Quest for the right Drug
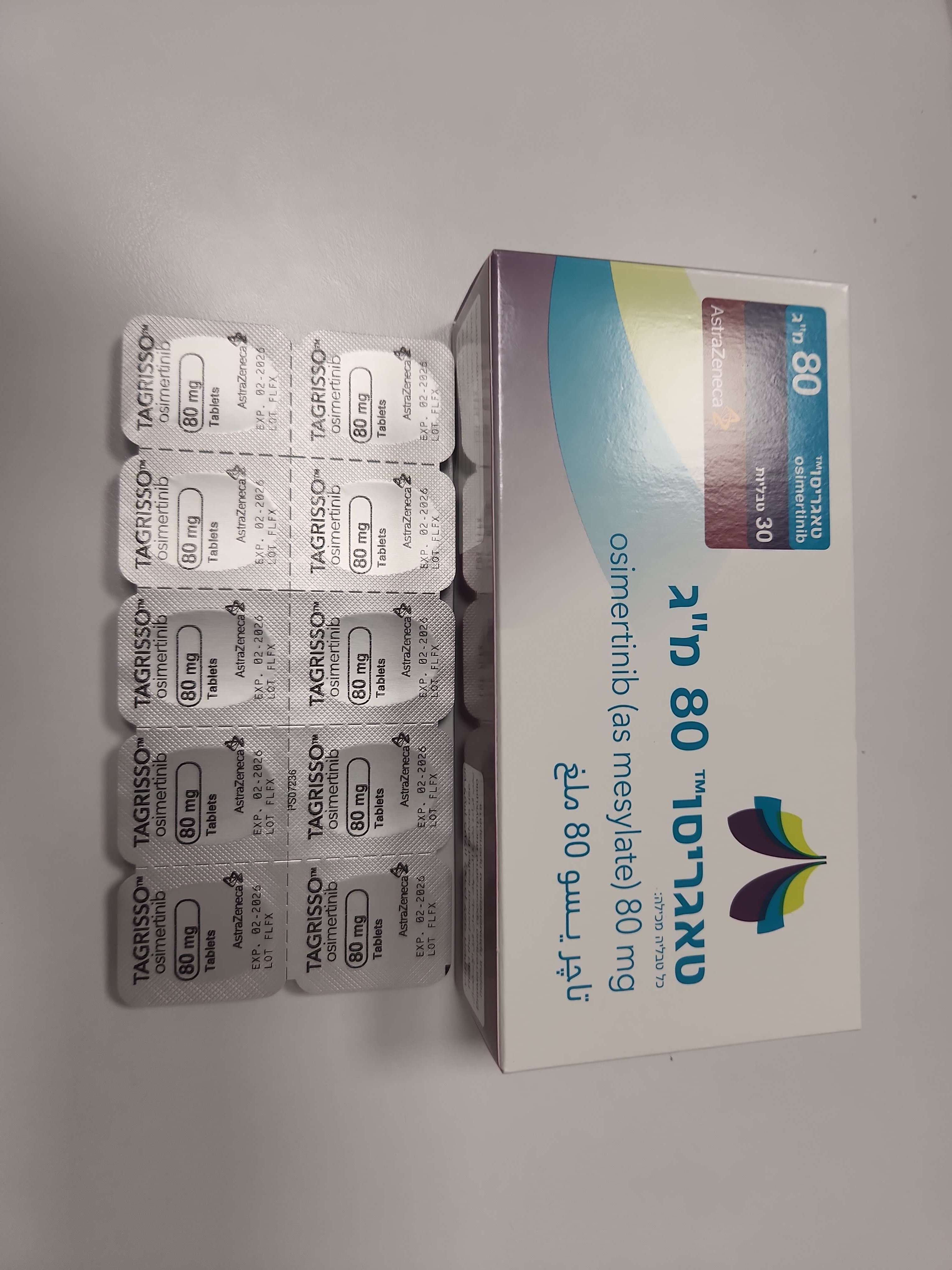
טאגריסו 80 מ"ג TAGRISSO 80 MG (OSIMERTINIB AS MESYLATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: antineoplastic agents, protein kinase inhibitors; ATC code: L01EB04. Mechanism of action Osimertinib is a Tyrosine Kinase Inhibitor (TKI). It is an irreversible inhibitor of EGFRs harboring sensitising-mutations (EGFRm) and TKI-resistance mutation T790M. Pharmacodynamic effects In vitro studies have demonstrated that osimertinib has high potency and inhibitory activity against EGFR across a range of all clinically relevant EGFR sensitising-mutant and T790M mutant NSCLC cell lines (apparent IC50s from 6 nM to 54 nM against phospho-EGFR). This leads to inhibition of cell growth, while showing significantly less activity against EGFR in wild-type cell lines (apparent IC50s from 480 nM to 1.8 μM against phospho-EGFR). In vivo oral administration of osimertinib lead to tumour shrinkage in both EGFRm and T790M NSCLC xenograft and transgenic mouse lung tumour models. Cardiac electrophysiology The QTc interval prolongation potential of TAGRISSO was assessed in 210 patients who received osimertinib 80 mg daily in AURA2. Serial ECGs were collected following a single dose and at steady-state to evaluate the effect of osimertinib on QTc intervals. A pharmacokinetic/pharmacodynamic analysis predicted a drug-related QTc interval prolongation at 80 mg of 14 msec with an upper bound of 16 msec (90% CI). Clinical efficacy and safety Adjuvant Treatment of EGFR Mutation-Positive NSCLC , with or without prior adjuvant chemotherapy – ADAURA The efficacy and safety of TAGRISSO for the adjuvant treatment of patients with EGFR mutation-positive (Ex19del or L858R) NSCLC who have had complete tumor resection, with or without prior adjuvant chemotherapy was demonstrated in a randomised, double-blind, placebo-controlled study (ADAURA). Eligible patients with resectable tumors stage IB – IIIA (according to American Joint Commission on Cancer [AJCC] 7th edition) were required to have EGFR mutations (Ex19del or L858R), identified by the cobas EGFR Mutation Test performed prospectively using biopsy or surgical specimen in a central laboratory. Patients were randomised 1:1 to receive TAGRISSO (n=339, 80 mg orally once daily) or placebo (n=343) following recovery from surgery and standard adjuvant chemotherapy where given. Patients not receiving adjuvant chemotherapy were randomised within 10 weeks and patients receiving adjuvant chemotherapy within 26 weeks following surgery. Randomisation was stratified by EGFR mutation type (Ex19del or L858R), ethnicity (Asian or non-Asian) and staging based on percutaneous transthoracic needle biopsy (pTNM) (IB or II or IIIA) according to AJCC 7th edition. Treatment was given until disease recurrence, unacceptable toxicity, or for 3 years. The major efficacy outcome measure was disease-free survival (DFS) by investigator assessment in the stage II-IIIA population. DFS by investigator assessment in the stage IB-IIIA population (overall population) was an additional efficacy outcome measure. Other additional efficacy outcome measures included DFS rate, overall survival (OS), OS rate, and time to deterioration in health-related quality of life (HRQoL) SF-36. The baseline demographic and disease characteristics of the overall population were: median age 63 years (range 30-86 years), ≥75 years old (11%), female (70%), Asian (64%), never smokers (72%), World Health Organization (WHO) performance status of 0 (64%) or 1 (36%), stage IB (31%), stage II (34%), and IIIA (35%). With regards to EGFR mutation status 55% were exon 19 deletions and 45% were exon 21 L858R substitution mutations; 9 patients (1%) also had a concurrent de novo T790M mutation. The majority (60%) of patients received adjuvant chemotherapy prior to randomization (26% IB; 71% IIA; 73% IIB; 80% IIIA). At the time of the DFS analysis, 205 (61%) patients were still on active treatment; of the 73 (11%) patients who had the opportunity to complete the 3-year treatment period, 40 (12%) were in the osimertinib arm and 33 (10%) in the placebo arm. There were 37 patients who had disease recurrence on TAGRISSO. The most commonly reported sites of recurrence were: lung (19 patients); lymph nodes (10 patients) and central nervous system (CNS) (5 patients). There were 157 patients who had disease recurrence on placebo. The most commonly reported sites were: lung (61 patients); lymph nodes (48 patients) and CNS (34 patients). ADAURA demonstrated a statistically significant reduction in the risk of disease recurrence or death for patients treated with TAGRISSO compared to patients treated with placebo in the stage II-IIIA population. Similar results were observed in the stage IB-IIIA population. Efficacy results from ADAURA by investigator assessment are summarized in Table 3. Table 3. Efficacy results from ADAURA by Investigator Assessment Stage II-IIIA population Stage IB-IIIA population TAGRISSO TAGRISSO Efficacy parameter Placebo (N=237) Placebo (N=343) (N=233) (N=339) Disease-free survival Number of events (%) 26 (11) 130 (55) 37 (11) 159 (46) Recurrent disease (%) 26 (11) 129 (54) 37 (11) 157 (46) Deaths (%) 0 1 (0.4) 0 2 (0.6) Median DFS, months (95% CI) NC (38.8, NC) 19.6 (16.6, 24.5) NC (NC, NC) 27.5 (22.0, 35.0) HR (99.06% CI); P- 0.17 (0.11, 0.26); <0.0001a 0.20 (0.14, 0.30); <0.0001b value DFS rate at 12 months (%) 97 (94, 99) 61 (54, 67) 97 (95, 99) 69 (63, 73) (95% CI) DFS rate at 24 months (%) 90 (84, 93) 44 (37, 51) 89 (85, 92) 52 (46, 58) (95% CI) DFS rate at 36 months (%) 78 (65, 87) 28 (19, 38) 79 (69, 86) 40 (32, 48) (95% CI)c, d HR=Hazard Ratio; CI=Confidence Interval; NC=Not Calculable DFS results based on investigator assessment A HR< 1 favours TAGRISSO Median follow-up time for DFS was 22.1 months for patients receiving TAGRISSO, 14.9 months for patients receiving placebo (stage II-IIIA population) and 16.6 months for patients receiving placebo (stage IB-IIIA population). DFS results are from the primary analysis (17 January 2020). a Adjusted for an interim analysis (33% maturity) a p-value < 0.0094 was required to achieve statistical significance. b Adjusted for an interim analysis (29% maturity) a p-value <0.0088 was required to achieve statistical significance. c The number of patients at risk at 36 months was 18 patients in the TAGRISSOarm and 9 patients in the placebo arm (stage II-IIIA population). d The number of patients at risk at 36 months was 27 patients in the TAGRISSOarm and 20 patients in the placebo arm (stage IB- IIIA population). The final analysis of OS (data cut-off: 27 January 2023) demonstrated a statistically significant improvement in OS for patients treated with TAGRISSO compared to placebo for both the stage II-IIIA population (100 OS events [21% maturity]; HR=0.49; 95.03% CI: 0.33, 0.73; p-value=0.0004) and the overall population (IB-IIIA; 124 OS events [18% maturity]; HR=0.49; 95.03% CI: 0.34, 0.70; p-value < 0.0001). For both populations, the median OS was not reached in either treatment arm and the 95% CIs were not calculable. The median follow-up time for OS in all patients was 59.9 months (stage II-IIIA population) and 60.4 months (stage IB- IIIA population) in the TAGRISSO arm and 56.2 months (stage IIIIIA population) and 59.4 months (stage IB-IIIA population) in the placebo arm. Figure 1. Kaplan-Meier curve of disease-free survival in stage II-IIIA patients by Investigator Assessment Figure 2. Kaplan-Meier curve of Disease-Free Survival in stage IB-IIIA (overall population) patients by investigator assessment The DFS benefit of TAGRISSO compared to placebo was consistent across all predefined subgroups analysed, including ethnicity, age, gender, and EGFR mutation type (Ex19Del or L858R). Figure 3. Kaplan-Meier curve of overall survival in stage II-IIIA patients Figure 4. Kaplan-Meier curve of overall survival in stage IB-IIIA (overall population) patients An exploratory analysis of CNS DFS (time to CNS recurrence or death) for patients on TAGRISSO compared to patients on placebo showed a HR of 0.18 (95% CI: 0.10, 0.33; p <0.0001) for the overall population (stage IB-IIIA). Patient reported outcomes Health-related quality of life (HRQL) in ADAURA was assessed using the Short Form (36) Health Survey version 2 (SF-36v2) questionnaire. SF-36v2 was administered at 12 weeks, 24 weeks and then every 24 weeks relative to randomisation until treatment completion or discontinuation. Overall, HRQL was maintained in both arms up to 30 months, with at least 70% of patients in the stage II-IIIA population not experiencing a clinically meaningful deterioration in the physical component of the SF-36 or death (70% vs 76% for TAGRISSO vs placebo), or in the mental component of the SF-36 or death (70% vs 71% for TAGRISSO vs placebo). Previously untreated EGFR mutation positive locally advanced or metastatic NSCLC – FLAURA The efficacy and safety of TAGRISSO for the treatment of patients with EGFR mutation positive locally advanced, not amenable to curative surgery or radiotherapy, or metastatic NSCLC who had not received previous systemic treatment for advanced disease, was demonstrated in a randomised, double-blind, active-controlled study (FLAURA). Patient tumour tissue samples were required to have one of the two common EGFR mutations known to be associated with EGFR TKI sensitivity (Ex19del or L858R), as identified by local or central testing. Patients were randomised 1:1 to receive either TAGRISSO (n=279, 80 mg orally once daily) or EGFR TKI comparator (n=277; gefitinib 250 mg orally once daily or erlotinib 150 mg orally once daily). Randomisation was stratified by EGFR mutation type (Ex19del or L858R) and ethnicity (Asian or non- Asian). Patients received study therapy until intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. For patients receiving EGFR TKI comparator, post- progression crossover to open-label TAGRISSO was permitted provided tumour samples tested positive for the T790M mutation. The primary efficacy end-point was progression-free survival (PFS) as assessed by investigator. The baseline demographic and disease characteristics of the overall study population were: median age 64 years (range 26-93 years), ≥75 years old (14%), female (63%), White (36%), Asian (62%), never smokers (64%), World Health Organization (WHO) performance status of 0 or 1 (100%), metastatic bone disease (36%), extra-thoracic visceral metastases (35%), CNS metastases (21%, identified by CNS lesion site at baseline, medical history, and/or prior surgery, and/or prior radiotherapy to CNS metastases). TAGRISSO demonstrated a clinically meaningful and statistically significant improvement in PFS compared to EGFR TKI comparator (median 18.9 months and 10.2 months, respectively, HR=0.46, 95% CI: 0.37, 0.57; P<0.0001). Efficacy results from FLAURA by investigator assessment are summarised in Table 4, and the Kaplan-Meier curve for PFS is shown in Figure 5. The final analysis of overall survival (OS, 58% maturity), demonstrated a statistically significant improvement with an HR of 0.799 (95.05% CI: 0.641, 0. 