Quest for the right Drug
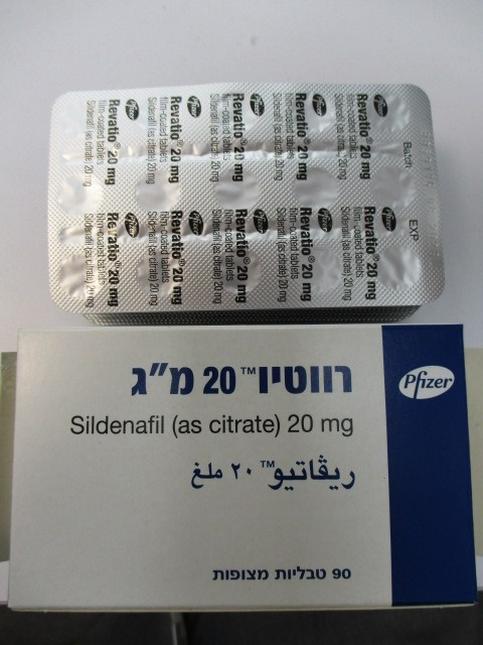
רווטיו REVATIO (SILDENAFIL AS CITRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Urologicals, Drugs used in erectile dysfunction, ATC code: G04BE03 Mechanism of action Sildenafil is a potent and selective inhibitor of cyclic guanosine monophosphate (cGMP) specific phosphodiesterase type 5 (PDE5), the enzyme that is responsible for degradation of cGMP. Apart from the presence of this enzyme in the corpus cavernosum of the penis, PDE5 is also present in the pulmonary vasculature. Sildenafil, therefore, increases cGMP within pulmonary vascular smooth muscle cells resulting in relaxation. In patients with pulmonary arterial hypertension this can lead to vasodilation of the pulmonary vascular bed and, to a lesser degree, vasodilatation in the systemic circulation. Pharmacodynamic effects Studies in vitro have shown that sildenafil is selective for PDE5. Its effect is more potent on PDE5 than on other known phosphodiesterases. There is a 10-fold selectivity over PDE6 which is involved in the phototransduction pathway in the retina. There is an 80-fold selectivity over PDE1, and over 700-fold over PDE 2, 3, 4, 7, 8, 9, 10 and 11. In particular, sildenafil has greater than 4,000-fold selectivity for PDE5 over PDE3, the cAMP-specific phosphodiesterase isoform involved in the control of cardiac contractility. Sildenafil causes mild and transient decreases in systemic blood pressure which, in the majority of cases, do not translate into clinical effects. After chronic dosing of 80 mg three times a day to patients with systemic hypertension the mean change from baseline in systolic and diastolic blood pressure was a decrease of 9.4 mmHg and 9.1 mm Hg respectively. After chronic dosing of 80 mg three times a day to patients with pulmonary arterial hypertension lesser effects in blood pressure reduction were observed (a reduction in both systolic and diastolic pressure of 2 mmHg). At the recommended dose of 20 mg three times a day no reductions in systolic or diastolic pressure were seen. Single oral doses of sildenafil up to 100 mg in healthy volunteers produced no clinically relevant effects on ECG. After chronic dosing of 80 mg three times a day to patients with pulmonary arterial hypertension no clinically relevant effects on the ECG were reported. In a study of the hemodynamic effects of a single oral 100 mg dose of sildenafil in 14 patients with severe coronary artery disease (CAD) (> 70 % stenosis of at least one coronary artery), the mean resting systolic and diastolic blood pressures decreased by 7 % and 6 % respectively compared to baseline. Mean pulmonary systolic blood pressure decreased by 9 %. Sildenafil showed no effect on cardiac output, and did not impair blood flow through the stenosed coronary arteries. Mild and transient differences in colour discrimination (blue/green) were detected in some subjects using the Farnsworth-Munsell 100 hue test at 1 hour following a 100 mg dose, with no effects evident after 2 hours post-dose. The postulated mechanism for this change in colour discrimination is related to inhibition of PDE6, which is involved in the phototransduction cascade of the retina. Sildenafil has no effect on visual acuity or contrast sensitivity. In a small size placebo-controlled study of patients with documented early age-related macular degeneration (n = 9), sildenafil (single dose, 100 mg) demonstrated no significant changes in visual tests conducted (visual acuity, Amsler grid, colour discrimination simulated traffic light, Humphrey perimeter and photostress). Clinical efficacy and safety Efficacy in adult patients with pulmonary arterial hypertension (PAH) A randomised, double-blind, placebo-controlled study was conducted in 278 patients with primary pulmonary hypertension, PAH associated with connective tissue disease, and PAH following surgical repair of congenital heart lesions. Patients were randomised to one of four treatment groups: placebo, sildenafil 20 mg, sildenafil 40 mg or sildenafil 80 mg, three times a day. Of the 278 patients randomised, 277 patients received at least 1 dose of study drug. The study population consisted of 68 (25 %) men and 209 (75 %) women with a mean age of 49 years (range: 18-81 years) and baseline 6-minute walk test distance between 100 and 450 metres inclusive (mean: 344 metres). 