Quest for the right Drug
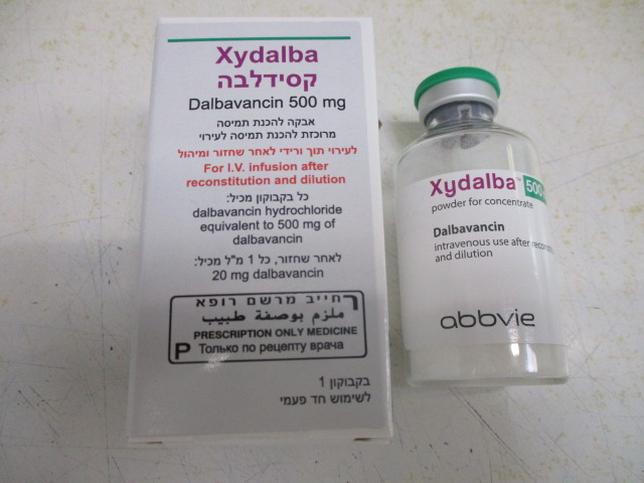
קסידלבה XYDALBA (DALBAVANCIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: antibacterials for systemic use, glycopeptide antibacterials, ATC code: J01XA04. Mechanism of action Dalbavancin is a bactericidal lipoglycopeptide. Its mechanism of action in susceptible Gram-positive bacteria involves interruption of cell wall synthesis by binding to the terminal D-alanyl-D-alanine of the stem peptide in nascent cell wall peptidoglycan, preventing cross-linking (transpeptidation and transglycosylation) of disaccharide subunits resulting in bacterial cell death. Mechanism of resistance All Gram-negative bacteria are inherently resistant to dalbavancin. Resistance to dalbavancin in Staphylococcus spp. and Enterococcus spp. is mediated by VanA, a genotype that results in modification of the target peptide in nascent cell wall. Based on in vitro studies the activity of dalbavancin is not affected by other classes of vancomycin resistance genes. Dalbavancin MICs are higher for vancomycin-intermediate staphylococci (VISA) than for fully vancomycin susceptible strains. If the isolates with higher dalbavancin MICs represent stable phenotypes and are correlated with resistance to the other glycopeptides, then the likely mechanism would be an increase in the number of glycopeptide targets in nascent peptidoglycan. Cross-resistance between dalbavancin and other classes of antibiotics was not seen in in vitro studies. Methicillin resistance has no impact on dalbavancin activity. Interactions with other antibacterial agents In in vitro studies, no antagonism has been observed between dalbavancin and other commonly used antibiotics (i.e. cefepime, ceftazidime, ceftriaxone, imipenem, meropenem, amikacin, aztreonam, ciprofloxacin, piperacillin/tazobactam and trimethoprim/sulfamethoxazole), when tested against 12 species of Gram-negative pathogens (see section 4.5). Susceptibility testing breakpoints Minimum inhibitory concentration (MIC) breakpoints determined by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) are: • Staphylococcus spp.: Susceptible ≤ 0.125 mg/l; Resistant > 0.125 mg/l, • Beta-haemolytic streptococci of Groups A, B, C, G: Susceptible ≤ 0.125 mg/l; Resistant > 0.125 mg/l, • Viridans group streptococci (Streptococcus anginosus group only): Susceptible ≤ 0.125 mg/l; Resistant > 0.125 mg/l. PK/PD relationship Bactericidal activity against staphylococci in vitro is time-dependent at serum concentrations of dalbavancin similar to those obtained at the recommended dose in humans. In vivo PK/PD relationship of dalbavancin for S. aureus was investigated using a neutropenic model of animal infection that showed that net reduction in the log10 of colony-forming units (CFU) was greatest when larger doses were given less frequently. Clinical efficacy against specific pathogens Efficacy has been demonstrated in clinical studies against the pathogens listed for ABSSSI that were susceptible to dalbavancin in vitro: • Staphylococcus aureus, • Streptococcus pyogenes, • Streptococcus agalactiae, • Streptococcus dysgalactiae, • Streptococcus anginosus group (includes S. anginosus, S. intermedius, and S. constellatus). Antibacterial activity against other relevant pathogens Clinical efficacy has not been established against the following pathogens although in vitro studies suggest that they would be susceptible to dalbavancin in the absence of acquired mechanisms of resistance: • Group G streptococci • Clostridium perfringens • Peptostreptococcus spp.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics of dalbavancin have been characterised in healthy subjects, patients, and special populations. Systemic exposures to dalbavancin are dose proportional following single doses over a range of 140 to 1120 mg, indicating linear pharmacokinetics of dalbavancin. No accumulation of dalbavancin was observed following multiple intravenous infusions administered once-weekly for up to 8 weeks (1,000 mg on Day 1, followed by up to 7 weekly 500 mg doses) in healthy adults. The mean terminal elimination half-life (t1/2) was 372 (range 333 to 405) hours. The pharmacokinetics of dalbavancin are best described using a three-compartment model (α and β distributional phases followed by a terminal elimination phase). Thus, the distributional half-life (t1/2β), which constitutes most of the clinically-relevant concentration-time profile, ranged from 5 to 7 days and is consistent with once-weekly dosing. Estimated pharmacokinetic parameters of dalbavancin following the two-dose regimen and the single-dose regimen, respectively, are shown in Table 2 below. Table 2 Mean (SD) dalbavancin pharmacokinetic parameters using population PK analysis1 Parameter Two-dose regimen2 Single-dose regimen3 Cmax (mg/L) Day 1: 281 (52) Day 1: 411 (86) Day 8: 141 (26) AUC0-Day14 18100 (4600) 20300 (5300) (mg•h/L) CL (L/h) 0.048 (0.0086) 0.049 (0.0096) 1 Source: DAL-MS-01. 