997) and a clinically meaningful longer median survival time in patients randomized to TAGRISSO compared to EGFR TKI comparator (Table 4 and Figure 6). A greater proportion of patients treated with TAGRISSO were alive at 12, 18, 24 and 36 months (89%, 81%, 74% and 54%, respectively) compared to patients treated with EGFR TKI comparator (83 %, 71%, 59% and 44% respectively). Analysis of post-progression endpoints demonstrated that the PFS benefit was preserved through subsequent lines of therapy. Table 4. Efficacy results from FLAURA by investigator assessment EGFR TKI comparator TAGRISSO Efficacy parameter (gefitinib or erlotinib) (N=279) (N=277) Progression-free survival Number of events (62% maturity) 136 (49) 206 (74) Median PFS, months (95% CI) 18.9 (15.2, 21.4) 10.2 (9.6, 11.1) HR (95% CI) ; P-value 0.46 (0.37, 0.57); P < 0.0001 Overall survival Number of deaths, (58% maturity) 155 (56) 166 (60) Median OS, months (95% CI) 38.6 (34.5, 41.8) 31.8 (26.6, 36.0) HR (95.05% CI); P-value 0.799 (0.641, 0.997); P=0.0462 † Objective response rate *1 Number of responses (n),Response Rate 223 210 (95% CI) 80% (75, 85) 76% (70, 81) Odds ratio (95% CI); P-value 1.3 (0.9, 1.9); P=0.2421 Duration of response (DoR)* Median DoR, months (95% CI) 17.2 (13.8, 22.0). 8.5 (7.3, 9.8) Second PFS after start of first subsequent therapy (PFS2) Number of patients with second 73 (26) 106 (38) progression (%) Median PFS2, months (95% CI) NC (23.7, NC) 20.0 (18.0, NC) HR (95% CI); P-value 0.58 (0.44, 0.78); P=0.0004 Time from randomisation to first subsequent treatment or death (TFST) Number of patients who had first subsequent 115 (41) 175 (63) treatment or died (%) Median TFST, months (95% CI) 23.5 (22.0, NC) 13.8 (12.3, 15.7) HR (95% CI); P-value 0.51 (0.40, 0.64); P<0.0001 Time from randomisation to second subsequent treatment or death (TSST) Number of patients who had second 75 (27) 110 (40) subsequent treatment or died (%) Median TSST, months (95% CI) NC (NC, NC) 25.9 (20.0, NC) HR (95% CI); P-value 0.60 (0.45, 0.80); P=0.0005 HR=Hazard Ratio; CI=Confidence Interval, NC=Not Calculable, PFS, ORR, DoR and PFS2 results based on RECIST investigator assessment *Based on unconfirmed response Median follow-up time was 15.0 months for patients receiving TAGRISSO and 9.7 months for patients receiving EGFR TKI comparator Median survival follow-up time was 35.8 months for patients receiving TAGRISSO and 27.0 months for patients receiving EGFR TKI comparator. PFS, ORR, DoR, PFS2, TFST and TSST results are from data cut-off 12 June 2017. OS results are from data cut-off 25 June 2019 A HR< 1 favours TAGRISSO, an Odds ratio of >1 favours TAGRISSO † Adjusted for an interim analysis (25% maturity) a P-value < 0. 0495 was required to achieve statistical significance 1 ORR results by Blinded Independent Central Review (BICR) were consistent with those reported via investigator assessment; ORR by BICR assessment was 78% (95% CI:73, 83) on TAGRISSO and 70% (95% CI:65, 76) on EGFR TKI comparator. Figure 5. Kaplan-Meier curves of progression-free survival as assessed by investigator in FLAURA Figure 6. Kaplan-Meier curves of overall survival in FLAURA The PFS benefit of TAGRISSO compared to EGFR TKI comparator was consistent across all predefined subgroups analysed, including ethnicity, age, gender, smoking history, CNS metastases status at study entry and EGFR mutation type (Exon 19 deletion or L858R). CNS metastases efficacy data in FLAURA study Patients with CNS metastases not requiring steroids and with stable neurologic status for at least two weeks after completion of the definitive therapy and steroids were eligible to be randomised in the FLAURA study. Of 556 patients, 200 patients had available baseline brain scans. A BICR assessment of these scans resulted in a subgroup of 128/556 (23%) patients with CNS metastases and these data are summarised in Table 5. CNS efficacy by RECIST v1.1 in FLAURA demonstrated a statistically significant improvement in CNS PFS (HR=0.48, 95% CI 0.26, 0.86; P=0.014). Table 5. CNS efficacy by BICR in patients with CNS metastases on a baseline brain scan in FLAURA EGFR TKI comparator TAGRISSO Efficacy parameter (gefitinib or erlotinib) N=61 N=67 CNS progression-free survival1 Number of events (%) 18 (30) 30 (45) Median CND PFS, months (95% CI) NC (16.5, NC) 13.9 (8.3, NC) HR (95% CI); P-value 0.48 (0.26, 0.86); P=0.014 CNS progression free and alive at 6 87 (74, 94) 71 (57, 81) months (%) (95% CI) CNS progression free and alive at 12 77 (62, 86) 56 (42, 68) months (%) (95% CI) HR=Hazard Ratio; CI=Confidence Interval, NC=Not Calculable A HR< 1 favours TAGRISSO, an Odds ratio of >1 favours TAGRISSO 1 