175 patients (63%) included were diagnosed with primary pulmonary hypertension, 84 (30%) were diagnosed with PAH associated with connective tissue disease and 18 (7%) of the patients were diagnosed with PAH following surgical repair of congenital heart lesions. Most patients were WHO Functional Class II (107/277, 39%) or III (160/277, 58%) with a mean baseline 6 minute walking distance of 378 meters and 326 meters respectively; fewer patients were Class I (1/277, 0.4%) or IV (9/277, 3%) at baseline. Patients with left ventricular ejection fraction < 45 % or left ventricular shortening fraction < 0.2 were not studied. Sildenafil (or placebo) was added to patients' background therapy which could have included a combination of anticoagulation, digoxin, calcium channel blockers, diuretics or oxygen. The use of prostacyclin, prostacyclin analogues and endothelin receptor antagonists was not permitted as add-on therapy, and neither was arginine supplementation. Patients who previously failed bosentan therapy were excluded from the study. The primary efficacy endpoint was the change from baseline at week 12 in 6-minute walk distance (6MWD). A statistically significant increase in 6MWD was observed in all 3 sildenafil dose groups compared to those on placebo. Placebo corrected increases in 6MWD were 45 metres (p < 0.0001), 46 metres (p < 0.0001) and 50 metres (p < 0.0001) for sildenafil 20 mg, 40 mg and 80 mg TID respectively. There was no significant difference in effect between sildenafil doses. For patients with a baseline 6MWD < 325 m improved efficacy was observed with higher doses (placebo-corrected improvements of 58 metres, 65 metres and 87 metres for 20 mg, 40 mg and 80 mg doses TID, respectively). When analysed by WHO functional class, a statistically significant increase in 6MWD was observed in the 20 mg dose group. For class II and class III, placebo corrected increases of 49 metres (p = 0.0007) and 45 metres (p = 0.0031) were observed respectively. The improvement in 6MWD was apparent after 4 weeks of treatment and this effect was maintained at weeks 8 and 12. Results were generally consistent in subgroups according to aetiology (primary and connective tissue disease -associated PAH), WHO functional class, gender, race, location, mean PAP and PVRI. Patients on all sildenafil doses achieved a statistically significant reduction in mean pulmonary arterial pressure (mPAP) and pulmonary vascular resistance (PVR) compared to those on placebo. Placebo-corrected treatment effects with mPAP were –2.7 mmHg (p = 0.04), -3.0 mm Hg (p = 0.01) and -5.1 mm Hg (p < 0.0001) for sildenafil 20 mg, 40 mg and 80 mg TID respectively. Placebo-corrected treatment effects with PVR were -178 dyne.sec/cm5 (p=0.0051), -195 dyne.sec/cm5 (p=0.0017) and -320 dyne.sec/cm5 (p<0.0001) for sildenafil 20 mg, 40 mg and 80 mg TID, respectively. The percent reduction at 12 weeks for sildenafil 20 mg, 40 mg and 80 mg TID in PVR (11.2 %, 12.9 %, 23.3 %) was proportionally greater than the reduction in systemic vascular resistance (SVR) (7.2 %, 5.9 %, 14.4 %). The effect of sildenafil on mortality is unknown. A greater percentage of patients on each of the sildenafil doses (i.e. 28 %, 36 % and 42 % of subjects who received sildenafil 20 mg, 40 mg and 80 mg TID doses, respectively) showed an improvement by at least one WHO functional class at week 12 compared to placebo (7 %). The respective odds ratios were 2.92 (p=0.0087), 4.32 (p=0.0004) and 5.75 (p<0.0001). Long-term survival data in naive population Patients enrolled into the pivotal study were eligible to enter a long term open label extension study. At 3 years 87 % of the patients were receiving a dose of 80 mg TID. A total of 207 patients were treated with Revatio in the pivotal study, and their long term survival status was assessed for a minimum of 3 years. In this population, Kaplan-Meier estimates of 1, 2 and 3 year survival were 96 %, 91 % and 82 %, respectively. Survival in patients of WHO functional class II at baseline at 1, 2 and 3 years was 99 %, 91 %, and 84 % respectively, and for patients of WHO functional