Quest for the right Drug
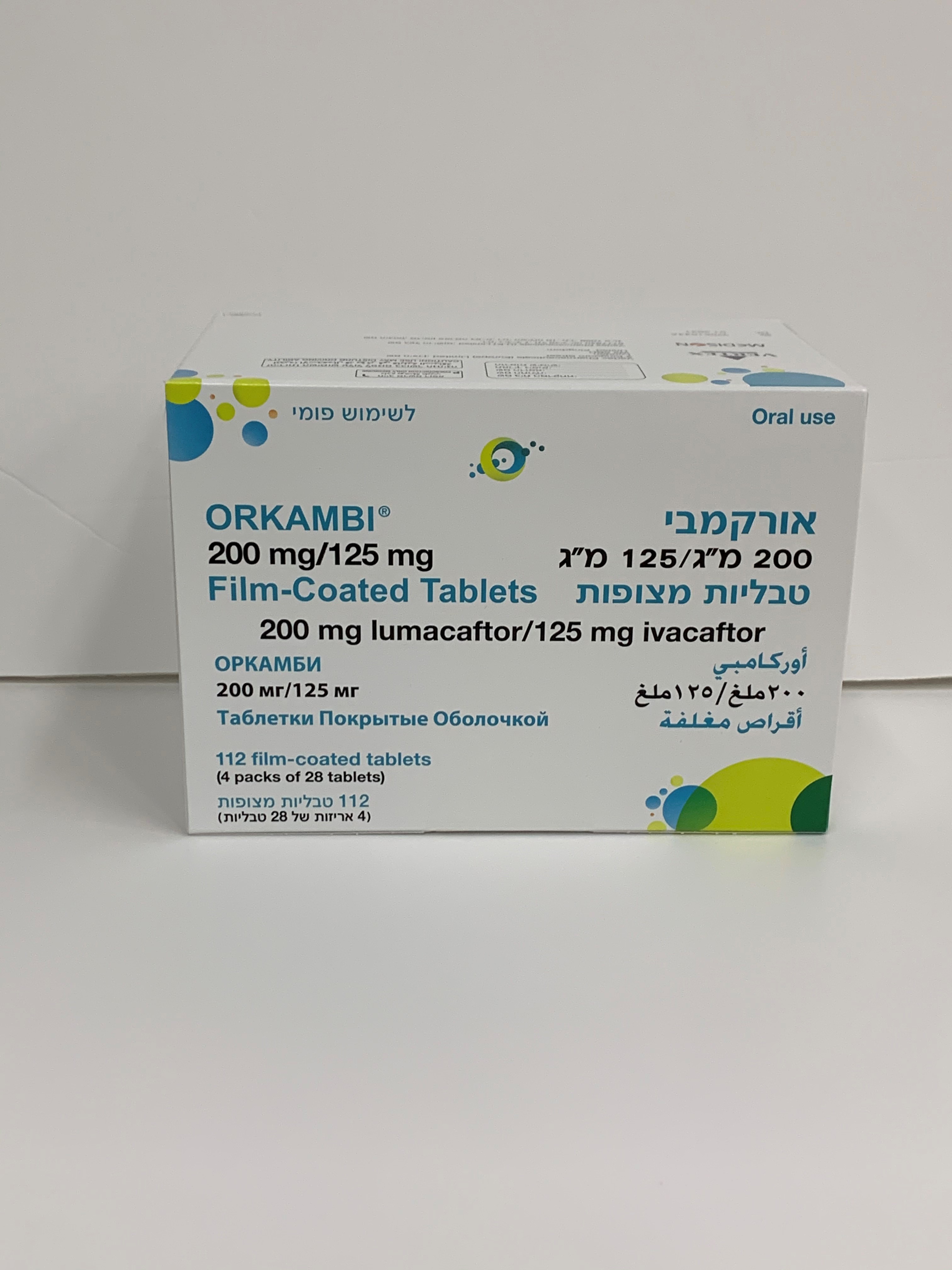
אורקמבי 200מ"ג / 125מ"ג טבליות מצופות ORKAMBI 200mg / 125mg FILM COATED TABLETS (IVACAFTOR, LUMACAFTOR)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other respiratory system products; ATC code: R07AX30 Mechanism of action The CFTR protein is a chloride channel present at the surface of epithelial cells in multiple organs. The F508del mutation impacts the CFTR protein in multiple ways, primarily by causing a defect in cellular processing and trafficking that reduces the quantity of CFTR at the cell surface. The small amount of F508del-CFTR that reaches the cell surface has low channel-open probability (defective channel gating). Lumacaftor is a CFTR corrector that acts directly on F508del-CFTR to improve its cellular processing and trafficking, thereby increasing the quantity of functional CFTR at the cell surface. Ivacaftor is a CFTR potentiator that facilitates increased chloride transport by potentiating the channel-open probability (or gating) of the CFTR protein at the cell surface. The combined effect of lumacaftor and ivacaftor is increased quantity and function of F508del-CFTR at the cell surface, resulting in increased chloride ion transport. The exact mechanisms by which lumacaftor improves cellular processing and trafficking of F508del-CFTR and ivacaftor potentiates F508del-CFTR are not known. Pharmacodynamic effects Effects on sweat chloride Changes in sweat chloride in response to lumacaftor alone or in combination with ivacaftor were evaluated in a double-blind, placebo-controlled, Phase 2 clinical trial in patients with CF age 18 years and older. In this trial, 10 patients (homozygous for F508del-CFTR mutation) completed dosing with lumacaftor alone 400 mg q12h for 28 days followed by the addition of ivacaftor 250 mg q12h for an additional 28 days, and 25 patients (homozygous or heterozygous for F508del) completed dosing with placebo. The treatment difference between lumacaftor 400 mg q12h alone and placebo evaluated as mean change in sweat chloride from baseline to day 28 was statistically significant at -8.2 mmol/L (95% CI: -14, -2). The treatment difference between the combination of lumacaftor 400 mg/ivacaftor 250 mg q12h and placebo evaluated as mean change in sweat chloride from baseline to day 56 was statistically significant at -11 mmol/L (95% CI: -18, -4). ORKA_100_125-200_125-SPC-0121-V1 Page 18 of 31 In trial 7 (see Clinical efficacy and safety) in patients homozygous for the F508del-CFTR mutation aged 6 to 11 years, the treatment difference (LS mean) in sweat chloride for the absolute change at week 24 as compared to placebo was -24.9 mmol/L (nominal P < 0.0001). The treatment difference (LS mean) in sweat chloride for the average absolute change at day 15 and at week 4 as compared to placebo was -20.8 mmol/L (95% CI: -23.4, -18.2; nominal P < 0.0001). Changes in FEV 1 Changes in ppFEV 1 in response to lumacaftor alone or in combination with ivacaftor were also evaluated in the double-blind, placebo-controlled, Phase 2 trial in patients with CF aged 18 years and older. The treatment difference between lumacaftor 400 mg q12h alone and placebo evaluated as mean absolute change in ppFEV 1 was -4.6 percentage points (95% CI: -9.6, 0.4) from baseline to day 28, 4.2 percentage points (95% CI: –1.3, 9.7) from baseline to day 56, and 7.7 percentage points (95% CI: 2.6, 12.8; statistically significant) from day 28 to day 56 (following the addition of ivacaftor to lumacaftor monotherapy). Decrease