CNS PFS determined by RECIST v1.1by CNS BICR (CNS measurable and non-measurable lesions at baseline by BICR) n=61 for TAGRISSO and n=67 for EGFR TKI comparator; responses are unconfirmed A pre-specified PFS subgroup based on CNS metastases status (identified by CNS lesion site at baseline, medical history, and/or prior surgery, and/or prior radiotherapy to CNS metastases) at study entry was performed in FLAURA and is shown in Figure 7. Irrespective of CNS lesion status at study entry, patients in the TAGRISSO arm demonstrated an efficacy benefit over those in the EGFR TKI comparator arm and there were fewer patients with new CNS lesions in the TAGRISSO arm compared to the EGFR TKI comparator arm (TAGRISSO, 11/279 [3.9%] compared to EGFR TKI comparator, 34/277 [12.3%]). In the subset of patients without CNS lesions at baseline, there were a lower number of new CNS lesions in the TAGRISSO arm compared to the EGFR TKI comparator arm (7/226 [3.1%] vs. 15/214 [7.0%], respectively). Figure 7. Overall PFS by investigator assessment by CNS metastases status at study entry, Kaplan-Meier plot (full analysis set) in FLAURA Patient reported outcomes Patient-reported symptoms and health-related quality of life (HRQL) were electronically collected using the EORTC QLQ-C30 and its lung cancer module (EORTC QLQ-LC13). The LC13 was initially administered once a week for the first 6 weeks, then every 3 weeks before and after progression. The C30 was assessed every 6 weeks before and after progression. At baseline, no differences in patient reported symptoms, function or HRQL were observed between TAGRISSO and EGFR TKI comparator (gefitinib or erlotinib) arms. Compliance over the first 9 months was generally high (≥70%) and similar in both arms. Key lung cancer symptoms analysis Data collected from baseline up to month 9 showed similar improvements in TAGRISSO and EGFR TKI comparator groups for the five pre-specified primary PRO symptoms (cough, dyspnoea, chest pain, fatigue, and appetite loss) with improvement in cough reaching the established clinically relevant cut-off. Up to month 9 there were no clinically meaningful differences in patient-reported symptoms between TAGRISSO and EGFR TKI comparator groups (as assessed by a difference of ≥ 10 points). HRQL and physical functioning improvement analysis Both groups reported similar improvements in most functioning domains and global health status/HRQL, indicating that patients’ overall health status improved. Up to month 9, there were no clinically meaningful differences between the TAGRISSO and EGFR TKI comparator groups in functioning or HRQL. Pre-treated T790M positive NSCLC patients-AURA3 The efficacy and safety of TAGRISSO for the treatment of patients with locally advanced or metastatic T790M NSCLC whose disease has progressed on or after EGFR TKI therapy, was demonstrated in a randomised, open-label, active-controlled Phase 3 study (AURA3). All patients were required to have EGFR T790M mutation-positive NSCLC identified by the cobas EGFR mutation test performed in a central laboratory prior to randomisation. The T790M mutation status was also assessed using ctDNA extracted from a plasma sample taken during screening. The primary efficacy outcome was progression- free survival (PFS) as assessed by investigator. Additional efficacy outcome measures included ORR, DoR and overall survival (OS) as assessed by investigator. Patients were randomised in a 2:1 (TAGRISSO: platinum-based doublet chemotherapy) ratio to receive TAGRISSO (n=279) or platinum-based doublet chemotherapy (n=140). Randomisation was stratified by ethnicity (Asian and non-Asian). Patients in the TAGRISSO arm received TAGRISSO 80 mg orally once daily until intolerance to therapy, or the investigator determined that the patient was no longer experiencing clinical benefit. Chemotherapy consisted of pemetrexed 500 mg/m2 with carboplatin AUC5 or pemetrexed 500 mg/m2 with cisplatin 75 mg/m2 on Day 1 of every 21-day cycle for up to 6 cycles. Patients whose disease has not progressed after four cycles of platinum-based chemotherapy may receive pemetrexed maintenance therapy (pemetrexed 500 mg/m2 on Day 1 of every 21-day cycle). Subjects on the chemotherapy arm who had objective radiological progression (by the investigator and confirmed by independent central imaging review) were given the opportunity to begin treatment with TAGRISSO. The baseline demographic and disease characteristics of the overall study population were: median age 62, ≥75 years old (15%), female (64%), white (32%), Asian (65%), never smoker (68%), WHO performance status 0 or 1 (100%). Fifty-four percent (54%) of patients had extra-thoracic visceral metastases, including 34% with CNS metastases (identified by CNS lesion site at baseline, medical history, and/or prior surgery, and/or prior radiotherapy to CNS metastases) and 23% with liver metastases. Forty-two percent (42%) of patients had metastatic bone disease. AURA3 demonstrated a statistically significant improvement in PFS in the patients treated with TAGRISSO compared to chemotherapy. Efficacy results from AURA3 by investigator assessment are summarised in Table 6, and the Kaplan-Meier curve for PFS is shown in Figure 8. No statistically significant difference was observed between the treatment arms at the final OS analysis. Table 6. Efficacy results from AURA3 by investigator assessment Chemotherapy TAGRISSO (Pemetrexed/Cisplatin or Efficacy parameter (N=279) Pemetrexed/Carboplatin) (N=140) Progression-free survival Number of events (% maturity) 140 (50) 110 (79) Median PFS, months (95% CI) 10.1 (8.3, 12.3) 4.4 (4.2, 5.6) HR (95% CI); P-value 0.30 (0.23,0.41); P- <0.001 Overall survival1 (OS) Number of deaths (% maturity) 188 (67.4) 93 (66.4) 26.8 (23.5, Median OS, months (95% CI) 22.5(20. 