events such as myocardial infarction have been observed which are not readily distinguishable from the natural history of the disease in these patients. A number of well-documented cases of generalized rash, characterized as leukocyloclastic vasculitis, have been reported. However, a definitive cause and effect relationship between these events and diltiazem therapy is yet to be established. Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form http://forms.gov.il/globaldata/getsequence/getsequence.aspx?formType=AdversEffec tMedic@moh.gov.il Precautions Diltiazem is extensively metabolized by the liver and excreted by the kidneys and in bile. As with any drug given over prolonged periods, laboratory parameters of renal and hepatic function should be monitored at regular intervals. Dermatological Events Dermatological events may be transient and may disappear despite continued use of diltiazem. However, skin eruptions progressing to erythema multiforme and/or exfoliative dermatitis have also been infrequently reported. Should a dermatologic reaction persist, the drug should be discontinued. Use in Diabetics Diltiazem should be used with caution in patients suffering from diabetes. Like other calcium channel blockers, diltiazem influences insulin secretion and its peripheral action by inhibiting calcium influx into cells. In one study, increases in fasting and peak glucose levels were observed after 2 to 6 months of diltiazem administration. Other Effects Calcium channel blocking agents, such as diltiazem, may be associated with mood changes, including depression. Like other calcium channel antagonists, diltiazem has an inhibitory effect on intestinal motility. Therefore, it should be used with caution in patients at risk to develop an intestinal obstruction. Abrupt Withdrawal The sudden withdrawal of dilitazem has been associated with sever angina in anginal paqtients. Effects on Ability to Drive and Use Machines Diltiazem may cause adverse reactions such as dizziness, which may impair patients' ability to drive or operate machinery to a varying extent depending on the dosage and individual susceptibility. Therefore, patients should not drive or operate machinery if affected. Drug Interactions Notes: Due to the potential for additive effects, caution and careful titration are warranted in patients receiving diltiazem concomitantly with other agents known to affect cardiac contractility and/or conduction. Diltiazem is extensively metabolised by CYP3A4, and as a result serum levels of diltiazem may be: • Increased by concomitant usage of CYP3A4 inhibitors such as H2 antagonists (e.g. cimetidine, ranitidine) and protease inhibitors (e.g. atazanavir, ritonavir) • Decreased by concomitant usage of CYP3A4 inducers such as barbiturates (phenobarbital, primidone), phenytoin and rifampicin. Diltiazem is also an inhibitor of CYP3A4, and may therefore increase serum levels of CYP3A4 substrates such as benzodiazepines (especially midazolam and triazolam), carbamazepine, ciclosporin, cilostazol, ivabradine, statins (simvastatin, atorvastatin, lovastatin), sirolimus, tacrolimus, erythromycin and theophylline. Care should be exercised in patients taking these drugs. Concomitant use of diltiazem with cilostazol should be avoided. Concomitant use with ivabradine is contraindicated due to the additional heart rate lowering effect of diltiazem to ivabradine (see section “Contraindications”). β -adrenergic Blockers/Calcium Channel Blockers: β-adrenergic blockers Diltiazem/β and calcium channel blockers both have negative chronotropic and inotropic effects. These combinations are advantageous in some patients (e.g. hypertension, angina); however, they may be a problem in others (e.g. sinoatrial disease, conduction defects, heart failure) (see Warnings). Combination therapy can, however adversely affect cardiac function, because of the depressant effects on myocardial contractility or AV conduction. Therefore, if combined therapy is used, closely monitor the patient and reassess continued use periodically. Patients with pre-existing conduction defects should not receive the combination of diltiazem and beta-blockers. Administration of diltiazem concomitantly with propranolol in five normal volunteers resulted in increased propranolol levels in all subjects and bioavailability of propranolol was increased by approximately 50%. If combination therapy is initiated or withdrawn in conjunction with propranolol, an adjustment in the propranolol dose may be warranted. In contrast, there appears to be no effect on the pharmacokinetics of atenolol, a renally cleared drug. In view of the known pharmacodynamic interactions between these classes of drugs, this effect may be of clinical relevance. Dilitazem/Drugs which May Induce Bradycardia/Other Antiarrhythmic Drugs (e.g. Amiodarone): There may be an additive effect (increased depression of cardiac conduction with risk of bradycardia and AV block) when diltiazem is prescribed with drugs which may induce bradycardia or other anti-arrhythmic drugs (e.g. amiodarone and beta blockers). Amiodarone should be used with caution with diltiazem particularly if there is suspicion of underlying dysfunction of the sinus node, such as bradycardia or sick sinus syndrome or if there is partial A-V block. Sinus arrest and a life-threatening low cardiac output state developed when amiodarone was added to a regimen of diltiazem and a diuretic. It has been suggested that diltiazem and amiodarone have additive adverse effects on sinus node function and myocardial contractility. There is an increased risk of bradycardia with this combination. Caution is required when amiodarone is combined with diltiazem, particularly in the elderly and when high doses are used. Diltiazem/Rifampicin: There is a risk of decreased diltiazem plasma levels after initiating therapy with rifampicin. The patient should be carefully monitored when initiating or discontinuing rifampicin treatment. Diltiazem/Benzodiazepines (e.g. Midazolam, Triazolam, Diazepam): Diltiazem significantly increases plasma concentration of midazolam and triazolam and prolongs their