in heart rate During the 24-week, placebo-controlled, Phase 3 studies, a maximum decrease in mean heart rate of 6 beats per minute (bpm) from baseline was observed on day 1 and day 15 around 4 to 6 hours after dosing. After day 15, heart rate was not monitored in the period after dosing in these studies. From week 4, the change in mean heart rate at pre-dose ranged from 1 to 2 bpm below baseline among patients treated with lumacaftor/ivacaftor. The percentage of patients with heart rate values < 50 bpm on treatment was 11% for patients who received lumacaftor/ivacaftor, compared to 4.9% for patients who received placebo. Cardiac electrophysiology No meaningful changes in QTc interval or blood pressure were observed in a thorough QT clinical study evaluating lumacaftor 600 mg once daily/ivacaftor 250 mg q12h and lumacaftor 1000 mg once daily/ivacaftor 450 mg q12h. Clinical efficacy and safety Trials in patients with CF aged 12 years and above who are homozygous for the F508del mutation in the CFTR gene The efficacy of lumacaftor/ivacaftor in patients with CF who are homozygous for the F508del mutation in the CFTR gene was evaluated in two randomised, double-blind, placebo-controlled clinical trials of 1,108 clinically stable patients with CF, in which 737 patients were randomised to and dosed with lumacaftor/ivacaftor. Patients in both trials were randomised 1:1:1 to receive lumacaftor 600 mg once daily/ivacaftor 250 mg q12h, lumacaftor 400 mg q12h/ivacaftor 250 mg q12h, or placebo. Patients took the study drug with fat-containing food for 24 weeks in addition to their prescribed CF therapies (e.g., bronchodilators, inhaled antibiotics, dornase alfa, and hypertonic saline). Patients from these trials were eligible to roll over into a blinded extension study. Trial 1 evaluated 549 patients with CF who were aged 12 years and older (mean age 25.1 years) with percent predicted FEV 1 (ppFEV 1 ) at screening between 40-90 (mean ppFEV 1 60.7 at baseline [range: 31.1 to 94.0]). Trial 2 evaluated 559 patients aged 12 years and older (mean age 25.0 years) with ppFEV 1 at screening between 40-90 (mean ppFEV 1 60.5 at baseline [range: 31.3 to 99.8]). Patients with a history of colonisation with organisms such as Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus or who had 3 or more abnormal liver function tests (ALT, AST, AP, GGT ≥ 3 times the ULN or total bilirubin ≥ 2 times the ULN) were excluded. ORKA_100_125-200_125-SPC-0121-V1 Page 19 of 31 The primary efficacy endpoint in both studies was the absolute change from baseline in ppFEV 1 at week 24. Other efficacy variables included relative change from baseline in ppFEV 1 , absolute change from baseline in BMI, absolute change from baseline in CFQ-R Respiratory Domain the proportion of patients achieving ≥ 5% relative change from baseline in ppFEV 1 at week 24, and the number of pulmonary exacerbations (including those requiring hospitalisation or IV antibiotic therapy) through week 24. In both trials, treatment with lumacaftor/ivacaftor resulted in a statistically significant improvement in ppFEV 1 (Table 5). Mean improvement in ppFEV 1 was rapid in onset (day 15) and sustained throughout the 24-week treatment period. At day 15, the treatment difference between lumacaftor 400 mg/ivacaftor 250 mg q12h and placebo for the mean absolute change (95% CI) in ppFEV 1 from baseline was 2.51 percentage points in the pooled trials 1 and 2 (P < 0.0001). Improvements in ppFEV 1 were observed regardless of age, disease severity, sex and