class III at baseline was 94 %, 90 %, and 81 %, respectively. Efficacy in adult patients with PAH (when used in combination with epoprostenol) A randomised, double-blind, placebo controlled study was conducted in 267 patients with PAH who were stabilised on intravenous epoprostenol. The PAH patients included those with Primary Pulmonary Arterial Hypertension (212/267, 79 %) and PAH associated with connective tissue disease (55/267, 21 %). Most patients were WHO Functional Class II (68/267, 26 %) or III (175/267, 66 %); fewer patients were Class I (3/267, 1 %) or IV (16/267, 6 %) at baseline; for a few patients (5/267, 2 %), the WHO Functional Class was unknown. Patients were randomised to placebo or sildenafil (in a fixed titration starting from 20 mg, to 40 mg and then 80 mg, three times a day as tolerated) when used in combination with intravenous epoprostenol. The primary efficacy endpoint was the change from baseline at week 16 in 6-minute walk distance. There was a statistically significant benefit of sildenafil compared to placebo in 6-minute walk distance. A mean placebo corrected increase in walk distance of 26 metres was observed in favour of sildenafil (95% CI: 10.8, 41.2) (p = 0.0009). For patients with a baseline walking distance ≥ 325 metres, the treatment effect was 38.4 metres in favour of sildenafil; for patients with a baseline walking distance < 325 metres, the treatment effect was 2.3 metres in favour of placebo. For patients with primary PAH, the treatment effect was 31.1 metres compared to 7.7 metres for patients with PAH associated with connective tissue disease. The difference in results between these randomisation subgroups may have arisen by chance in view of their limited sample size. Patients on sildenafil achieved a statistically significant reduction in mean Pulmonary Arterial Pressure (mPAP) compared to those on placebo. A mean placebo-corrected treatment effect of -3.9 mmHg was observed in favour of sildenafil (95% CI: -5.7, -2.1) (p = 0.00003). Time to clinical worsening was a secondary endpoint as defined as the time from randomisation to the first occurrence of a clinical worsening event (death, lung transplantation, initiation of bosentan therapy, or clinical deterioration requiring a change in epoprostenol therapy). Treatment with sildenafil significantly delayed the time to clinical worsening of PAH compared to placebo (p = 0.0074). 23 subjects experienced clinical worsening events in the placebo group (17.6 %) compared with 8 subjects in the sildenafil group (6.0 %). Long-term Survival Data in the background epoprostenol study Patients enrolled into the epoprostenol add-on therapy study were eligible to enter a long term open label extension study. At 3 years 68 % of the patients were receiving a dose of 80 mg TID. A total of 134 patients were treated with Revatio in the initial study, and their long term survival status was assessed for a minimum of 3 years. In this population, Kaplan-Meier estimates of 1, 2 and 3 year survival were 92 %, 81 % and 74 %, respectively. Efficacy and safety in adult patients with PAH (when used in combination with bosentan) A randomized, double-blind, placebo controlled study was conducted in 103 clinically stable subjects with PAH (WHO FC II and III) who were on bosentan therapy for a minimum of three months. The PAH patients included those with primary PAH, and PAH associated with connective tissue disease. Patients were randomized to placebo or sildenafil (20 mg three times a day) in combination with bosentan (62.5-125 mg twice a day). The primary efficacy endpoint was the change from baseline at Week 12 in 6MWD. The results indicate that there is no significant difference in mean change from baseline on 6MWD observed between sildenafil (20 mg three times a day) and placebo (13.62 m (95% CI: -3.89 to 31.12) and 14.08 m (95% CI: -1.78 to 29.95), respectively). Differences in 6MWD were observed between patients with primary PAH and PAH associated with connective tissue disease. For subjects with primary PAH (67 subjects), mean changes from baseline were 26.39 m (95% CI: 10.70 to 42.08) and 11.84 m (95% CI: -8.83 to 32.52) for the sildenafil and placebo groups, respectively. However, for subjects with