Quest for the right Drug
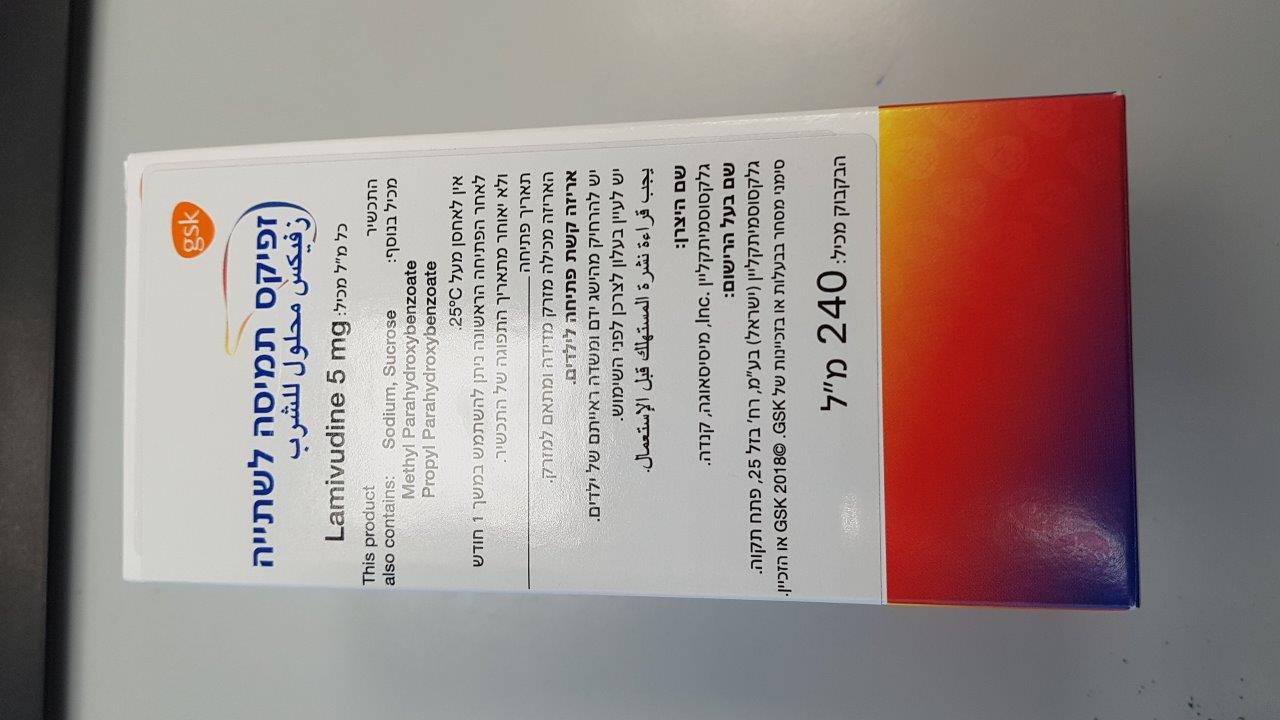
זפיקס תמיסה לשתייה ZEFFIX ORAL SOLUTION (LAMIVUDINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
אין פרטים : ORAL SOLUTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Exacerbations of Hepatitis after Discontinuation of Treatment Clinical and laboratory evidence of exacerbations of hepatitis have occurred after discontinuation of lamivudine. These exacerbations have been detected primarily by serum ALT elevations in addition to re-emergence of HBV DNA commonly observed after stopping treatment; see Table 4 for more information regarding frequency of posttreatment ALT elevations [see Adverse Reactions (6.1)]. Although most events appear to have been self-limited, fatalities have been reported in some cases. The causal relationship to discontinuation of lamivudine treatment is unknown. Patients should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment with ZEFFIX. There is insufficient evidence to determine whether re-initiation of ZEFFIX alters the course of posttreatment exacerbations of hepatitis. 5.2 Risk of HIV-1 Resistance if ZEFFIX is Used in Patients with Unrecognized or Untreated HIV-1 Infection Zeffix tablets and oral solution contain a lower lamivudine dose than the lamivudine dose used to treat HIV-1 infection with EPIVIR tablets and oral solution or with lamivudine-containing antiretroviral fixed-dose combination products. ZEFFIX is not appropriate for patients co-infected with HBV and HIV-1. If a patient with unrecognized or untreated HIV-1 infection is prescribed Zeffix for the treatment of HBV, rapid emergence of HIV-1 resistance is likely to result because of the subtherapeutic dose and the inappropriate use of monotherapy for HIV-1 treatment. HIV counseling and testing should be offered to all patients before beginning treatment with ZEFFIX and periodically during treatment because of the risk of rapid emergence of resistant HIV-1 and limitation of treatment options if ZEFFIX is prescribed to treat chronic hepatitis B in a patient who has unrecognized or untreated HIV-1 infection or who acquires HIV-1 infection during treatment. 5.3 Emergence of Resistance-Associated HBV Substitutions In controlled clinical trials, YMDD-mutant HBV was detected in subjects with on ZEFFIX re-appearance of HBV DNA after an initial decline below the assay limit [see Microbiology (12.4)]. Subjects treated with ZEFFIX (adults and children) with YMDD-mutant HBV at 52 weeks showed diminished treatment responses in comparison with subjects treated with ZEFFIX without evidence of YMDD substitutions, including the following: lower rates of HBeAg seroconversion and HBeAg loss (no greater than placebo recipients), more frequent return of positive HBV DNA, and more frequent ALT elevations. In the controlled trials, when subjects developed YMDD-mutant HBV, they had a rise in HBV DNA and ALT from their previous on-treatment levels. Progression of hepatitis B, including death, has been reported in some subjects with YMDD-mutant HBV, including subjects from the liver transplant setting and from other clinical trials. In order to reduce the risk of resistance in patients receiving monotherapy with Zeffix, a switch to an alternative regimen should be considered if serum HBV DNA remains detectable after 24 weeks of treatment. Optimal therapy should be guided by resistance testing. 