Quest for the right Drug
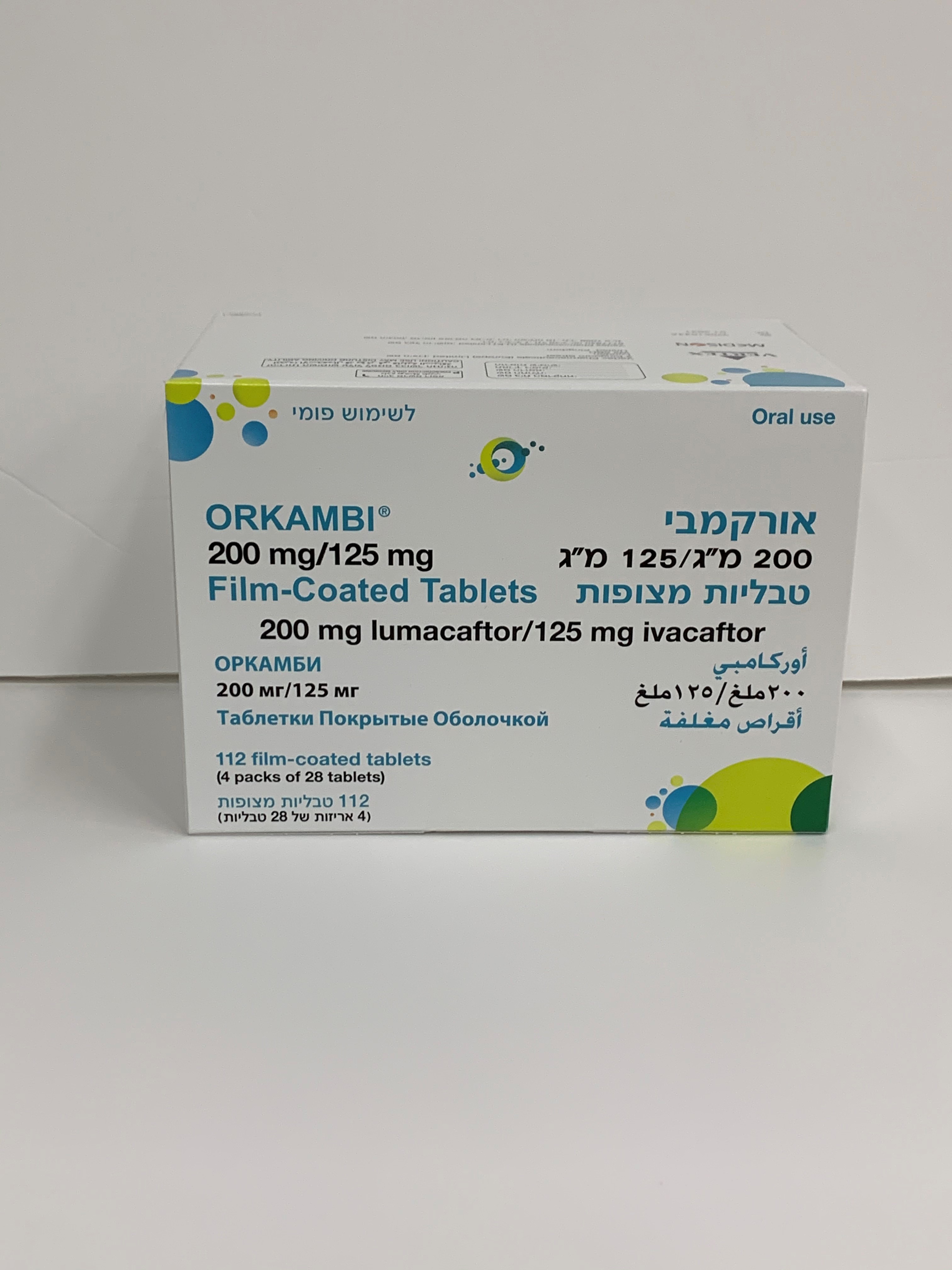
אורקמבי 200מ"ג / 125מ"ג טבליות מצופות ORKAMBI 200mg / 125mg FILM COATED TABLETS (IVACAFTOR, LUMACAFTOR)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The most common adverse reactions in Phase 3 clinical studies were dyspnoea (14.0% versus 7.8% on placebo), diarrhoea (11.0% versus 8.4% on placebo), and nausea (10.2% versus 7.6% on placebo). Serious adverse reactions included hepatobiliary events, e.g., transaminase elevations, cholestatic hepatitis and hepatic encephalopathy. Tabulated list of adverse reactions Adverse reactions identified from the 24-week, placebo-controlled, Phase 3 studies (trials 809-103 and 809-104) in patients aged 12 years and older and from a 24-week, placebo-controlled study in patients aged 6 to 11 years (trial 809-109), who are homozygous for the F508del mutation in the CFTR gene are presented in Table 4 and are listed by system organ class and frequency. Adverse reactions observed with ivacaftor alone are also provided in Table 4. Adverse reactions are ranked under the MedDRA frequency classification: very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000); and not known (frequency cannot be estimated using the available data). ORKA_100_125-200_125-SPC-0524-V1 Page 14 of 31 Table 4: Adverse reactions in lumacaftor/ivacaftor-treated patients and in patients treated with ivacaftor alone System organ class Frequency Adverse reactions Infections and infestations very common Nasopharyngitis* common Upper respiratory tract infection, rhinitis Psychiatric disorders not known Depression Vascular disorders uncommon Hypertension Nervous system disorders very common Headache, dizziness* uncommon Hepatic encephalopathy† Ear and labyrinth disorders common Ear pain*, ear discomfort*, tinnitus*, tympanic membrane hyperaemia*, vestibular disorder* uncommon Ear congestion* Respiratory, thoracic and very common Nasal congestion, dyspnoea, productive cough, mediastinal disorders sputum increased common Respiration abnormal, oropharyngeal pain, sinus congestion*, rhinorrhoea, pharyngeal erythema*, bronchospasm Gastrointestinal disorders very common Abdominal pain*, abdominal pain upper, diarrhoea, nausea common Flatulence, vomiting Hepatobiliary disorders common Transaminase elevations uncommon Cholestatic hepatitis‡ Skin and subcutaneous tissue common Rash disorders Reproductive system and common Menstruation irregular, dysmenorrhoea, breast disorders metrorrhagia, breast mass* uncommon Menorrhagia, amenorrhoea, polymenorrhoea, breast inflammation*, gynaecomastia*, nipple disorder*, nipple pain*, oligomenorrhoea Investigations very common Bacteria in sputum* common Blood creatine phosphokinase increased uncommon Blood pressure increased * Adverse reactions and frequencies observed in patients in clinical studies with ivacaftor monotherapy † 1 patient out of 738 ‡ 2 patients out of 738 The safety data from 1,029 patients aged 12 years and older who were homozygous for the F508del mutation in the CFTR gene treated with lumacaftor/ivacaftor for up to an additional 96 weeks in the long-term safety and efficacy rollover study (trial 809-105) were similar to the 24-week, placebo-controlled studies (see section 5.1). ORKA_100_125-200_125-SPC-0524-V1 Page 15 of 31 Description of selected adverse reactions Hepatobiliary adverse reactions During trials 809-103 and 809-104, the incidence of maximum transaminase (ALT or AST) levels > 8, > 5, and > 3 x ULN was 0.8%, 2.0%, and 5.2%; and 0.5%, 1.9%, and 5.1% in lumacaftor/ivacaftor- and placebo-treated patients, respectively. The incidence of transaminase-related adverse reactions was 5.1% and 4.6% in lumacaftor/ivacaftor-treated patients and those who received