geographic region. The Phase 3 trials of lumacaftor/ivacaftor included 81 patients with ppFEV 1 < 40 at baseline. The treatment difference in this subgroup was comparable to that observed in patients with ppFEV 1 ≥ 40. At week-24, the treatment difference between lumacaftor 400 mg/ivacaftor 250 mg q12h and placebo for the mean absolute change (95% CI) in ppFEV 1 from baseline in the pooled trials 1 and 2 were 3.39 percentage points (P = 0.0382) for patients with ppFEV 1 < 40 and 2.47 percentage points (P < 0.0001) for patients with ppFEV 1 ≥ 40. Table 5: Summary of primary and key secondary outcomes in trial 1 and trial 2* Trial 1 Trial 2 Pooled (trial 1 and trial 2) LUM 400 mg LUM 400 mg LUM 400 mg Placebo q12h/ IVA Placebo q12h/IVA Placebo q12h/IVA (n=184) 250 mg q12h (n=187) 250 mg q12h (n=371) 250 mg q12h (n=182) (n=187) (n=369) Absolute change Treatment 2.41 2.65 2.55 in ppFEV 1 at – – – difference (P = 0.0003) † (P = 0.0011) † (P < 0.0001) week 24 (percentage Within-group -0.73 1.68 -0.02 2.63 -0.39 2.16 points) change (P = 0.2168) (P = 0.0051) (P = 0.9730) (P < 0.0001) (P < 0.3494) (P < 0.0001) Treatment 4.15 4.69 4.4 Relative change – – – difference (P = 0.0028)† (P = 0.0009)† (P < 0.0001) in ppFEV 1 at Within-group -0.85 3.3 0.16 4.85 -0.34 4.1 week 24 (%) change (P = 0.3934) (P = 0.0011) (P = 0.8793) (P < 0.0001) (P = 0.6375) (P < 0.0001) Treatment 0.13 0.36 0.24 Absolute change – – – difference (P = 0.1938) (P < 0.0001)† (P = 0.0004) in BMI at Within-group 0.19 0.32 0.07 0.43 0.13 0.37 week 24 (kg/m2) change (P = 0.0065) (P < 0.0001) (P = 0.2892) (P < 0.0001) (P = 0.0066) (P < 0.0001) Absolute change Treatment 1.5 2.9 2.2 – – – in CFQ-R difference (P = 0.3569) (P = 0.0736) (P = 0.0512) Respiratory Within-group 1.1 2.6 2.8 5.7 1.9 4.1 Domain Score at change (P = 0.3423) (P = 0.0295) (P = 0.0152) (P < 0.0001) (P = 0.0213) (P < 0.0001) week 24 (points) Proportion of % 25% 32% 26% 41% 26% 37% patients with ≥5% relative change in 1.43 1.90 1.66 Odds ratio – – – ppFEV 1 at (P = 0.1208) (P = 0.0032) (P = 0.0013) week 24 ORKA_100_125-200_125-SPC-0121-V1 Page 20 of 31 # of events Number of (rate per 48 112 (1.07) 73 (0.71) 139 (1.18) 79 (0.67) 251 (1.14) 152 (0.70) pulmonary wks) exacerbations 0.66 0.57 0.61 through week 24 Rate ratio – – – (P = 0.0169) (P = 0.0002) (P < 0.0001) * In each study, a hierarchical testing procedure was performed within each active treatment arm for primary and secondary endpoints vs. placebo; at each step, P ≤ 0.0250 and all previous tests also meeting this level of significance was required for statistical significance. † Indicates statistical significance confirmed in the hierarchical testing procedure. At week 24, the proportion of patients who remained free from pulmonary exacerbations was significantly higher for patients treated with lumacaftor/ivacaftor compared with placebo. In the pooled analysis, the rate ratio of exacerbations through week 24 in subjects treated with lumacaftor/ivacaftor (lumacaftor 400 mg/ivacaftor 250 mg q12h; n = 369) was 0.61 (P < 0.0001), representing a reduction of 39% relative to placebo. The event rate per year, annualised to 48 weeks, was 0.70 in the lumacaftor/ivacaftor group and 1.14 in the placebo group. Treatment with lumacaftor/ivacaftor significantly decreased the risk for exacerbations requiring hospitalisation versus placebo by 61% (rate ratio=0.39, P < 0.0001; event rate per 48 weeks 0.17 for lumacaftor/ivacaftor and 0.45 for placebo) and reduced exacerbations requiring treatment with intravenous antibiotics