Quest for the right Drug
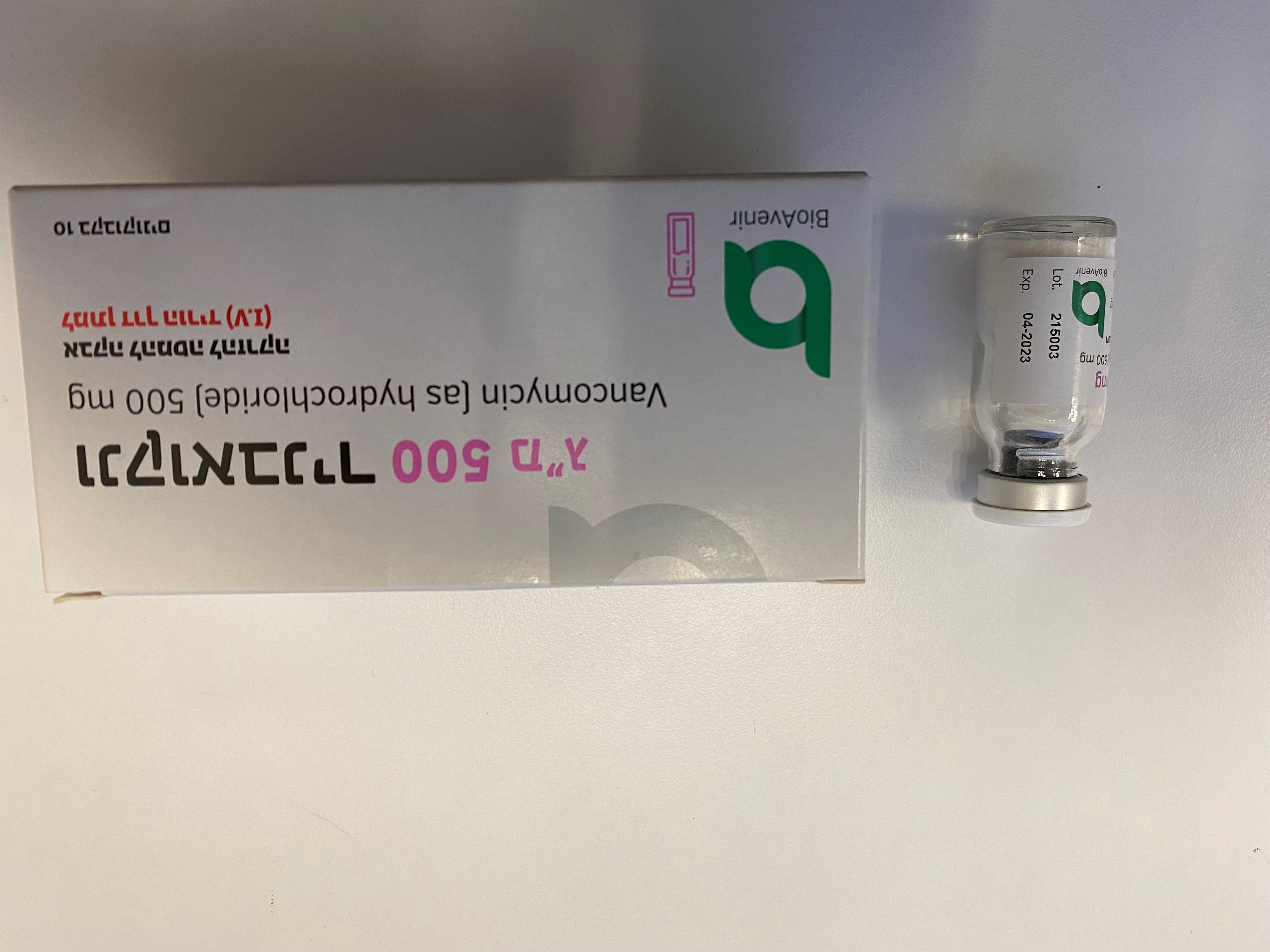
ונקואבניר 500 מ"ג VANCOAVENIR 500 MG (VANCOMYCIN AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1. Pharmacodynamic properties ANTIBIOTIC ANTIBACTERIAL AGENT OF THE GLYCOPEPTIDE FAMILY (J: anti- infectious), ATC code : J01XA01 Mechanism of action Vancomycin is a tricyclic glycopeptide antibiotic that inhibits the synthesis of the cell wall in sensitive bacteria by binding with high affinity to the D-alanyl-D-alanine terminus of cell wall precursor units. The drug is slowly bactericidal for dividing microorganisms. In addition, it impairs the permeability of the bacterial cell membrane and RNA synthesis. Pharmacokinetic/ Pharmacodynamic relationship Vancomycin displays concentration-independent activity with the area under the concentration curve (AUC) divided by the minimum inhibitory concentration (MIC) of the target organism as the primary predictive parameter for efficacy. On basis of in vitro, animal and limited human data, an AUC/MIC ratio of 400 has been established as a PK/PD target to achieve clinical effectiveness with vancomycin. To achieve this target when MICs are ≥ 1.0 mg/L, dosing in the upper range and high trough serum concentrations (15-20 mg/L) are required (see section 4.2). Mechanism of resistance Acquired resistance to glycopeptides is most common in enterococci and is based on acquisition of various van gene complexes which modifies the D-alanyl-D-alanine target to D-alanyl-D-lactate or D-alanyl-D-serine which bind vancomycin poorly. In some countries, increasing cases of resistance are observed particularly in enterococci; multi-resistant strains of Enterococcus faecium are especially alarming. Van genes have rarely been found in Staphylococcus aureus, where changes in cell wall structure result in “intermediate” susceptibility, which is most commonly heterogeneous. Also, methicillin-resistant staphylococcus strains (MRSA) with reduced susceptibility for vancomycin were reported. The reduced susceptibility or resistance to vancomycin in Staphylococcus is not well understood. Several genetic elements and multiple mutations are required. There is no cross-resistance between vancomycin and other classes of antibiotics. Cross-resistance with other glycopeptide antibiotics, such as teicoplanin, does occur. Secondary development of resistance during therapy is rare. Synergism: The combination of vancomycin with an aminoglycoside antibiotic has a synergistic effect against many strains of Staphylococcus aureus, non-enterococcal D-streptococci, enterococci and streptococci of the Viridans group. The