PAH associated with connective tissue disease (36 subjects) mean changes from baseline were - 18.32 m (95% CI: -65.66 to 29.02) and 17.50 m (95% CI: -9.41 to 44.41) for the sildenafil and placebo groups, respectively. Overall, the adverse events were generally similar between the two treatment groups (sildenafil plus bosentan vs. bosentan alone), and consistent with the known safety profile of sildenafil when used as monotherapy (see sections 4.4 and 4.5). Effects on mortality in adults with PAH A study to investigate the effects of different dose levels of sildenafil on mortality in adults with PAH was conducted following the observation of a higher risk of mortality in paediatric patients taking a high dose of sildenafil TID, based on body weight, compared to those taking a lower dose in the long-term extension of the paediatric clinical trial (see below Paediatric population - Pulmonary arterial hypertension - Long term extension data). The study was a randomized, double-blind, parallel-group study in 385 adults with PAH. Patients were randomly assigned 1:1:1 to one of three dosage groups (5 mg TID (4 times lower than the recommended dose), 20 mg TID (recommended dose) and 80 mg TID (4 times the recommended dose)). In total, the majority of subjects were PAH treatment naïve (83.4%). For most subjects the etiology of PAH was idiopathic (71.7%). The most common WHO Functional Class was Class III (57.7% of subjects). All three treatment groups were well balanced with respect to baseline demographics of strata history of PAH-treatment and etiology of PAH, as well as the WHO Functional Class categories. The mortality rates were 26.4% (n=34) for the 5 mg TID dose, 19.5% (n=25) for the 20 mg TID dose and 14.8% (n=19) with the 80 mg TID dose.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Sildenafil is rapidly absorbed. Maximum observed plasma concentrations are reached within 30 to 120 minutes (median 60 minutes) of oral dosing in the fasted state. The mean absolute oral bioavailability is 41 % (range 25-63 %). After oral three times a day dosing of sildenafil, AUC and Cmax increase in proportion with dose over the dose range of 20-40 mg. After oral doses of 80 mg three times a day a more than dose proportional increase in sildenafil plasma levels has been observed. In pulmonary arterial hypertension patients, the oral bioavailability of sildenafil after 80 mg three times a day was on average 43 % (90 % CI: 27 % - 60 %) higher compared to the lower doses. When sildenafil is taken with food, the rate of absorption is reduced with a mean delay in Tmax of 60 minutes and a mean reduction in Cmax of 29 % however, the extent of absorption was not significantly affected (AUC decreased by 11 %). Distribution The mean steady state volume of distribution (Vss) for sildenafil is 105 l, indicating distribution into the tissues. After oral doses of 20 mg three times a day, the mean maximum total plasma concentration of sildenafil at steady state is approximately 113 ng/ml. Sildenafil and its major circulating N-desmethyl metabolite are approximately 96 % bound to plasma proteins. Protein binding is independent of total drug concentrations. Biotransformation Sildenafil is cleared predominantly by the CYP3A4 (major route) and CYP2C9 (minor route) hepatic microsomal isoenzymes. The major circulating metabolite results from N-demethylation of sildenafil. This metabolite has a phosphodiesterase selectivity profile similar to sildenafil and an in vitro potency for PDE5 approximately 50 % that of the parent drug. The N-desmethyl metabolite is further metabolised, with a terminal half-life of approximately 4 h. In patients with pulmonary arterial hypertension, plasma concentrations of N-desmethyl metabolite are approximately 72 % those of sildenafil after 20 mg three times a day dosing (translating into a 36 % contribution to sildenafil's pharmacological effects). The subsequent effect on efficacy is unknown. Elimination The total body clearance of sildenafil is 41 l/h with a resultant terminal phase half-life of 3-5 h. After either oral or intravenous administration, sildenafil is excreted as metabolites predominantly in the faeces (approximately 80 % of administered oral dose) and to a