half-life. Special care should be taken when prescribing short-acting benzodiazepines metabolised by the CYP3A4 pathway in patients using diltiazem. Diazepam has been reported to cause a significant decrease in diltiazem plasma levels. The average decrease in diltiazem concentration was between 20 and 30%. Three out of eight patients showed decreases which were greater than 50%. Diltiazem/Buspirone: In 9 healthy subjects, diltiazem significantly increased the mean buspirone AUC 5.5-fold and Cmax 4.1-fold compared to placebo. The T½ and Tmax of buspirone were not significantly affected by diltiazem. Enhanced effects and increased toxicity of buspirone may be possible during concomitant administration with diltiazem. Subsequent dose adjustments may be necessary during co- administration, and should be based on clinical assessment Dilitazem/ Corticosteroids (e.g Methyprednisolone): Concomitant administration has resulted in the inhibition of methylprednisolone metabolism (CYP3A4) and inhibition of P-glycoprotein. The patient should be monitored when initiating methylprednisolone treatment. An adjustment in the dose of methylprednisolone may be necessary Diltiazem/Alpha Blockers: Concomitant treatment with alpha-blockers may produce or aggravate hypotension. The combination of diltiazem with an alpha-blocker should only be considered with the strict monitoring of blood pressure due to the risk of increased antihypertensive effects. Diltiazem/Rimonabant: Co-administration with diltiazem results in an increase in serum rimonabant levels. Diltiazem/Short and Long Acting Nitrates: Increased hypotensive effects and faintness may be seen due to additive vasodilatating effects. In patients treated with calcium channel antagonists, the addition of nitrate derivatives should only be carried out at gradually increasing doses. Diltiazem/Phenobarbital/Phenytoin: As with all drugs, care should be exercised when treating patients with multiple medications. Diltiazem undergoes biotransformation by cytochrome P450 mixed function oxidase. Coadministration of diltiazem with other agents which follow the same route of biotransformation may result in the competitive inhibition of metabolism. Dosages of similarly metabolized drugs, particularly those of low therapeutic ratio, or in patients with renal and/or hepatic impairment, may require adjustment when starting or stopping concomitantly administered diltiazem, in order to maintain optimum therapeutic blood levels. Diltiazem/Quinidine/Theophylline/Carbamazepine: Pharmacologic effects may be increased due to inhibition of hepatic metabolism possibly by diltiazem. The increased plasma levels cause neurotoxic symptoms which resolve several days after stopping the calcium blocker. Concomitant administration of diltiazem with carbamazepine has been reported to result in elevated serum levels of carbamazepine (40% to 72% increase) resulting in toxicity in some cases. Diltiazem/Tricyclic Antidepressants: Diltiazem may increase the bioavailability of tricyclic antidepressants. Diltiazem/Cimetidine/Ranitidine: Cimetidine or ranitidine increase the bioavailability of diltiazem. Patients on diltiazem should be monitored closely when adding cimetidine or ranitidine and, if necessary, the dose of diltiazem should be reduced. Diltiazem/Statins: Diltiazem is an inhibitor of CYP3A4 and has been shown to significantly increase the AUC of some statins. The risk of myopathy and rhabdomyolysis due to statins metabolised by CYP3A4 may be increased with concomitant use of diltiazem. When possible, a non CYP3A4-metabolised statin should be used together with diltiazem, otherwise close monitoring for signs and symptoms of a potential statin toxicity is required. Diltiazem/Cyclosporin: Cyclosporin plasma levels may be increased by diltiazem, and renal toxicity may occur. Therefore, cyclosporine concentrations should be monitored, especially when diltiazem therapy is initiated, adjusted, or discontinued. Diltiazem/Lithium: Diltiazem and lithium appear to act synergistically. Neurotoxicity has occurred with coadministration, even when the lithium level was in the therapeutic range. Diltiazem/Digoxin: Serum digoxin levels may be increased upon concomitant administration of calcium channel blockers and digoxin. Although some studies suggest that no significant interaction occurs with diltiazem, caution is required and digoxin levels be monitored when initiating, adjusting, and discontinuing diltiazem therapy to avoid possible over or underdigitalization. Diltiazem/Anticoagulants/Aspirin/Salicylates: Anticoagulants, aspirin and salicylates are highly protein-bound drugs. Caution should be exercised upon concomitant administration with diltiazem, since serum levels of these agents may be increased. Diltiazem/Antihypertensive Agents (e.g. ACE Inhibitors)/Alcohol: Additive hypotensive effects may result upon concomitant administration. Therefore, caution should be exercised, and dosage adjustments of either agents may be necessary. Diltiazem/Inhalation Anesthetics: Concurrent use with calcium channel blockers may produce additive hypotensive effects. Therefore, caution should be exercised when inhalation anesthetics are administered during surgery, to patients on dialtiazem. Diltiazem/Encainide: Serum encainide levels may be increased without any change in the levels of the active metabolites of encainide. Diltiazem/Fentanyl: Severe hypotension or increased fluid volume requirements have occurred in patients receiving nifedipine and fentanyl concomitantly; this interaction should also be considered for all calcium blockers. Diltiazem/Dantrolene Infusion: Lethal ventricular fibrillation is regularly observed in animals when intravenous verapamil and dantrolene are administered concomitantly. The combination of a calcium channel antagonist and dantrolene is therefore potentially dangerous.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לב וכלי דם | AMLODIPINE, FELODIPINE, DILTIAZEM, LERCANIDIPINE |
שימוש לפי פנקס קופ''ח כללית 1994
Vasospastic angina (Prinzmetal), chronic stable angina
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
