Quest for the right Drug
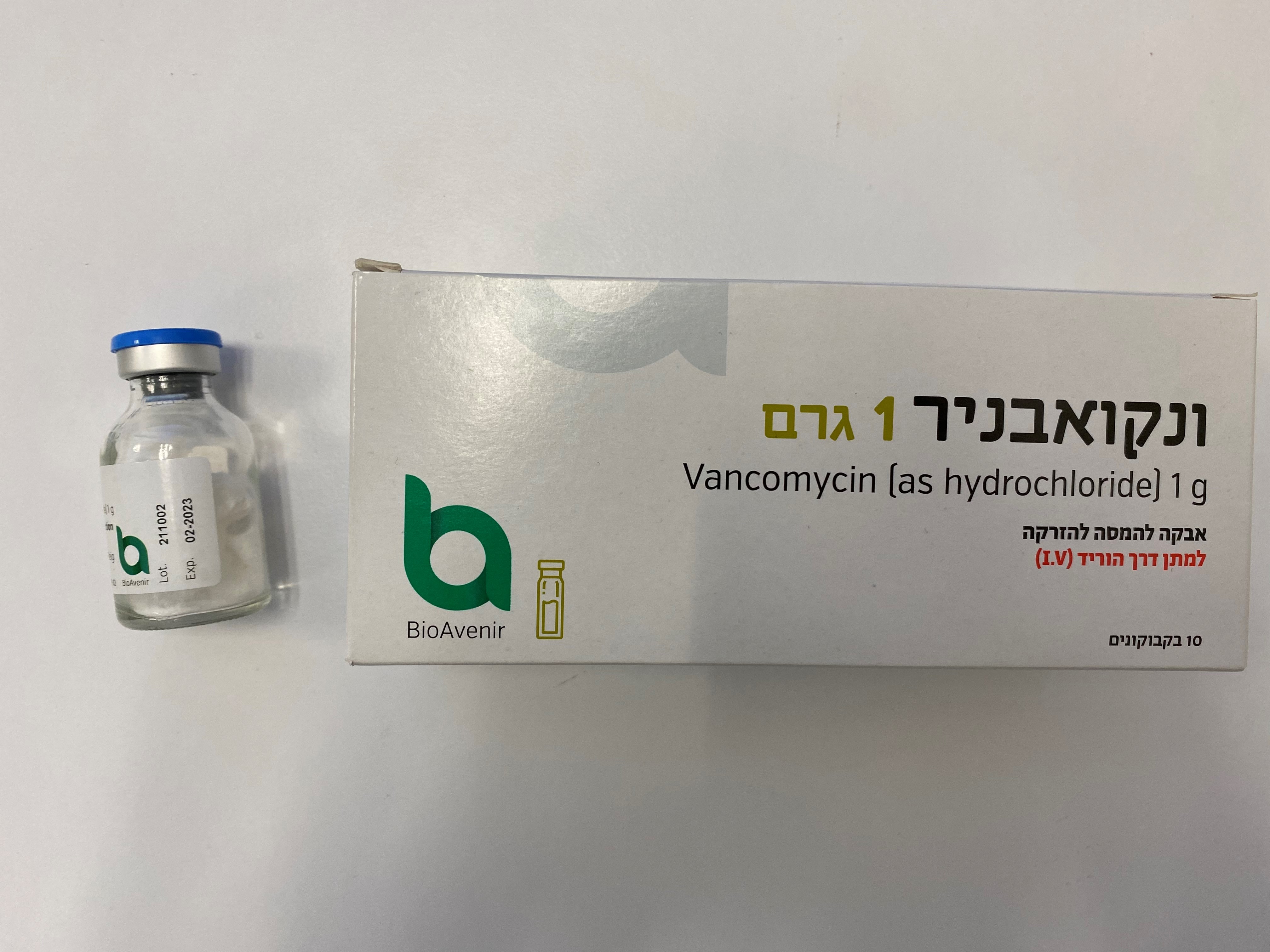
ונקואבניר 1 ג' VANCOAVENIR 1 G (VANCOMYCIN AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה לזריקה : POWDER FOR SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Therapeutic indications for intravenous and oral administration are different. Both administration routes could not be commuted. Intravenous administration Solution concentrations of no more than 5 mg/ml are recommended. In selected patients in need of fluid restriction, solution concentration up to 10 mg/ml may be used; use of such higher concentrations may increase the risk of infusion-related events (see section 6.6). Infusions should be given over at least 60 minutes. In adults, if doses exceeding 500 mg are used, a rate of infusion of no more than 10 mg/min is recommended. Infusion-related adverse events are related to both concentration and rate of administration of vancomycin. The duration of treatment is guided by the severity of the infection and its clinical and bacteriological progression. Patients with normal renal and hepatic functions Adults, adolescents and children over 12 years old: The recommended daily intravenous dose is 2000 mg (2g), divided into 500 mg doses administered every 6 hours or (1g) 1000mg every 12 hours. Each dose should be administered at no more than 10 mg/min or over a period of at least 60 minutes, whichever is longer. For bacterial endocarditis, the generally accepted regimen is 1000 mg of vancomycin intravenously every 12 hours for 4 weeks either alone or in combination with other antibiotics (gentamicin plus rifampin, gentamicin, streptomycin). Enterococcal endocarditis is treated for 6 weeks with vancomycin in combination with an aminoglycoside – according to national recommendations. Children 1 month to 12 years old: The recommended intravenous dose is 10 mg/kg, every 6 hours. Each dose should be administered over a period of at least 60 minutes. Infants and newborn: The recommended initial dose is 15 mg/kg, followed by 10 mg/kg every 12 hours during the first week of life, and every 8 hours after that age and up to 1 month of age.Each dose should be administered over at least 60 minutes. Close monitoring of serum concentrations of vancomycin is recommended. See section 'Patients with impaired renal function' below. Elderly patients: Lower maintenance doses than for adults may be required due to the age –related reduction in renal function. Obese patients: Modification of usual daily doses may be required. Patients with impaired hepatic function: There is no evidence that the dose has to be reduced in patients with impaired hepatic function. Patients with impaired renal function: Dosage adjustment must be made in patients with impaired renal function. In order to optimize dosage, serum vancomycin concentrations should be measured by means of microbiological assay, radioimmunoassay, fluorescence polarization immunoassay, fluorescence immunoassay or high pressure liquid chromatography. Calculation of vancomycin daily dose: measure creatinine clearance and use the table below (daily dose of vancomycin in mg is around 15 times the glomerular filtration rate in ml/min): VANCOMYCIN POSOLOGY IN PATIENTS WITH IMPAIRED RENAL FUNCTION (Adapted from Moellering et al.)1 Creatinine clearance Vancomycin dose (ml/min) (mg/24 hours) 100 1545 90 1390 80 1235 70 1080 60 925 50 770 40 620 30 465 20 310 10 155 1 Moellering RC, Krogstad DJ, Greenb1att DJ: Vancomycin therapy in patients with impaired renal function: a nomogram for dosage. Ann Intem Med 1981; 94:343. This table is not valid for functionally anephric patients. For such patients, an initial dose of 