combination of vancomycin with a cephalosporin has a synergistic effect against some oxacillin-resistant Staphylococcus epidermidis strains, and the combination of vancomycin with rifampicin has a synergistic effect against Staphylococcus epidermidis and a partial synergistic effect against some Staphylococcus aureus strains. As vancomycin in combination with a cephalosporin may also have an antagonistic effect against some Staphylococcus epidermidis strains and in combination with rifampicin against some Staphylococcus aureus strains, preceding synergism testing is useful. Specimens for bacterial cultures should be obtained in order to isolate and identify the causative organisms and to determine their susceptibility to vancomycin. Susceptibility testing breakpoints Vancomycin is active against gram-positive bacteria, such as staphylococci, streptococci, enterococci, pneumococci, and clostridia. Gram-negative bacteria are resistant. The prevalence of acquired resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the utility of the agent in at least some types of infections is questionable. This information only provides approximate guidance on the chance whether micro-organisms are susceptible to vancomycin. Minimum inhibitory concentration (MIC) breakpoints established by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) are as follows: Susceptible Resistant Staphylococcus aureus (1) ≤ 2 mg/L > 2 mg/l Coagulase-negative ≤ 4 mg/L > 4 mg/l staphylococci (1) Enterococcus spp. ≤ 4 mg/L > 4 mg/L Streptococcus groups A, B, C ≤ 2 mg/L > 2 mg/l and G Streptococcus pneumoniae ≤ 2 mg/L > 2 mg/l Gram positive anaerobes ≤ 2 mg/L > 2 mg/l (1) S. aureus with vancomycin MIC values of 2 mg/L are on the border of the wild type distribution and there may be an impaired clinical response. Commonly susceptible species Gram positive Enterococcus faecalis. Staphylococcus aureus Methicillin-resistant Staphylococcus aureus Coagulase negative Staphylococci Streptococcus spp. Streptococcus pneumoniae Enterococcus spp. Staphylococcus spp. Anaerobic species Clostridium spp except Clostriduim innocuum Eubacterium spp. Peptostreptococcus spp. Inconstant susceptible species (acquired resistance ≥ 10%) Enterococcus faecium Inherently resistant All Gram negative bacteria Gram positive aerobic species Erysipelothrix rhusiopathiae Heterofermentative Lactobacillus Leuconostoc spp. Pediococcus spp. Anaerobic species Clostridium innocuum The emergence of resistance towards vancomycin differs from one hospital to another and a local microbiological laboratory should therefore be contacted for relevant local information.