5.4 Lactic Acidosis and Severe Hepatomegaly with Steatosis Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues, including Zeffix. A majority of these cases have been in women. Female sex and obesity may be risk factors for the development of lactic acidosis and severe hepatomegaly with steatosis in patients treated with antiretroviral nucleoside analogues. Most of these reports have described patients receiving nucleoside analogues for treatment of HIV infection, but there have been reports of lactic acidosis in patients receiving lamivudine for hepatitis B. Treatment with Zeffix should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations. Zeffix tablets: This medicine contains less than 1mmol sodium (23mg) per tablet, that is to say essentially ‘sodium free’ Zeffix oral solution: Sucrose Patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption or sucrase-isomaltase insufficiency should not take this medicine. Diabetic patients should be advised that each dose of oral solution (100 mg = 20 ml) contains 4 g of sucrose Propyl parahydroxybenzoate and methyl parahydroxybenzoateThe oral solution contains propyl and methyl parahydroxybenzoate. These products may cause allergic reactions (possibly delayed). Each 20 ml dose contains: 30 mg of methyl parahydroxybenzoate (E218) and 3.6 mg of propyl parahydroxybenzoate (E216) Propylene glycol This medicine contains 400 mg propylene glycol in each 20 ml. Sodium This medicinal product contains 58.8mg sodium per 20ml dose, equivalent to 2.9% of the WHO recommended maximum daily intake of 2g sodium for an adult. 6 ADVERSE REACTIONS The following adverse reactions are discussed in other sections of the labeling: • Exacerbations of hepatitis B after discontinuation of treatment [see Warnings and Precautions (5.1)]. • Risk of emergence of resistant HIV-1 infection [see Warnings and Precautions (5.2)]. • Risk of emergence of resistant HBV infection [see Warnings and Precautions (5.3)]. • Lactic acidosis and severe hepatomegaly with steatosis [see Warnings and Precautions (5.4)]. 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. Clinical Trials Experience in Adult Subjects with Chronic HBV Infection Clinical adverse reactions (regardless of investigator’s causality assessment) reported in greater than or equal to 10% of subjects who received Zeffix and reported at a rate greater than in subjects who received placebo are listed in Table 2. Table 2. Clinical Adverse Reactionsa Reported in Greater than or Equal to 10% of Subjects Who Received Zeffix for 52 to 68 Weeks and at an Incidence Greater than Placebo (Trials 1-3) Adverse Event ZEFFIX Placebo (n = 332) (n = 200) Ear, Nose, and Throat Ear, nose, and throat infections 25% 21% Sore throat 13% 8% Gastrointestinal Diarrhea 14% 12% a Includes adverse events regardless of severity and causality assessment. Specified laboratory abnormalities reported in subjects who received ZEFFIX and reported at a rate greater than in subjects who received placebo are listed in Table 3. Table 3. Frequencies of Specified Laboratory Abnormalities Reported during Treatment at a Greater Frequency in Subjects Treated with