2. 28.8) 31.5) HR (95.56% CI); P-value 0.87 (0.67, 1.13); P = 0.277 Objective response rate2 Number of responses, response rate (95% 197 44 CI) 71% (65, 76) 31% (24, 40) Odds ratio (95% CI); P-value 5.4 (3.5, 8.5); P <0.001 Duration of response (DoR)2 Median DoR, months (95% CI) 9.7 (8.3, 11.6) 4.1 (3.0, 5.6) HR=Hazard Ratio; CI=confidence interval; NC=non-calculable; ; OS=Overall Survival All efficacy results based on RECIST investigator assessment 1 The final analysis of OS was performed . at 67% maturity. The CI for the HR has been adjusted for previous interim analyses. The OS analysis was not adjusted for the potentially confounding effects of crossover (99 [71%] patients on the chemotherapy arm received subsequent osimertinib treatment). 2 ORR and DoR results by investigator assessment were consistent with those reported via Blinded Independent Central Review (BICR); ORR by BICR assessment was 64.9% [95% CI: 59.0, 70.5] on osimertinib and 34.3 % [95% CI: 26.5, 42.8] on chemotherapy; DoR by BICR assessment was 11.2 months (95% CI: 8.3, NC) on osimertinib and 3.1 months (95% CI: 2.9, 4.3) on chemotherapy. Figure 8. Kaplan-Meier curves of Progression-Free Survival as assessed by investigator in AURA3 A sensitivity analysis of PFS was conducted by a Blinded Independent Central Review (BICR) and showed a median PFS of 11.0 months with TAGRISSO compared with 4.2 months with chemotherapy. This analysis demonstrated a consistent treatment effect (HR 0.28; 95% CI: 0.20, 0.38) with that observed by investigator assessment. Clinically meaningful improvements in PFS with HRs less than 0.50 in favour of patients receiving TAGRISSO compared to those receiving chemotherapy were consistently observed in all predefined subgroups analysed, including ethnicity, age, gender, smoking history and EGFR mutation (Exon 19 deletion and L858R). CNS metastases efficacy data in AURA3 study Patients with asymptomatic, stable brain metastases not requiring steroids for at least 4 weeks prior to the start of study treatment were eligible to be randomised in the study. A BICR assessment of CNS efficacy by RECIST v1.1 in the subgroup of 116/419 (28%) patients identified to have CNS metastases on a baseline brain scan are summarised in Table 7. Table 7. CNS efficacy by BICR in patients with CNS metastases on a baseline brain scan in AURA3 Chemotherapy Efficacy parameter TAGRISSO (Pemetrexed/Cisplatin or Pemetrexed/Carboplatin) CNS objective response rate1 CNS response rate % (n/N) 70% (21/30) 31% (5/16) (95% CI) (51, 85) (11%, 59%) Odds ratio (95% CI); P-value 5.1 (1.4, 21); P=0.015 CNS duration of response2 Median CNS DoR, months (95% CI) 8.9 (4.3, NC) 5.7 (NC, NC) CNS disease control rate 87% (65/75) 68% (28/41) CNS disease control rate (77, 93) (52, 82) Odds ratio (95% CI); P-value 3 (1.2, 7.9); P=0.021 CNS progression-free survival 3 N=75 N=41 Number of events (% maturity) 19 (25) 16 (39) Median CNS PFS, months (95% CI) 11.7 (10, NC) 5.6 (4.2, 9.7) HR (95% CI); P-value 0.32 (0.15, 0.69); P=0.004 1 CNS Objective Response Rate and Duration of Response determined by RECIST v1.1 by CNS BICR in the evaluable for response population (CNS measurable lesions at baseline by BICR) n=30 for TAGRISSO and n=16 for Chemotherapy 2 Based on patients with response only; DoR defined as the time from the date of first documented response (complete response or partial response) until progression or death event; DCR defined as the proportion of patients with response (complete response or partial response), or stable disease ≥ 6 weeks 3 CNS Progression Free Survival determined by RECIST v1.1 by CNS BICR in the full analysis set population (CNS measurable and non-measurable lesions at baseline by BICR) n=75 for TAGRISSO and n=41 for Chemotherapy A HR<1 favours TAGRISSO A pre-specified PFS subgroup analysis based on CNS metastases status at study entry was performed in AURA3 and is shown in Figure 9. Figure 9. Overall PFS by investigator assessment by CNS metastases status at study entry, Kaplan-Meier plot (full analysis set) in AURA3 AURA3 demonstrated a statistically significant improvement in PFS for patients receiving TAGRISSO compared to those receiving chemotherapy irrespective of CNS metastases status at study entry. Patient reported outcomes Patient-reported symptoms and HRQL were electronically collected using the EORTC QLQ-C30 and its lung cancer module (EORTC QLQ-LC13). The LC13 was initially administered once a week for the first 6 weeks, then every 3 weeks before and after progression. The C30 was assessed every 6 weeks before and after progression. Key lung cancer symptoms analysis TAGRISSO improved patient-reported lung cancer symptoms compared to chemotherapy by demonstrating a statistically