Pharmacokinetic Properties
5.2. Pharmacokinetic properties Absorption Vancomycin is administered intravenously for the treatment of systemic infections. In the case of patients with normal renal function, intravenous infusion of multiple doses of 1 g vancomycin (15 mg/kg) for 60 minutes produces approximate average plasma concentrations of 50-60 mg/L, 20-25 mg/L and 5-10 mg/L, immediately, 2 hours and 11 hours after completing the infusion, respectively. The plasma levels obtained after multiple doses are similar to those achieved after a single dose. If vancomycin is administered during a peritoneal dialysis intraperitoneally, approximately 30-65% reach the systemic cycle during the first 6 hours. After intraperitoneal administration of 30 mg/kg serum levels of approximately 10 mg/L are reached. Vancomycin is not usually absorbed into the blood after oral administration. However, absorption may occur after oral administration in patients with (pseudomembranous) colitis. This may lead to vancomycin accumulation in patients with co-existing renal impairment. Distribution The volume of distribution is about 60 L/1.73 m² body surface. At serum concentrations of vancomycin of 10 mg/L to 100 mg/L, the binding of the drug to plasma proteins is approximately 30-55%, measured by ultra-filtration. Vancomycin diffuses readily across the placenta and is distributed into cord blood. In non- inflamed meninges, vancomycin passes the blood-brain barrier only to a low extent. Biotransformation There is very little metabolism of the drug. After parenteral administration, it is excreted almost completely as microbiologically active substance (approx. 75-90% within 24 hours) through glomerular filtration via the kidneys. Elimination The elimination half-life of vancomycin is 4 to 6 hours in patients with normal renal function and 2.2-3 hours in children. Plasma clearance is about 0.058 L/kg/h and kidney clearance about 0.048 L/kg/h. In the first 24 hours, approximately 80 % of an administered dose of vancomycin is excreted in the urine through glomerular filtration. Renal dysfunction delays the excretion of vancomycin. In anephric patients, the mean half-life is 7.5 days. Due to ototoxicity of vancomycin therapy-adjuvant monitoring of the plasma concentrations is indicated in such cases. Biliary excretion is insignificant (less than 5% of a dose). Although the vancomycin is not eliminated efficiently by haemodialysis or peritoneal dialysis, there have been reports of an increase in vancomycin clearance with haemoperfusion and haemofiltration. After oral administration, only a fraction of the administered dose is recovered in the urine. In contrast, high concentrations of vancomycin are found in the faeces (>3100 mg/kg with doses of 2 g/day). Linerarity/non-linearity Vancomycin concentration generally increases proportionally with increasing dose. Plasma concentrations during multiple dose administration are similar to those after the administration of a single dose. Characteristics in specific groups Renal impairment Vancomycin is primarily cleared by glomerular filtration. In patients with impaired renal function the terminal elimination half-life of vancomycin is prolonged and the total body clearance is reduced. Subsequently, optimal dose should be calculated in line with dosing recommendations provided in section 4.2. Posology and method of administration. Hepatic impairment Vancomycin pharmacokinetics is not altered in patients with hepatic impairment. Pregnant Women Significantly increased doses may be required to achieve therapeutic serum concentrations in pregnant women (see section 4.6). Overweight patients Vancomycin distribution may be altered in overweight patients due to increases in volume of distribution, in renal clearance and possible changes in plasma protein binding. In these subpopulations vancomycin serum concentration were found higher than expected in male healthy adults (see section 4.2). Paediatric population Vancomycin PK has shown wide inter-individual variability in preterm and term neonates. In neonates, after intravenous administration, vancomycin volume of distribution varies between 0.38 and 0.97 L/kg, similar to adult values, while clearance varies between 0.63 and 1.4 mL/kg/min. Half-life varies between 3.5 and 10 h and is longer than in adults, reflecting the usual lower values for clearance in the neonate. In infants and older children, the volume of distribution ranges between 0.26-1.05 L/kg while clearance varies between 0.33-1.87 mL/kg/min.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