by 56% (rate ratio = 0.44, P < 0.0001; event rate per 48 weeks 0.25 for lumacaftor/ivacaftor and 0.58 for placebo). These results were not considered statistically significant within the framework of the testing hierarchy for the individual studies. Long-term safety and efficacy rollover trial Trial 3 was a Phase 3, parallel-group, multicentre, rollover extension study in patients with CF that included patients aged 12 years and older from trial 1 and trial 2. This extension trial was designed to evaluate the safety and efficacy of long-term treatment of lumacaftor/ivacaftor. Of the 1,108 patients who received any treatment in trial 1 or trial 2, 1,029 (93%) were dosed and received active treatment (lumacaftor 600 mg once daily/ivacaftor 250 mg q12h or lumacaftor 400 mg q12h/ivacaftor 250 mg q12h) in trial 3 for up to an additional 96 weeks (i.e. up to a total of 120 weeks). The primary efficacy analysis of this extension study included data up to week 72 of trial 3 with a sensitivity analysis that included data up to week 96 of trial 3. Patients treated with lumacaftor/ivacaftor in trial 1 or trial 2 showed an effect that was maintained with respect to baseline after an additional 96 weeks through trial 3. For patients who transitioned from placebo to active treatment similar changes as those observed in patients treated with lumacaftor/ivacaftor in trial 1 or trial 2 were seen (see Table 5). Results from trial 3 are presented in Figure 1 and Table 6. ORKA_100_125-200_125-SPC-0121-V1 Page 21 of 31 Figure 1. Absolute change from baseline in percent predicted FEV 1 at each visit† † From trials 1, 2 and 3. ORKA_100_125-200_125-SPC-0121-V1 Page 22 of 31 Table 6: Long-term effect of Lumacaftor/Ivacaftor in trial 3* Placebo transitioned to Lumacaftor 400 mg q12h/ Lumacaftor 400 mg q12h/ Ivacaftor 250 mg q12h Ivacaftor 250 mg q12h (n = 176)** (n = 369)† LS Means LS Means Baseline and Endpoint Mean (SD) (95% CI) P value Mean (SD) (95% CI) P value Baseline ppFEV1‡ 60.2 (14.7) 60.5 (14.1) Absolute change from baseline ppFEV1 (percentage points) (n = 134) (n = 273) Extension week 72 1.5 0.0254 0.5 0.2806 (0.2, 2.9) (-0.4, 1.5) (n = 75) (n = 147) Extension week 96 0.8 0.3495 0.5 0.4231 (-0.8, 2.3) (-0.7, 1.6) Relative change from baseline ppFEV1 (%) (n = 134) (n = 273) Extension week 72 2.6 0.0332 1.4 0.1074 (0.2, 5.0) (-0.3, 3.2) (n = 75) (n = 147) Extension week 96 1.1 0.4415 1.2 0.2372 (-1.7, 3.9) (-0.8, 3.3) Baseline BMI (kg/m2)‡ 20.9 (2.8) 21.5 (3.0) Absolute change from baseline in BMI (kg/m2) (n = 145) (n = 289) Extension week 72 0.62 < 0.0001 0.69 < 0.0001 (0.45, 0.79) (0.56, 0.81) (n = 80) (n = 155) Extension week 96 0.76 < 0.0001 0.96 < 0.0001 (0.56, 0.97) (0.81, 1.11) Baseline CFQ-R 70.4 (18.5) 68.3 (18.0) Respiratory Domain Score (points)‡ Absolute change in CFQ-R Respiratory Domain Score (points) (n = 135) (n = 269) Extension week 72 3.3 0.0124 5.7 < 0.0001 (0.7, 5.9) (3.8, 7.5) (n = 81) (n = 165) Extension week 96 0.5 0.7665 3.5 0.0018 (-2.7, 3.6) (1.3, 5.8) Number of Pulmonary exacerbations (events) ** † *** Number of events per patient- 0.69 0.65 year (95% CI) (rate per 48 (0.56, 0.85) (0.56, 0.75) wks) Number of events requiring 0.30 0.24 hospitalization per patient- (0.22, 0.40) (0.19, 0.29) year (95% CI) (rate per 48 wks) ORKA_100_125-200_125-SPC-0121-V1 Page 23 of 31 Number of events requiring 0.37 0.32 intravenous antibiotics per (0.29, 0.49) (0.26, 0.38) patient-year (95% CI) (rate per 48 wks) * A total of 82% (421 of 516 eligible patients) completed 72 weeks of