Quest for the right Drug
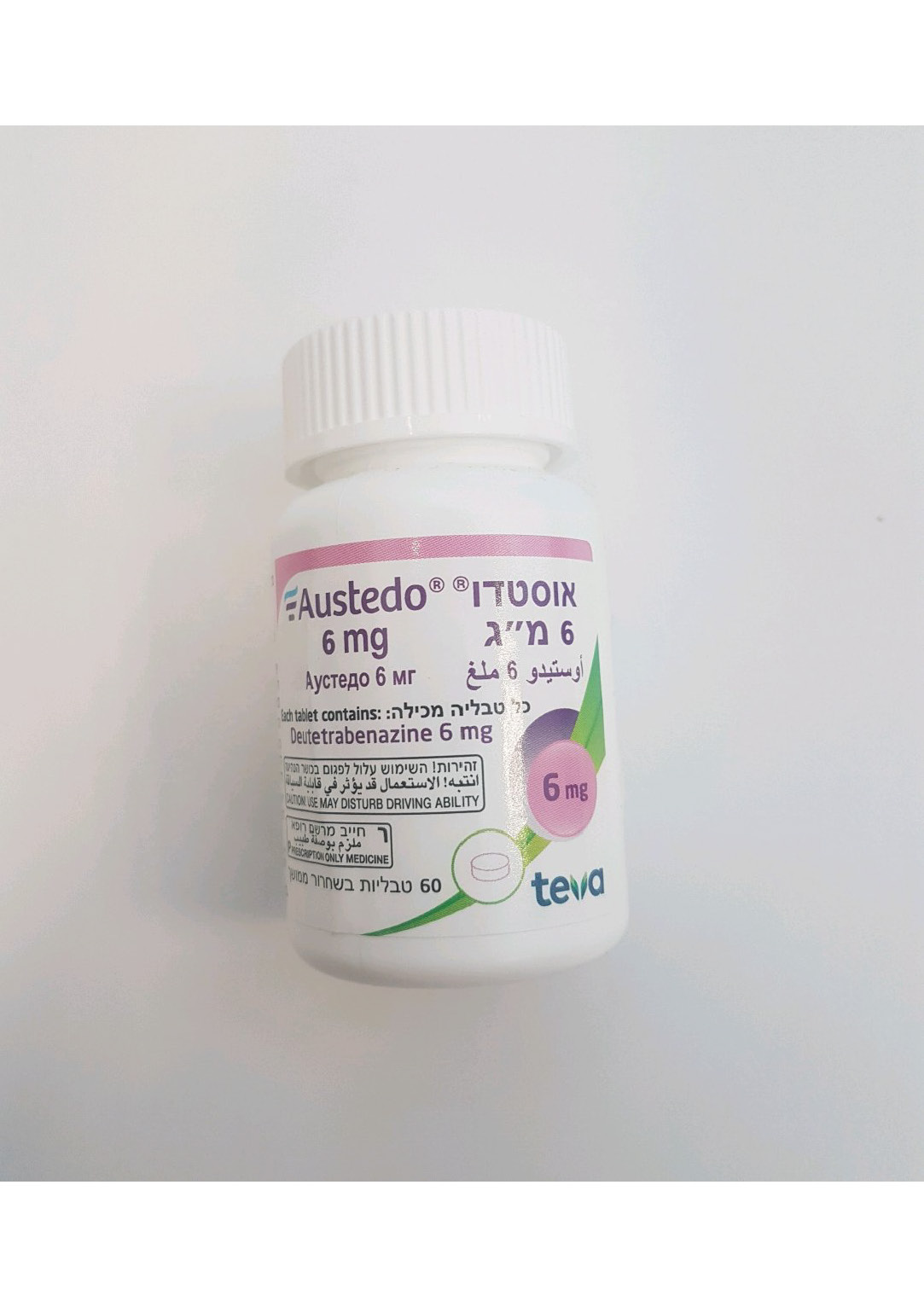
אוסטדו 6 מ"ג AUSTEDO 6 MG (DEUTETRABENAZINE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות עם שחרור נרחב : TABLETS EXTENDED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
12.2 Pharmacodynamics Cardiac Electrophysiology At the maximum recommended dose, AUSTEDO does not prolong the QT interval to any clinically relevant extent. An exposure-response analysis on QTc prolongation from a study in extensive or intermediate (EM) and poor CYP2D6 metabolizers (PM) showed that a clinically- relevant effect can be excluded at exposures following single doses of 24 and 48 mg of AUSTEDO. Melanin Binding Deutetrabenazine or its metabolites bind to melanin-containing tissues (i.e., eye, skin, fur) in pigmented rats. After a single oral dose of radiolabeled deutetrabenazine, radioactivity was still detected in eye and fur at 35 days following dosing [see Warnings and Precautions (5.9)].