lesser extent in the urine (approximately 13 % of administered oral dose). Pharmacokinetics in special patient groups Elderly Healthy elderly volunteers (65 years or over) had a reduced clearance of sildenafil, resulting in approximately 90 % higher plasma concentrations of sildenafil and the active N-desmethyl metabolite compared to those seen in healthy younger volunteers (18-45 years). Due to age-differences in plasma protein binding, the corresponding increase in free sildenafil plasma concentration was approximately 40 %. Renal insufficiency In volunteers with mild to moderate renal impairment (creatinine clearance = 30-80 ml/min), the pharmacokinetics of sildenafil were not altered after receiving a 50 mg single oral dose. In volunteers with severe renal impairment (creatinine clearance < 30 ml/min), sildenafil clearance was reduced, resulting in mean increases in AUC and Cmax of 100 % and 88 % respectively compared to age-matched volunteers with no renal impairment. In addition, N- desmethyl metabolite AUC and Cmax values were significantly increased by 200 % and 79 % respectively in subjects with severe renal impairment compared to subjects with normal renal function. Hepatic insufficiency In volunteers with mild to moderate hepatic cirrhosis (Child-Pugh class A and B) sildenafil clearance was reduced, resulting in increases in AUC (85 %) and Cmax (47 %) compared to age-matched volunteers with no hepatic impairment. In addition, N-desmethyl metabolite AUC and Cmax values were significantly increased by 154 % and 87 %, respectively in cirrhotic subjects compared to subjects with normal hepatic function. The pharmacokinetics of sildenafil in patients with severely impaired hepatic function have not been studied. Population pharmacokinetics In patients with pulmonary arterial hypertension, the average steady state concentrations were 20 - 50 % higher over the investigated dose range of 20–80 mg three times a day compared to healthy volunteers. There was a doubling of the Cmin compared to healthy volunteers. Both findings suggest a lower clearance and/or a higher oral bioavailability of sildenafil in patients with pulmonary arterial hypertension compared to healthy volunteers.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול בחולה המוגדר ב-NYHA (New York Heart Association) כ-Class III ומעלה הסובל מיתר לחץ דם ריאתי עורקי. ב. התחלת הטיפול בתרופה האמורה תהיה על פי הוראתו של מנהל מחלקה בבית חולים שהוא מומחה למחלות ריאה או מומחה בקרדיולוגיה או מומחה בטיפול נמרץ כללי או מומחה בכירורגית כלי דם או מומחה בקרדיולוגית ילדים או מומחה במחלות ריאה ילדים או מומחה בטיפול נמרץ ילדים או מומחה בראומטולוגיה. ג. משך הטיפול בתרופה האמורה ייעשה על פי מרשם של מומחה למחלות ריאה או מומחה בקרדיולוגיה או מומחה בטיפול נמרץ כללי או מומחה בכירורגית כלי דם או מומחה בקרדיולוגית ילדים או מומחה במחלות ריאה ילדים או מומחה בטיפול נמרץ ילדים או מומחה בראומטולוגיה. ד. ניתן להתחיל טיפול בתרופה האמורה במקרה בו התנגודת הריאתית המחושבת תישאר גבוהה אחרי טסט פרמקולוגי וזאת כאשר החולה סובל מ-NYHA Class III ומעלה ובעל מרחק הליכה ל-6 דקות הנמוך מ-400 מטרים ב-2 בדיקות עוקבות.ה. יש להימנע משילובי תרופות אלא לטפל בכל פעם בתרופה בודדת ורק עם כישלון בטיפול בה, לעבור לטיפול בתרופה אחרת, למעט המצבים הבאים: 1. בכישלון של טיפול ב-Sildenafil ניתן להוסיף במקרים נבחרים Iloprost באינהלציה או Selexipag או Bosentan או Ambrisentan או Macitentan.2. בכישלון של טיפול ב-Bosentan או Ambrisentan או Macitentan ניתן להוסיף במקרים נבחרים Iloprost באינהלציה או Selexipag או Sildenafil3. בכישלון של טיפול משולב ב- Bosentan או Ambrisentan או Macitentan עם Sildenafil או Tadalafil ניתן להוסיף במקרים נבחרים Selexipag. 4. השילוב של Epoprostenol או Treprostinil עם Ambrisentan או Macitentan או Bosentan או Sildenafil יעשה רק לאחר כישלון של אחד מהפרוסטציקלינים האמורים כטיפול בודד.5. השילוב של תרופה ממשפחת ה-Endothelin receptor antagonists (Ambrisentan או Macitentan או Bosentan) עם תרופה ממשפחת מעכבי PDE5 (Sildenafil או Tadalafil) יתאפשר כטיפול ראשוני (Upfront) עבור חולי יתר לחץ דם ריאתי עורקי, Group 1, שטרם קיבלו טיפול למחלתם.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לטיפול באין אונות | ||||
| לטיפול ביתר לחץ דם ריאתי |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
20/09/2006
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