significant difference in mean change from baseline versus chemotherapy during the overall time period from randomisation until 6 months for 5 pre-specified primary PRO symptoms (appetite loss, cough, chest pain, dyspnoea, and fatigue) as shown in Table 8. Table 8. Mixed Model Repeated Measures – Key lung cancer symptoms - mean change from baseline in TAGRISSO patients compared with chemotherapy Appetite Loss Cough Chest Pain Dyspnoea Fatigue Arms TAGRISSO Chemo- TAGRISSO Chemo- TAGRISSO Chemo- TAGRISSO Chemo- TAGRISSO Chemo- (279) therapy (279) therapy (279) therapy (279) therapy (279) therapy (140) (140) (140) (140) (140) N 239 97 228 113 228 113 228 113 239 97 Adj Mean -5.51 2.73 -12.22 -6.69 -5.15 0.22 -5.61 1.48 -5.68 4.71 Estimated -8.24 -5.53 -5.36 -7.09 -10.39 (-12.88, 3.60) (-8.89, -2.17) (-8.20, -2.53) (-9.86, -4.33) (-14.55, -6.23) Difference (95%CI) p-value p <0.001 p=0.001 p<0.001 p<0.001 p<0.001 Adjusted mean and estimated differences obtained from a Mixed Model Repeated Measures (MMRM) analysis. The model included patient, treatment, visit, treatment-by-visit interaction, baseline symptom score, and baseline symptom score-by-visit interaction and used an unstructured covariance matrix. HRQL and physical functioning improvement analysis Patients on TAGRISSO had significantly greater chances of achieving a clinically meaningful improvement of greater than or equal to 10 points on the global health status and physical functioning of the EORTC-C30 questionnaire compared with chemotherapy during the study period Odds Ratio (OR) global health status: 2.11, (95% CI 1.24, 3.67, p=0.007); OR physical functioning 2.79 (95% CI 1.50, 5.46, p=0.002). Pre-treated T790M positive NSCLC patients - AURAex and AURA2 Two single-arm, open-label clinical studies, AURAex (Phase 2 Extension cohort, (n=201)) and AURA2 (n=210) were conducted in patients with EGFR T790M mutation-positive lung cancer who have progressed on one or more prior systemic therapies, including an EGFR TKI. All patients were required to have EGFR T790M mutation-positive NSCLC identified by the cobas EGFR mutation test performed in a central laboratory prior to treatment. The T790M mutation status was also assessed retrospectively using ctDNA extracted from a plasma sample taken during screening. All patients received TAGRISSO at a dose of 80 mg once daily. The primary efficacy outcome measure of these two studies was ORR according to RECIST v1.1 as evaluated by a Blinded Independent Central Review (BICR). Secondary efficacy outcome measures included Duration of Response (DoR) and Progression-Free Survival (PFS). Baseline characteristics of the overall study population (AURAex and AURA2) were as follows: median age 63 years, 13% of patients were ≥75 years old, female (68%), White (36%), Asian (60%). All patients received at least one prior line of therapy. Thirty-one percent (31%) (N=129) had received 1 prior line of therapy (EGFR-TKI treatment only), 69% (N=282) had received 2 or more prior lines. Seventy-two percent (72%) of patients were never smokers, 100% of patients had a World Health Organization (WHO) performance status of 0 or 1. Fifty-nine percent (59%) of patients had extra-thoracic visceral metastasis including 39% with CNS metastases (identified by CNS lesion site at baseline, medical history, and/or prior surgery and/or prior radiotherapy to CNS metastases) and 29% with liver metastases. Forty-seven percent (47%) of patients had metastatic bone disease. The median duration of follow up for PFS was 12.6 months. In the 411 pre-treated EGFR T790M mutation-positive patients, the total ORR by Blinded Independent Central Review (BICR) was 66% (95% CI: 61, 71). In patients with a confirmed response by BICR, the median DoR was 12.5 months (95% CI: 11.1, NE). The ORR by BICR in AURAex was 62% (95% CI: 55, 68) and 70% (95% CI: 63, 77) in AURA2. The median PFS was 11.0 months 95% CI (9.6, 12.4). Objective response rates by BICR above 50% were observed in all predefined subgroups analysed, including line of therapy, ethnicity, age and region. In the evaluable for response population, 85% (223/262) had documentation of response at the time of the first scan (6 weeks); 94% (247/262) had documentation of response at the time of the second scan (12 weeks). CNS metastases efficacy data in Phase 2 studies (AURAex and AURA2) A BICR assessment of CNS efficacy by RECIST v 1.1 was performed in a subgroup of 50 (out of 411) patients identified to have measurable CNS metastases on a baseline brain scan. A CNS ORR of 54% (27/50 patients; 95% CI: 39.3, 68.2) was observed with 12% of these responses being complete responses. Clinical studies have not been conducted in patients with de novo EGFR T790M mutation-positive NSCLC.