ZEFFIX than with Placebo (Trials 1-3)a Subjects with Abnormality/Subjects with Test Observations (Abnormal Level) ZEFFIX Placebo Serum Lipase 2.5 x ULN b 10% 7% Creatine Phosphokinase (CPK) 9% 5% 7 x baseline Platelets <50,000/mm3 4% 3% a Includes subjects treated for 52 to 68 weeks. b Includes observations during and after treatment in the 2 placebo-controlled trials that collected this information. ULN = Upper limit of normal. In subjects followed for up to 16 weeks after discontinuation of treatment, posttreatment ALT elevations were observed more frequently in subjects who had received ZEFFIX than in subjects who had received placebo. A comparison of ALT elevations between Weeks 52 and 68 in subjects who discontinued ZEFFIX at Week 52 and subjects in the same trials who received placebo throughout the treatment course is shown in Table 4. Table 4. Posttreatment ALT Elevations with No-Active-Treatment Follow-up (Trials 1 and 3) Subjects with ALT Elevation/ Subjects with Observationsa Abnormal Value Zeffixb Placebob ALT 2 x baseline value 27% 19% ALT 3 x baseline value c 21% 8% ALT 2 x baseline value and absolute ALT 15% 7% >500 IU/L ALT 2 x baseline value; and bilirubin >2 x 0.7% 0.9% ULN and 2 x baseline value a Each subject may be represented in one or more category. b During treatment phase. c Comparable to a Grade 3 toxicity in accordance with modified WHO criteria. ULN = Upper limit of normal. Clinical Trials Experience in Pediatric Subjects with Chronic HBV Infection Most commonly observed adverse reactions in the pediatric trials were similar to those in adult trials. Posttreatment transaminase elevations were observed in some subjects followed after cessation of ZEFFIX. 6.2 Postmarketing Experience The following adverse reactions have been identified during post-approval use of ZEFFIX. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These reactions have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to lamivudine. Blood and Lymphatic Anemia (including pure red cell aplasia and severe anemias progressing on therapy), lymphadenopathy, splenomegaly, thrombocytopenia. Digestive Stomatitis. Endocrine and Metabolic Hyperglycemia. General Weakness. Hepatic and Pancreatic Lactic acidosis and steatosis [see Warnings and Precautions (5.4)], posttreatment exacerbations of hepatitis [see Warnings and Precautions (5.1)], pancreatitis. Hypersensitivity Anaphylaxis, urticaria. Musculoskeletal Cramps, rhabdomyolysis. Nervous Paresthesia, peripheral neuropathy. Respiratory Abnormal breath sounds/wheezing. Skin Alopecia, pruritus, rash. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il Additionally, you should also report to GSK Israel (il.safety@gsk.com).
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2000
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
28.07.19 - עלון לצרכן 04.01.22 - עלון לצרכן אנגלית 08.05.22 - עלון לצרכן אנגלית 04.01.22 - עלון לצרכן עברית 08.05.22 - עלון לצרכן עברית 04.01.22 - עלון לצרכן ערבית 08.05.22 - עלון לצרכן ערבית 16.02.24 - עלון לצרכן עברית 04.05.24 - עלון לצרכן אנגלית 04.05.24 - עלון לצרכן עברית 04.05.24 - עלון לצרכן ערבית 25.06.24 - עלון לצרכן עברית 20.01.16 - החמרה לעלון 12.10.21 - החמרה לעלון 25.06.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
זפיקס תמיסה לשתייה