this study; 42% completed 96 weeks. Majority of patients discontinued for reasons other than safety. ** For patients rolled over from trials 1 and 2 (placebo-to-lumacaftor/ivacaftor group) total exposure was up to 96 weeks. Presentation of the lumacaftor 400 mg q12h/ivacaftor 250 mg q12h dose group is consistent with recommended posology. *** The event rate per patient-year was annualised to 48 weeks. † For patients rolled over from trials 1 and 2 (lumacaftor/ivacaftor-to-lumacaftor/ivacaftor group) total exposure was up to 120 weeks. Presentation of the lumacaftor 400 mg q12h/ivacaftor 250 mg q12h dose group is consistent with recommended posology. ‡ Baseline for the placebo transitioned to lumacaftor 400 mg q12h/ivacaftor 250 mg q12h group was the trial 3 baseline. Baseline for the lumacaftor 400 mg q12h/ivacaftor 250 mg q12h group was the trial 1 and 2 baseline. Trial in patients with CF who are heterozygous for the F508del mutation in the CFTR gene Trial 4 was a multicentre, double–blind, randomised, placebo–controlled, Phase 2 trial in 125 patients with CF aged 18 years and older who had a ppFEV 1 of 40 to 90, inclusive, and have the F508del mutation on one allele plus a second allele with a mutation predicted to result in the lack of CFTR production or a CFTR that is not responsive to ivacaftor in vitro. Patients received either lumacaftor/ivacaftor (n = 62) or placebo (n = 63) in addition to their prescribed CF therapies. The primary endpoint was improvement in lung function as determined by the mean absolute change from baseline at day 56 in ppFEV 1 . Treatment with lumacaftor/ivacaftor resulted in no significant improvement in ppFEV 1 relative to placebo in patients with CF heterozygous for the F508del mutation in the CFTR gene (treatment difference 0.60 [P = 0.5978]) and no meaningful improvements in BMI or weight (see section 4.4). Trials in patients with CF aged 6 to 11 years old who are homozygous for the F508del mutation in the CFTR gene Trial 7 was a 24-week, placebo-controlled, Phase 3 clinical study in 204 patients with CF aged 6 to 11 years old (mean age 8.8 years). Trial 7 evaluated subjects with lung clearance index (LCI 2.5 ) ≥ 7.5 at the initial screening visit (mean LCI 2.5 10.28 at baseline [range: 6.55 to 16.38]) and ppFEV 1 ≥ 70 at screening (mean ppFEV 1 89.8 at baseline [range: 48.6 to 119.6]). Patients received either lumacaftor 200 mg/ivacaftor 250 mg every 12 hours (n = 103) or placebo (n = 101) in addition to their prescribed CF therapies. Patients who had 2 or more abnormal liver function tests (ALT, AST, AP, GGT ≥ 3 times the ULN), or ALT or AST > 5 times ULN, or total bilirubin > 2 times ULN were excluded. The primary efficacy endpoint was absolute change in LCI 2.5 from baseline through week 24. Key secondary endpoints included average absolute change from baseline in sweat chloride at day 15 and week 4 and at week 24 (see Pharmacodynamic effects), absolute change from baseline in BMI at week 24, absolute change from baseline in CFQ-R Respiratory Domain through week 24. These results are presented in Table 7 below: ORKA_100_125-200_125-SPC-0121-V1 Page 24 of 31 Table 7: Summary of primary and key secondary outcomes in trial 7 LUM 200 mg/IVA Placebo 250 mg q12h (n = 101) (n = 103) Primary Endpoint Absolute change in lung -1.09 clearance index (LCI 2.5 ) from Treatment difference – (P < 0.0001) baseline through week 24 0.08 Within-group change -1.01 (P < 0.0001) (P = 0.5390) Key Secondary Endpoints* Absolute change in BMI at 0.11 week 24 (kg/m2) Treatment