placebo, respectively. Seven patients who received lumacaftor/ivacaftor had liver-related serious adverse reactions with elevated transaminases, including 3 with concurrent elevation in total bilirubin. Following discontinuation of lumacaftor/ivacaftor, liver function tests returned to baseline or improved substantially in all patients (see section 4.4). Among 7 patients with pre-existing cirrhosis and/or portal hypertension who received lumacaftor/ivacaftor in the placebo-controlled, Phase 3 studies, worsening liver function with increased ALT, AST, bilirubin, and hepatic encephalopathy was observed in one patient. The event occurred within 5 days of the start of dosing and resolved following discontinuation of lumacaftor/ivacaftor (see section 4.4). Post–marketing cases of liver function decompensation including liver failure leading to death have been reported in CF patients with pre-existing cirrhosis with portal hypertension who were treated with lumacaftor/ivacaftor (see section 4.4). Respiratory adverse reactions During trials 809-103 and 809-104, the incidence of respiratory adverse reactions (e.g., chest discomfort, dyspnoea, bronchospasm, and respiration abnormal) was 26.3% in lumacaftor/ivacaftor-treated patients compared to 17.0% in patients who received placebo. The incidence of these adverse reactions was more common in patients with lower pre-treatment FEV1. Approximately three-quarters of the events began during the first week of treatment, and in most patients the events resolved without dosing interruption. The majority of adverse reactions were mild or moderate in severity, non-serious and did not result in treatment discontinuation (see section 4.4). During a 24-week, open-label, Phase 3b clinical study (trial 809-011 [Part B]) in 46 patients aged 12 years and older with advanced lung disease (ppFEV1 < 40) [mean ppFEV1 29.1 at baseline (range: 18.3 to 42.0)], the incidence of respiratory adverse reactions was 65.2%. In the subgroup of 28 patients who were initiated at the full dose of lumacaftor/ivacaftor (2 tablets every 12 hours), the incidence was 71.4%, and in the 18 patients who were initiated at a reduced dose of lumacaftor/ivacaftor (1 tablet every 12 hours for up to 2 weeks, and subsequently increased to the full dose), the incidence was 55.6%. Of the patients who were initiated lumacaftor/ivacaftor at the full dose, one patient had a serious respiratory event, three patients subsequently had their dose reduced, and three patients discontinued treatment. No serious respiratory adverse reactions, dose reductions or discontinuations were seen in patients who were initiated at the half dose (see section 4.4). Menstrual abnormalities During trials 809-103 and 809-104, the incidence of combined menstrual abnormalities (amenorrhoea, dysmenorrhoea, menorrhagia, menstruation irregular, metrorrhagia, oligomenorrhoea, and polymenorrhoea) was 9.9 % in lumacaftor/ivacaftor-treated female patients and 1.7% in placebo-treated females. These menstrual events occurred more frequently in the subset of female patients who were taking hormonal contraceptives (25.0%) versus patients who were not taking hormonal contraceptives ORKA_100_125-200_125-SPC-0524-V1 Page 16 of 31 (3.5%) (see section 4.5). Most of these reactions were mild or moderate in severity and non-serious. In lumacaftor/ivacaftor-treated patients, approximately two-thirds of these reactions resolved, and the median duration was 10 days. Increased blood pressure During trials 809-103 and 809-104, adverse reactions related to increased blood pressure (e.g., hypertension, blood pressure increased) were reported in 0.9% (7/738) of patients treated with lumacaftor/ivacaftor and in no patients who received