Pharmacokinetic Properties
12.3 Pharmacokinetics After oral dosing up to 25 mg, plasma concentrations of deutetrabenazine are generally below the limit of detection because of the extensive hepatic metabolism of deutetrabenazine. Systemic exposure (Cmax and AUC) for the active metabolites increased proportionally to dose following single or multiple doses of deutetrabenazine (6 mg to 24 mg and 7.5 mg twice daily to 22.5 mg twice daily). Absorption Following oral administration of deutetrabenazine, the extent of absorption is at least 80%. Peak plasma concentrations (Cmax) of deuterated α-HTBZ and β-HTBZ are reached within 3 to 4 hours after dosing. Effect of Food The effects of food on the bioavailability of AUSTEDO were studied in subjects administered a single dose with and without food. Food had no effect on AUC of α-HTBZ or β-HTBZ, although Cmax was increased by approximately 50% in the presence of food [see Dosage and Administration (2.1)]. Distribution The median volume of distribution (Vc/F) of the α-HTBZ, and the β-HTBZ metabolites of AUSTEDO are approximately 500 L and 730 L, respectively. Results of PET-scan studies in humans show that following intravenous injection of 11C-labeled tetrabenazine or α-HTBZ, radioactivity is rapidly distributed to the brain, with the highest binding in the striatum and lowest binding in the cortex. The in vitro protein binding of tetrabenazine, α-HTBZ, and β-HTBZ was examined in human plasma for concentrations ranging from 50 to 200 ng/Ml. Tetrabenazine binding ranged from 82% to 85%, α-HTBZ binding ranged from 60% to 68%, and β-HTBZ binding ranged from 59% to 63%. Elimination AUSTEDO is primarily renally eliminated in the form of metabolites. The half-life of the active deuterated α-HTBZ, β-HTBZ, and total (α+β)-HTBZ is approximately 12 hours, 7.5 hours, and 9 to 11 hours, respectively. The clearance values (CL/F) of the α-HTBZ, and the β-HTBZ metabolites of AUSTEDO are approximately 65 L/hour and 200 L/hour, respectively, for a 70 kg HD or TD patient with functional CYP2D6 metabolism in the fed state. Metabolism In vitro experiments in human liver microsomes demonstrate that deutetrabenazine is extensively biotransformed, mainly by carbonyl reductase, to its major active metabolites, α-HTBZ and β- HTBZ, which are subsequently metabolized primarily by CYP2D6, with minor contributions of CYP1A2 and CYP3A4/5, to form several minor metabolites. Excretion In a mass balance study in 6 healthy subjects, 75% to 86% of the deutetrabenazine dose was excreted in the urine, and fecal recovery accounted for 8% to 11% of the dose. Urinary excretion of the α-HTBZ and β-HTBZ metabolites from deutetrabenazine each accounted for less than 10% of the administered dose. Sulfate and glucuronide conjugates of the α-HTBZ and β-HTBZ metabolites of deutetrabenazine, as well as products of oxidative metabolism, accounted for the majority of metabolites in the urine. Specific Populations Male and Female Patients There is no apparent effect of gender on the pharmacokinetics of α-HTBZ and β-HTBZ of deutetrabenazine. Patients with Renal Impairment No clinical studies have been conducted to assess the effect of renal impairment on the PK of AUSTEDO. Patients with Hepatic Impairment The effect of hepatic impairment on the pharmacokinetics of deutetrabenazine and its primary metabolites has not been studied. However, in a clinical study conducted to assess the effect of hepatic impairment on the pharmacokinetics of tetrabenazine, a closely related VMAT2 inhibitor, the exposure to α-HTBZ and β-HTBZ was up to 40% greater in patients with hepatic impairment, and the mean tetrabenazine Cmax in patients with hepatic impairment was up to 190-fold higher than in healthy subjects [see Contraindications (4), Use in Specific Populations (8.6)]. Poor CYP2D6 