difference – (P = 0.2522) 0.27 0.38 Within-group change (P = 0.0002) (P < 0.0001) Absolute change in CFQ-R 2.5 Treatment difference – Respiratory Domain Score (P = 0.0628) through week 24 (points) 3.0 5.5 Within-group change (P = 0.0035) (P < 0.0001) * Trial included key secondary and other secondary endpoints. Percent predicted FEV 1 was also evaluated as a clinically meaningful other secondary endpoint. In the lumacaftor/ivacaftor patients, the treatment difference for absolute change in ppFEV 1 from baseline through week 24 was 2.4 (P = 0.0182). Patients with CF aged 6 years and older from trial 6 and trial 7 were included in a phase 3, multicentre, rollover extension study (trial 9). This extension trial was designed to evaluate the safety and efficacy of long-term treatment of lumacaftor/ivacaftor. Of the 262 patients who received any treatment in trial 6 or trial 7, 239 (91%) were dosed and received active treatment (patients 6 to < 12 years of age received lumacaftor 200 mg q12h/ivacaftor 250 mg q12h; patients ≥ 12 years of age received lumacaftor 400 mg q12h/ivacaftor 250 mg q12h) in the extension study for up to an additional 96 weeks (i.e., up to a total of 120 weeks) (see section 4.8). Secondary efficacy results and pulmonary exacerbation event rate per patient year are presented in Table 8. ORKA_100_125-200_125-SPC-0121-V1 Page 25 of 31 Table 8: Long-term effect of lumacaftor/ivacaftor in trial 9 Placebo transitioned to Lumacaftor / ivacaftor – lumacaftor / ivacaftor lumacaftor / ivacaftor (P-L/I) (L/I-L/I) (n = 96)* (n = 143)* LS Mean LS Mean Baseline and endpoint Mean (SD) (95% CI) Mean (SD) (95% CI) n = 101 n = 128 Baseline LCI 2.5 ‡** 10.26 (2.24) 10.24 (2.42) Absolute change from baseline in LCI 2.5 (n = 69) (n = 88) Extension week 96 -0.86 -0.85 (-1.33, -0.38) (-1.25, -0.45) n = 101 n = 161 Baseline BMI (kg/m2)‡ 16.55 (1.96) 16.56 (1.77) Absolute change from baseline in BMI (kg/m2) (n = 83) (n =130) Extension week 96 2.04 1.78 (1.77, 2.31) (1.56, 1.99) n = 78 n = 135 Baseline CFQ-R‡ Respiratory 77.1 78.5 Domain Score (points) (15.5) (14.3) Absolute change in CFQ-R Respiratory Domain Score (points) (n = 65) (n = 108) Extension week 96 6.6 7.4 (3.1, 10.0) (4.8, 10.0) Number of pulmonary exacerbations (events) (trial 7 FAS and ROS)† n = 96 n = 103 Number of events per patient- year 0.30 0.45 (95% CI) (0.21, 0.43) (0.33, 0.61) *Subjects treated with placebo in trial 7 (n=96) and transitioned onto active LUM/IVA treatment in the extension study (P-L/I). Subjects treated with LUM/IVA in either parent study [trial 6 (n=49) or trial 7 (n=94)] and continued active LUM/IVA treatment in the extension (L/I-L/I). ‡Baseline for both groups (P-L/I and L/I-L/I) was the trial 6 and trial 7 (parent study) baseline and the corresponding n refers to the analysis set in the parent study. **The LCI sub-study included 117 subjects in the L/I-L/I group and 96 subjects in the P-L/I group. †FAS = full analysis set (n=103) includes subjects who received L/I in trial 7 and in trial 9, assessed over the cumulative study period for L/I; ROS = rollover set (n=96) includes subjects who received placebo in trial 7 and L/I in trial 9, assessed over the current study period in for trial 9. ORKA_100_125-200_125-SPC-0121-V1 Page 26 of 31