placebo. In patients treated with lumacaftor/ivacaftor (mean baseline 114 mmHg systolic and 69 mmHg diastolic), the maximum increase from baseline in mean systolic and diastolic blood pressure was 3.1 mmHg and 1.8 mmHg, respectively. In patients who received placebo (mean baseline 114 mmHg systolic and 69 mmHg diastolic), the maximum increase from baseline in mean systolic and diastolic blood pressure was 0.9 mmHg and 0.9 mmHg, respectively. The proportion of patients who experienced a systolic blood pressure value > 140 mmHg or a diastolic blood pressure > 90 mmHg on at least two occasions was 3.4% and 1.5% in patients treated with lumacaftor/ivacaftor, respectively, compared with 1.6% and 0.5% in patients who received placebo (see section 4.4). Paediatric population Safety data were evaluated in 161 paediatric patients aged 6 to 11 years (trials 809-011and 809-109) and in 194 patients aged 12 to 17 years with CF who are homozygous for the F508del mutation and who received lumacaftor/ivacaftor in clinical studies. Patients aged 12 to 17 years were included in trials 809- 103 and 809-104. The safety profile in these paediatric patients is generally consistent with that in adult patients. Long-term safety data from a 96-week rollover extension study in 239 patients aged 6 years and older who were homozygous for the F508del mutation in the CFTR gene (trial 809-110) were generally consistent with the 24-week parent studies in patients aged 6 to 11 years (trial 809-011 and trial 809-109). Description of selected adverse reactions for patients aged 6 to 11 years Hepatobiliary adverse reactions During the 24-week, open-label Phase 3 clinical study in 58 patients aged 6 to 11 years (trial 809-011), the incidence of maximum transaminase (ALT or AST) levels > 8, > 5, and > 3 x ULN was 5.3%, 8.8%, and 19.3%. No patients had total bilirubin levels > 2 x ULN. Lumacaftor/ivacaftor dosing was maintained or successfully resumed after interruption in all patients with transaminase elevations, except 1 patient who discontinued treatment permanently. During the 24-week, placebo-controlled Phase 3 clinical study in 204 patients aged 6 to 11 years (trial 809-109), the incidence of maximum transaminase (ALT or AST) levels > 8, > 5, and > 3 x ULN was 1.0%, 4.9%, and 12.6% in the lumacaftor/ivacaftor patients, and 2.0%, 3.0%, and 7.9% in the placebo-treated patients. No patients had total bilirubin levels > 2 x ULN. Two patients in the lumacaftor/ivacaftor group and two patients in the placebo group discontinued treatment permanently due to transaminase elevations. Respiratory adverse reactions During the 24-week, open-label Phase 3 clinical study (trial 809-011) in 58 patients aged 6 to 11 years (mean baseline ppFEV1 was 91.4), the incidence of respiratory adverse reactions was 6.9% (4/58). ORKA_100_125-200_125-SPC-0524-V1 Page 17 of 31 During the 24-week, placebo-controlled Phase 3 clinical study (trial 809-109) in patients aged 6 to 11 years (mean baseline ppFEV1 was 89.8), the incidence of respiratory adverse reactions was 18.4% in lumacaftor/ivacaftor patients and 12.9% in placebo patients. A decline in ppFEV1 at initiation of therapy was observed during serial post dose spirometry assessments. The absolute change from pre-dose at 4- 6 hours post-dose was -7.7 on day 1 and -1.3 on day 15 in lumacaftor/ivacaftor patients. The post-dose decline was resolved by week 16. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בחולי לייפת כיסתית (CF- Cystic fibrosis) הומוזיגוטיים למוטציה מסוג F508del בגן CFTR. התכשיר יינתן לחולים בני שש שנים ומעלה שטרם עברו השתלת ריאה.מתן התרופה ייעשה לפי מרשם של רופא מומחה ברפואת ריאות.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
157 84 34839 00
מחיר
0 ₪
מידע נוסף