15 mg/kg of body weight should be administered to achieve prompt therapeutic serum concentrations. The dose required to maintain stable concentrations is 1.9 mg/kg/24 hours. When only serum creatinine is known, the following formula (based on sex, weight and age of patient) may be used to calculate approximate creatinine clearance, and actual creatinine clearance should be measured promptly. Calculated creatinine clearances (ml/min) are only estimates. Weight (kg) x (140 – age in years) Men = Women = 0.85 x above value 72 x serum creatinine concentration (mg/100 ml) The formula above should not be used in particular conditions with decreased renal function (shock, severe heart failure or oliguria), obesity, malnutrition, oedema or ascites, since it would give an overestimate of actual creatinine clearance. Where possible, the creatinine clearance should always be determined. In patients with slight or moderate renal impairment, the initial dose should not be lower than 15 mg/kg. In patients with severe renal impairment, it may be preferable to administer maintenance doses of 250 mg to 1 g once every several days rather than administering lower doses on a daily basis. Patients with anuria (with practically no renal function) should receive a dose of 15 mg/kg body weight until the therapeutic serum concentration is reached. The maintenance doses are 1.9 mg/kg body weight per 24 hours. In order to facilitate the procedure, adult patients with strongly impaired renal function may obtain a maintenance dose of 250 - 1000 mg at intervals of several days instead of a daily dose. Dosage in case of haemodialysis: For patients without any renal function, even under regular hemodialysis, the following dosage is also possible: Saturating dose 1000 mg, maintenance dose 1000 mg every 7 - 10 days. If polysulfone membranes are used in haemodialysis (high flux dialysis), the half-life of vancomycin is reduced. An additional maintenance dose may be necessary in patients on regular haemodialysis. Monitoring of vancomycin serum concentrations: The serum concentration of vancomycin should be monitored at the second day of treatment immediately prior to the next dose, and one hour post infusion. Therapeutic vancomycin blood levels should be between 30 and 40 mg/l (maximum 50 mg/l) one hour after the end of the infusion, the minimum level (short prior to the next administration) between 5 and 10 mg/l. The concentrations should normally be monitored twice or three times per week. Oral administration Treatment of colitis due to C. difficile Adults: The usual daily dose is 0,5g to 2 g given in 4 divided doses (125 mg to 500 mg per dose) for 7 to 10 days. Children: The usual daily dose is 40 mg/kg/day given in 4 divided doses, up to a maximum of 250 mg/dose, for 7 to 10 days. Method of administration: For intravenous infusion only, and not for intramuscular administration. Parenterally vancomycin shall only be administered as slow intravenous infusion (not more than 10 mg/min – over at least 60 min) which is sufficiently diluted (at least 500 mg/100ml or at least 1000mg/200 ml). Patients requiring fluid restriction can receive a solution of 500 mg /50 ml or 1000 mg /100 ml. With these higher concentrations the risk for infusion related side effects can be increased. The reconstituted solution may also be used for oral administration. Therapeutic indications for intravenous and oral administration are different. Both administration routes could not be commuted. For information about the preparation of the solution, please refer to section 6.6 special precautions for disposal and other handling.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