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The exposure (AUC) of lumacaftor is approximately 2-fold higher in healthy adult volunteers compared to exposure in patients with CF. The exposure of ivacaftor is similar between healthy adult volunteers and patients with CF. After twice-daily dosing, steady-state plasma concentrations of lumacaftor and ivacaftor in healthy subjects were generally reached after approximately 7 days of treatment, with an accumulation ratio of approximately 1.9 for lumacaftor. The steady-state exposure of ivacaftor is lower than that of day 1 due to the CYP3A induction effect of lumacaftor (see section 4.5). After oral administration of lumacaftor 400 mg q12h/ivacaftor 250 mg q12h in a fed state, the steady-state mean (± SD) for AUC 0-12h and C max were 198 (64.8) µg∙hr/mL and 25.0 (7.96) µg/mL for lumacaftor, respectively, and 3.66 (2.25) µg∙hr/mL and 0.602 (0.304) µg/mL for ivacaftor, respectively. After oral administration of ivacaftor alone as 150 mg q12h in a fed state, the steady-state mean (± SD) for AUC 0-12h and C max were 9.08 (3.20) µg∙hr/mL and 1.12 (0.319) µg/mL, respectively. Absorption Following multiple oral doses of lumacaftor, the exposure of lumacaftor generally increased proportional to dose over the range of 50 mg to 1000 mg every 24 hours. The exposure of lumacaftor increased approximately 2.0-fold when given with fat-containing food relative to fasted conditions. The median (range) t max of lumacaftor is approximately 4.0 hours (2.0; 9.0) in the fed state. Following multiple oral dose administration of ivacaftor in combination with lumacaftor, the exposure of ivacaftor generally increased with dose from 150 mg every 12 hours to 250 mg every 12 hours. The exposure of ivacaftor when given in combination with lumacaftor increased approximately 3-fold when given with fat-containing food in healthy volunteers. Therefore, lumacaftor/ivacaftor should be administered with fat-containing food. The median (range) t max of ivacaftor is approximately 4.0 hours (2.0; 6.0) in the fed state. Distribution Lumacaftor is approximately 99% bound to plasma proteins, primarily to albumin. After oral administration of 400 mg every 12 hours in patients with CF in a fed state, the typical apparent volumes of distribution for the central and peripheral compartments [coefficient of variation as a percentage (CV)] were estimated to be 23.5 L (48.7%) and 33.3 L (30.5%), respectively. Ivacaftor is approximately 99% bound to plasma proteins, primarily to alpha 1-acid glycoprotein and albumin. After oral administration of ivacaftor 250 mg every 12 hours in combination with lumacaftor, the typical apparent volumes of distribution for the central and peripheral compartments (CV) were estimated to be 95.0 L (53.9%) and 201 L (26.6%), respectively. In vitro studies indicate that lumacaftor is a substrate of Breast Cancer Resistance Protein (BCRP). Biotransformation Lumacaftor is not extensively metabolised in humans, with the majority of lumacaftor excreted unchanged in the faeces. In vitro and in vivo data indicate that lumacaftor is mainly metabolised via oxidation and glucuronidation. ORKA_100_125-200_125-SPC-0121-V1 Page 27 of 31 Ivacaftor is extensively metabolised in humans. In vitro and in vivo data indicate that ivacaftor is primarily metabolised by CYP3A. M1 and M6 are the two major metabolites of ivacaftor in humans. M1 has approximately one-sixth the potency of ivacaftor and is considered pharmacologically active. M6 has less than one-fiftieth the potency of ivacaftor and is not considered pharmacologically active. Elimination Following oral administration of lumacaftor, the majority of lumacaftor (51%) is excreted unchanged in the faeces. There was negligible urinary excretion of lumacaftor as