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Osimertinib pharmacokinetic parameters have been characterized in healthy subjects and NSCLC patients. Based on population pharmacokinetic analysis, osimertinib apparent plasma clearance is 14.3 L/h, apparent volume of distribution is 918 L and terminal half-life of approximately 44 hours. The AUC and Cmax increased dose proportionally over 20 to 240 mg dose range. Administration of osimertinib once daily results in approximately 3 fold accumulation with steady-state exposures achieved by 15 days of dosing. At steady-state, circulating plasma concentrations are typically maintained within a 1.6 fold range over the 24-hour dosing interval. Absorption Following oral administration of TAGRISSO, peak plasma concentrations of osimertinib were achieved with a median (min-max) tmax of 6 (3-24) hours, with several peaks observed over the first 24 hours in some patients. The absolute bioavailability of TAGRISSO is 70% (90% CI 67, 73). Based on a clinical pharmacokinetic study in patients at 80 mg, food does not alter osimertinib bioavailability to a clinically meaningful extent. (AUC increase by 6% (90% CI -5, 19) and Cmax decrease by 7% (90% CI -19, 6)). In healthy volunteers administered an 80 mg tablet where gastric pH was elevated by dosing of omeprazole for 5 days, osimertinib exposure was not affected (AUC and Cmax increase by 7% and 2%, respectively) with the 90% CI for exposure ratio contained within the 80-125% limit. Distribution Population estimated mean volume of distribution at steady-state (Vss/F) of osimertinib is 918 L indicating extensive distribution into tissue. In vitro plasma protein binding of osimertinib is 94.7% (5.3% free). Osimertinib has also been demonstrated to bind covalently to rat and human plasma proteins, human serum albumin and rat and human hepatocytes. Biotransformation In vitro studies indicate that osimertinib is metabolized predominantly by CYP3A4, and CYP3A5. However, with current available data, alternative metabolic pathways cannot be fully ruled out. Based on in vitro studies, 2 pharmacologically active metabolites (AZ7550 and AZ5104) have subsequently been identified in the plasma of preclinical species and in humans after oral dosing with osimertinib; AZ7550 showed a similar pharmacological profile to TAGRISSO while AZ5104 showed greater potency across both mutant and wild-type EGFR. Both metabolites appeared slowly in plasma after administration of TAGRISSO to patients, with a median (min-max) tmax of 24 (4-72) and 24 (6-72) hours, respectively. In human plasma, parent osimertinib accounted for 0.8%, with the 2 metabolites contributing 0.08% and 0.07% of the total radioactivity with the majority of the radioactivity being covalently bound to plasma proteins. The geometric mean exposure of both AZ5104 and AZ7550, based on AUC, was approximately 10% each of the exposure of osimertinib at steady-state. The main metabolic pathway of osimertinib was oxidation and dealkylation. At least 12 components were observed in the pooled urine and faecal samples in humans with 5 components accounting for >1% of the dose of which unchanged osimertinib, AZ5104 and AZ7550, accounted for approximately 1.9, 6.6 and 2.7% of the dose while a cysteinyl adduct (M21) and an unknown metabolite (M25) accounted for 1.5% and 1.9% of the dose, respectively. Based on in vitro studies, osimertinib is a competitive inhibitor of CYP 3A4/5 but not CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6 and 2E1 at clinically relevant concentrations. Based on in vitro studies, osimertinib is not an inhibitor of UGT1A1 and UGT2B7 at clinically relevant concentrations hepatically. Intestinal inhibition of UGT1A1 is possible but the clinical impact is unknown. Elimination Following a single oral dose of 20 mg, 67.8% of the dose was recovered in faeces (1.2% as parent) while 14.2% of the administered dose (0.8% as parent) was found in urine by 84 days of sample collection. Unchanged osimertinib accounted for approximately 2% of the elimination with 0.8% in urine and 1.2% in faeces. Interactions with transport proteins In vitro studies have shown that osimertinib is not a substrate of OATP1B1 and OATP1B3. In vitro, osimertinib does not inhibit OAT1, OAT3, OATP1B1, OATP1B3, MATE1, OCT2 and MATE2K at clinically relevant concentrations. Based on in vitro studies osimertinib is a substrate of P-gp and BCRP but at clinical doses, clinically relevant interactions are unlikely. Based on in vitro data, osimertinib is an inhibitor of BCRP and P-gp. (See section 4.5). Special populations In a population based pharmacokinetic analyses (n=1367), no clinically significant relationships were identified between predicted steady-state exposure (AUCss) and patient’s age (range: 25 to 91 years), gender (65% female), ethnicity (including White, Asian, Japanese, Chinese and non-Asian-non-White patients), line of therapy and smoking status (n=34 current smokers, n=419 former smokers). Population PK analysis indicated that body weight was a significant covariate with a less than 20% change in osimertinib AUCss expected across a body weight range of 88kg to 43kg respectively (95% to 5% quantiles) when compared to the AUCss for the median body weight of 61 kg. Taking the extremes of body weight into consideration, from <43 kg to >88 kg, AZ5104 metabolite ratios ranged from 11.8% to 9.6% while for AZ7550 it ranged from 12.8% to 8.1% respectively. Based on population PK analysis, serum albumin was identified as a significant covariate with a <30% change in osimertinib AUCss expected across the albumin range of 29 to 46 g/L respectively (95% to 5% quantiles) when compared to the AUCss for the median baseline albumin of 39 g/L. These exposure changes due to body weight or