Metabolizers Although the pharmacokinetics of deutetrabenazine and its metabolites have not been systematically evaluated in patients who do not express the drug metabolizing enzyme CYP2D6, it is likely that the exposure to α-HTBZ and β-HTBZ would be increased similarly to taking strong CYP2D6 inhibitors (approximately 3-fold) [see Dosage and Administration (2.4), Drug Interactions (7.1)]. Drug Interaction Studies Deutetrabenazine, α-HTBZ, and β-HTBZ have not been evaluated in in vitro studies for induction or inhibition of CYP enzymes or interaction with P-glycoprotein. The results of in vitro studies of tetrabenazine do not suggest that tetrabenazine or its α-HTBZ or β-HTBZ metabolites are likely to result in clinically significant inhibition of CYP2D6, CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2E1, or CYP3A. In vitro studies suggest that neither tetrabenazine nor its α-HTBZ or β-HTBZ metabolites are likely to result in clinically significant induction of CYP1A2, CYP3A4, CYP2B6, CYP2C8, CYP2C9, or CYP2C19. Neither tetrabenazine nor its α-HTBZ or β-HTBZ metabolites are likely to be a substrate or inhibitor of P-glycoprotein at clinically relevant concentrations in vivo. The deutetrabenazine metabolites, 2-methylpropanoic acid of β-HTBZ (M1) and monohydroxy tetrabenazine (M4), have been evaluated in a panel of in vitro drug-drug interaction studies; the results indicate that M1/M4 are not expected to cause clinically relevant drug interactions. CYP2D6 Inhibitors In vitro studies indicate that the α-HTBZ and β-HTBZ metabolites of deutetrabenazine are substrates for CYP2D6. The effect of CYP2D6 inhibition on the pharmacokinetics of deutetrabenazine and its metabolites was studied in 24 healthy subjects following a single 22.5 mg dose of deutetrabenazine given after 8 days of administration of the strong CYP2D6 inhibitor paroxetine 20 mg daily. In the presence of paroxetine, systemic exposure (AUCinf) of α-HTBZ was 1.9-fold higher and β-HTBZ was 6.5-fold higher, resulting in approximately 3-fold increase in AUCinf for total (α+β)-HTBZ. Paroxetine decreased the clearance of α-HTBZ and β-HTBZ metabolites of AUSTEDO with corresponding increases in mean half-life of approximately 1.5- fold and 2.7-fold, respectively. In the presence of paroxetine, Cmax of α-HTBZ and β-HTBZ were 1.2-fold and 2.2-fold higher, respectively. The effect of moderate or weak CYP2D6 inhibitors such as duloxetine, terbinafine, amiodarone, or sertraline on the exposure of deutetrabenazine and its metabolites has not been evaluated. Digoxin AUSTEDO was not evaluated for interaction with digoxin. Digoxin is a substrate for P- glycoprotein. A study in healthy subjects showed that tetrabenazine (25 mg twice daily for 3 days) did not affect the bioavailability of digoxin, suggesting that at this dose, tetrabenazine does not affect P-glycoprotein in the intestinal tract. In vitro studies also do not suggest that tetrabenazine or its metabolites are P-glycoprotein inhibitors.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. מחלת הנטינגטון עם תנועות לא רצוניות משמעותיות TMC≥8 (total maximal chorea).2. הפרעת תנועה מאוחרת (Tardive Dyskinesia) בדרגת חומרה בינונית- קשה (דירוג total AIMS≥ 6 או מעל 3 נקודות באזור אחד של הגוף).ב. מתן התרופה ייעשה לפי מרשם של מומחה בנוירולוגיה או בפסיכיאטריה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מחלת הנטינגטון עם תנועות לא רצוניות משמעותיות TMC≥8 (total maximal chorea). | 01/02/2023 | נוירולוגיה | מחלת הנטינגטון, Huntington's chorea | |
| הפרעת תנועה מאוחרת (Tardive Dyskinesia) בדרגת חומרה בינונית- קשה (דירוג total AIMS≥ 6 או מעל 3 נקודות באזור אחד של הגוף). | 01/02/2023 | נוירולוגיה | הפרעת תנועה מאוחרת, Tardive dyskinesia |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/02/2023
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