unchanged drug. The apparent terminal half-life is approximately 26 hours. The typical apparent clearance, CL/F (CV), of lumacaftor was estimated to be 2.38 L/hr (29.4%) for patients with CF. Following oral administration of ivacaftor alone, the majority of ivacaftor (87.8%) is eliminated in the faeces after metabolic conversion. There was negligible urinary excretion of ivacaftor as unchanged drug. In healthy subjects, the half-life of ivacaftor when given with lumacaftor is approximately 9 hours. The typical CL/F (CV) of ivacaftor when given in combination with lumacaftor was estimated to be 25.1 L/hr (40.5%) for patients with CF. Special populations Hepatic impairment Following multiple doses of lumacaftor/ivacaftor for 10 days, subjects with moderately impaired hepatic function (Child-Pugh Class B, score 7 to 9) had higher exposures (AUC 0-12hr by approximately 50% and C max by approximately 30%) compared with healthy subjects matched for demographics. The impact of mild hepatic impairment (Child-Pugh Class A, score 5 to 6) on pharmacokinetics of lumacaftor given in combination with ivacaftor has not been studied, but the increase in exposure is expected to be less than 50%. Studies have not been conducted in patients with severe hepatic impairment (Child-Pugh Class C, score 10 to 15), but exposure is expected to be higher than in patients with moderate hepatic impairment (see sections 4.2, 4.4, and 4.8). Renal impairment Pharmacokinetic studies have not been performed with lumacaftor/ivacaftor in patients with renal impairment. In a human pharmacokinetic study with lumacaftor alone, there was minimal elimination of lumacaftor and its metabolites in urine (only 8.6% of total radioactivity was recovered in the urine with 0.18% as unchanged parent). In a human pharmacokinetic study with ivacaftor alone, there was minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine). A population pharmacokinetic analysis of clearance versus creatinine clearance shows no trend for subjects with mild and moderate renal impairment (see section 4.2). Elderly The safety and efficacy of lumacaftor/ivacaftor in patients age 65 years or older have not been evaluated. Gender The effect of gender on lumacaftor pharmacokinetics was evaluated using a population pharmacokinetics analysis of data from clinical studies of lumacaftor given in combination with ivacaftor. Results indicate ORKA_100_125-200_125-SPC-0121-V1 Page 28 of 31 no clinically relevant difference in pharmacokinetic parameters for lumacaftor or ivacaftor between males and females. No dose adjustments are necessary based on gender. Paediatric population The exposures are similar between adults and the paediatric population based on population (PK) analyses as presented in Table 9: Table 9: Mean (SD) lumacaftor and ivacaftor exposure by age group Mean ivacaftor Mean lumacaftor (SD) Age group Dose (SD) AUCss AUCss (μg/mL*h) (μg/mL*h) Patients aged 6 to lumacaftor 200 mg/ivacaftor 203 (57.4) 5.26 (3.08) 11 years 250 mg every 12 hours Patients aged 12 to less lumacaftor 400 mg/ivacaftor 241 (61.4) 3.90 (1.56) than 18 years 250 mg every 12 hours

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בחולי לייפת כיסתית (CF- Cystic fibrosis) הומוזיגוטיים למוטציה מסוג F508del בגן CFTR. התכשיר יינתן לחולים בני שש שנים ומעלה שטרם עברו השתלת ריאה.מתן התרופה ייעשה לפי מרשם של רופא מומחה ברפואת ריאות.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
11/01/2018
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
157 84 34839 00
מחיר
0 ₪
מידע נוסף