baseline albumin differences are not considered clinically relevant. Hepatic impairment Osimertinib is eliminated mainly via the liver. In a clinical study, patients with different types of advanced solid tumours and with mild hepatic impairment (Child Pugh A, mean score = 5.3, n=7) or moderate hepatic impairment (Child Pugh B, mean score = 8.2, n=5) had no increase in exposure compared to patients with normal hepatic function (n=10) after a single 80 mg dose of TAGRISSO. The geometric mean ratio (90% CI) of osimertinib AUC and Cmax was 63.3% (47.3, 84.5) and 51.4% (36.6, 72.3) in patients with mild hepatic impairment and 68.4% (49.6, 94.2) and 60.7% (41.6, 88.6) in patients with moderate hepatic impairment; for the metabolite AZ5104 the AUC and Cmax were 66.5% (43.4, 101.9) and 66.3% (45.3, 96.9) in patients with mild hepatic impairment and 50.9% (31.7, 81.6) and 44.0% (28.9, 67.1) in patients with moderate hepatic impairment, compared to the exposure in patients with normal hepatic function. Based on population PK analysis, there was no relationship between markers of hepatic function (ALT, AST, bilirubin) and osimertinib exposure. The hepatic impairment marker serum albumin showed an effect on the PK of osimertinib. Clinical studies that were conducted excluded patients with AST or ALT >2.5x upper limit of normal (ULN), or if due to underlying malignancy, >5.0x ULN or with total bilirubin >1.5x ULN. Based on a pharmacokinetic analysis of 134 patients with mild hepatic impairment, 8 patients with moderate hepatic impairment and 1216 patients with normal hepatic function osimertinib exposures were similar. There are no data available on patients with severe hepatic impairment (see section 4.2). Renal impairment In a clinical study, patients with severe renal impairment (CLcr 15 to less than 30 mL/min; n=7) compared to patients with normal renal function (CLcr greater than or equal to 90 mL/min; n=8) after a single 80 mg oral dose of TAGRISSO showed a 1.85-fold increase in AUC (90% CI; 0.94, 3.64) and a 1.19-fold increase in Cmax (90% CI: 0.69, 2.07). Furthermore, based on a population pharmacokinetic analysis of 593 patients with mild renal impairment (CLcr 60 to less than 90 mL/min), 254 patients with moderate renal impairment (CLcr 30 to less than 60 mL/min),5 patients with severe renal impairment (CLcr 15 to less than 30 mL/min) and 502 patients with normal renal function (greater than or equal to 90 mL/min), osimertinib exposures were similar. Patients with CLcr less than or equal to 10 mL/min were not included in the clinical studies. Patients with brain metastases PET images following administration of microdoses of [11C]osimertinib in EGFR mutation positive NSCLC patients with brain metastases (n=4) and healthy volunteers (n=7) demonstrated that the brain to plasma ratio (Kp) was similar and that [11C]osimertinib crossed the blood brain barrier rapidly and was homogeneously distributed across all regions of the brain in both patients and healthy volunteers.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. סרטן ריאה מתקדם מקומי או גרורתי מסוג NSCLC (Non small cell lung cancer) בחולים המבטאים מוטציות פעילות מסוג EGFR בחולה שטרם קיבל טיפול במעכבי טירוזין קינאז למחלתו. 2. סרטן ריאה מתקדם מקומי או גרורתי מסוג NSCLC (Non small cell lung cancer) עם מוטציה מסוג EGFR T790M בחולה שמחלתו התקדמה במהלך או לאחר טיפול קודם במעכבי טירוזין קינאז.3. טיפול משלים בסרטן ריאה מסוג NSCLC בשלב מחלה IB-IIIA בגידולים עם מוטציות מסוג EGFR exon 19 deletions או EGFR exon 21 L858R mutations בלבד.משך הטיפול בתכשיר להתוויה זו לא יעלה על שלוש שנים. ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול משלים בסרטן ריאה מסוג NSCLC בשלב מחלה IB-IIIA בגידולים עם מוטציות מסוג EGFR exon 19 deletions או EGFR exon 21 L858R mutations בלבד. משך הטיפול בתכשיר להתוויה זו לא יעלה על שלוש שנים. | 03/02/2022 | אונקולוגיה | EGFR+ NSCLC | |
| סרטן ריאה מתקדם מקומי או גרורתי מסוג NSCLC (Non small cell lung cancer) בחולים המבטאים מוטציות פעילות מסוג EGFR בחולה שטרם קיבל טיפול במעכבי טירוזין קינאז למחלתו. | 16/01/2019 | אונקולוגיה | EGFR+ NSCLC | |
| סרטן ריאה מתקדם מקומי או גרורתי מסוג NSCLC (Non small cell lung cancer) עם מוטציה מסוג EGFR T790M בחולה שטרם קיבל טיפול במעכבי טירוזין קינאז למחלתו. | 11/01/2018 | אונקולוגיה | EGFR+ NSCLC | |
| א. התרופה תינתן לטיפול בסרטן ריאה מתקדם מקומי או גרורתי מסוג NSCLC (Non small cell lung cancer) עם מוטציה מסוג EGFR T790M שמחלתם התקדמה במהלך או לאחר טיפול קודם במעכבי טירוזין קינאז. ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה. | 21/01/2016 | אונקולוגיה | EGFR+ NSCLC |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
19.10.21 - עלון לצרכן אנגלית 21.08.22 - עלון לצרכן עברית 19.10.21 - עלון לצרכן ערבית 02.10.22 - עלון לצרכן אנגלית 07.11.22 - עלון לצרכן עברית 02.10.22 - עלון לצרכן ערבית 27.02.23 - עלון לצרכן אנגלית 27.02.23 - עלון לצרכן ערבית 20.11.23 - עלון לצרכן עברית 20.03.24 - עלון לצרכן אנגלית 20.03.24 - עלון לצרכן ערבית 11.04.24 - עלון לצרכן עברית 12.07.24 - עלון לצרכן אנגלית 12.07.24 - עלון לצרכן ערבית 15.09.19 - החמרה לעלון 17.05.20 - החמרה לעלון 05.08.20 - החמרה לעלון 17.08.20 - החמרה לעלון 28.03.21 - החמרה לעלון 20.07.21 - החמרה לעלון 29.08.21 - החמרה לעלון 21.08.22 - החמרה לעלון 07.11.22 - החמרה לעלון 06.03.23 - החמרה לעלוןלתרופה במאגר משרד הבריאות
טאגריסו 80 מ"ג