2 1,000 mg on Day 1 + 500 mg on Day 8; Study DUR001-303 subjects with evaluable PK sample. 3 1,500 mg; Study DUR001-303 subjects with evaluable PK sample. The dalbavancin plasma concentration-time following the two-dose and the single-dose regimens, respectively, are shown in Figure 1. Figure 1. Dalbavancin Plasma Concentrations versus time in a typical ABSSSI patient (simulation using population pharmacokinetic model) for both the single and the two- dose regimens. Distribution Clearance and volume of distribution at steady state are comparable between healthy subjects and patients with infections. The volume of distribution at steady state was similar to the volume of extracellular fluid. Dalbavancin is reversibly bound to human plasma proteins, primarily to albumin. The plasma protein binding of dalbavancin is 93 % and is not altered as a function of drug concentration, renal insufficiency, or hepatic insufficiency. Following a single intravenous dose of 1,000 mg in healthy volunteers AUC in skin blister fluid amounted (bound and unbound dalbavancin) to approximately 60 % of the plasma AUC at day 7 post- dose. Biotransformation Metabolites have not been observed in significant amounts in human plasma. The metabolites hydroxy-dalbavancin and mannosyl aglycone have been detected in urine (< 25 % of administered dose). The metabolic pathways responsible for producing these metabolites have not been identified; however, due to the relatively minor contribution of metabolism to the overall elimination of dalbavancin, drug-drug interactions via inhibition or induction of metabolism of dalbavancin are not anticipated. Hydroxy-dalbavancin and mannosyl aglycone show significantly less antibacterial activity compared to dalbavancin. Elimination Following administration of a single 1,000 mg dose in healthy subjects, an average of 19 % to 33 % of the administered dalbavancin dose was excreted in urine as dalbavancin and 8 % to 12 % as the metabolite hydroxy-dalbavancin. Approximately 20 % of the administered dose was excreted in faeces. Special populations Renal impairment The pharmacokinetics of dalbavancin were evaluated in 28 subjects with varying degrees of renal impairment and in 15 matched control subjects with normal renal function. Following a single dose of 500 mg or 1,000 mg dalbavancin, the mean plasma clearance (CLT) was reduced 11 %, 35 %, and 47 % in subjects with mild (CLCR 50 - 79 ml/min), moderate (CLCR 30 – 49 ml/min), and severe (CLCR < 30 ml/min) renal impairment, respectively, compared to subjects with normal renal function. The mean AUC for subjects with creatinine clearance < 30 ml/min was approximately 2 - fold higher. The clinical significance of the decrease in mean plasma CLT, and the associated increase in AUC0-∞ noted in these pharmacokinetic studies of dalbavancin in subjects with severe renal impairment has not been established. Dalbavancin pharmacokinetics in subjects with end-stage renal disease receiving regularly scheduled renal dialysis (3 times/week) were similar to those observed in subjects with mild to moderate renal impairment, and less than 6 % of an administered dose is removed after 3 hours of haemodialysis. For dosing instructions in subjects with renal impairment refer to section 4.2. Hepatic impairment The pharmacokinetics of dalbavancin were evaluated in 17 subjects with mild, moderate, or severe hepatic impairment and compared to 9 matched healthy subjects with normal hepatic function. The mean AUC was unchanged in subjects with mild hepatic impairment compared to subjects with normal hepatic function; however, the mean AUC decreased by 28 % and 31 %, respectively, in subjects with moderate and severe hepatic impairment. The cause and the clinical significance of the decreased exposure in subjects with moderate and severe hepatic function are unknown. For dosing instructions in subjects with hepatic impairment refer to section 4.2. Gender Clinically significant gender-related differences in dalbavancin pharmacokinetics have not been observed in healthy subjects or in patients with infections. No dose adjustment is recommended based on gender. Elderly The pharmacokinetics of dalbavancin were not significantly altered with age; therefore, dose adjustment is not necessary based on age (see section 4.2). The experience with dalbavancin in elderly is limited: 276 patients ≥ 75 years of age were included in the Phase 2/3 clinical studies, of which 173 received dalbavancin. Patients up to 93 years of age have been included in clinical studies.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
