Quest for the right Drug
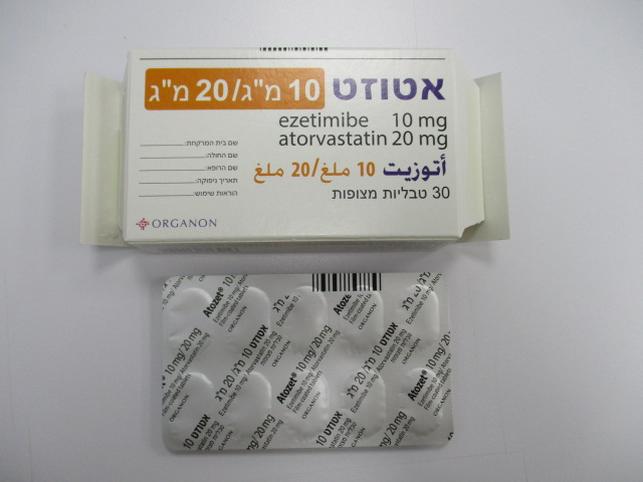
אטוזט 10 מ"ג/20 מ"ג ATOZET10 MG/20 MG (ATORVASTATIN AS CALCIUM TRIHYDRATE, EZETIMIBE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Interactions : אינטראקציות
4.5 Interaction with other medicinal products and other forms of interaction Multiple mechanisms may contribute to potential interactions with HMG CoA reductase inhibitors. Drugs or herbal products that inhibit certain enzymes (e.g. CYP3A4) and/or transporter (e.g. OATP1B) pathways may increase atorvastatin plasma concentrations and may lead to an increased risk of myopathy/rhabdomyolysis. Consult the prescribing information of all concomitantly used drugs to obtain further information about their potential interactions with atorvastatin and/or the potential for enzyme or transporter alterations and possible adjustments to dose and regimens. Pharmacodynamic interactions Atorvastatin is metabolised by cytochrome P450 3A4 (CYP3A4) and is a substrate of the hepatic transporters, organic anion-transporting polypeptide 1B1 (OATP1B1) and 1B3 (OATP1B3) transporter. Metabolites of atorvastatin are substrates of OATP1B1. Atorvastatin is also identified as a substrate of the multi-drug resistance protein 1 (MDR1) and breast cancer resistance protein (BCRP), which may limit the intestinal absorption and biliary clearance of atorvastatin (see section 5.2). Concomitant administration of medicinal products that are inhibitors of CYP3A4 or transport proteins may lead to increased plasma concentrations of atorvastatin and an increased risk of myopathy. The risk might also be increased at concomitant administration of ATOZET with other medicinal products that have a potential to induce myopathy, such as fibric acid derivatives and ezetimibe (see section 4.4). Pharmacokinetic interactions ATOZET No clinically significant pharmacokinetic interaction was seen when ezetimibe was co-administered with atorvastatin. Effects of other medicinal products on ATOZET Ezetimibe Antacids: Concomitant antacid administration decreased the rate of absorption of ezetimibe but had no effect on the bioavailability of ezetimibe. This decreased rate of absorption is not considered clinically significant. Cholestyramine: Concomitant cholestyramine administration decreased the mean area under the curve (AUC) of total ezetimibe (ezetimibe + ezetimibe-glucuronide) approximately 55%. The incremental low-density lipoprotein cholesterol (LDL-C) reduction due to adding ATOZET to cholestyramine may be lessened by this interaction (see section 4.2). Ciclosporin: In a study of eight post-renal transplant patients with creatinine clearance of > 50 mL/min on a stable dose of ciclosporin, a single 10-mg dose of ezetimibe resulted in a 3.4-fold (range 2.3 to 7.9 fold) increase in the mean AUC for total ezetimibe compared to a healthy control population, receiving ezetimibe alone, from another study (n = 17). In a different study, a renal transplant patient with severe renal insufficiency who was receiving ciclosporin and multiple other medicinal products demonstrated a 12-fold greater exposure to total ezetimibe compared to concurrent controls receiving ezetimibe alone. In a two-period crossover study in twelve healthy subjects, daily administration of 20 mg ezetimibe for 8 days with a single 100-mg dose of ciclosporin on Day 7 resulted in a mean 15% increase in ciclosporin AUC (range 10% decrease to 51% increase) compared to a single 100-mg dose of ciclosporin alone. A controlled study on the effect of co-administered ezetimibe on ciclosporin exposure in renal transplant patients has not been conducted. Caution should be exercised when initiating ATOZET in the setting of ciclosporin. Ciclosporin concentrations should be monitored in patients receiving ATOZET and ciclosporin (see section 4.4). Fibrates: Concomitant fenofibrate or gemfibrozil administration increased total ezetimibe concentrations approximately 1.5 and 1.7 fold, respectively. Although these increases are not considered clinically significant, co-administration of ATOZET with fibrates is not recommended (see section 4.4). Atorvastatin CYP3A4 inhibitors: Potent CYP3A4 inhibitors have been shown to lead to markedly increased concentrations of atorvastatin (see Table 1 and specific information below). Co-administration of potent CYP3A4 inhibitors (e.g., ciclosporin, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole, some antivirals used in the treatment of HCV (e.g. elbasvir/grazoprevir) and HIV protease inhibitors including ritonavir, lopinavir, atazanavir, indinavir, darunavir, etc.) should be avoided if possible. In cases where co-administration of these medicinal products with ATOZET cannot be avoided, lower starting and maximum doses of ATOZET should be considered and appropriate clinical monitoring of the patient is recommended (see Table 1). Moderate CYP3A4 inhibitors (e.g. erythromycin, diltiazem, verapamil and fluconazole) may increase plasma concentrations of atorvastatin (see Table 1). An increased risk of myopathy has been observed with the use of erythromycin in combination with statins. Interaction studies evaluating the effects of amiodarone or verapamil on atorvastatin have not been conducted. Both amiodarone and verapamil are known to inhibit CYP3A4 activity and co-administration with ATOZET may result in increased exposure to atorvastatin. Therefore, a lower maximum dose of ATOZET should be considered and appropriate clinical monitoring of the patient is recommended when concomitantly used with moderate CYP3A4 inhibitors. Appropriate clinical monitoring is recommended after initiation or following dose adjustments of the inhibitor. Inhibitors of Breast Cancer Resistant Protein (BCRP): Concomitant administration of products that are inhibitors of BCRP (e.g. elbasvir and grazoprevir) may lead to increased plasma concentrations of atorvastatin and an increased risk of myopathy; therefore, a dose adjustment of atorvastatin should be considered depending on the prescribed dose. Co-administration of elbasvir and grazoprevir with atorvastatin increases plasma concentrations of atorvastatin 1.9-fold (see Table 1); therefore, the dose of ATOZET should not exceed 10/20 mg daily in patients receiving concomitant medications with products containing elbasvir or grazoprevir (see sections 4.2 and 4.4). Inducers of cytochrome P450 3A4: Concomitant administration of atorvastatin with inducers of cytochrome P450 3A4 (e.g. efavirenz, rifampicin, St. John's wort) can lead to variable reductions in plasma concentrations of atorvastatin. Due to the dual interaction mechanism of rifampicin, (cytochrome P450 3A4 induction and inhibition of hepatocyte uptake transporter OATP1B1), simultaneous co-administration of ATOZET with rifampicin is recommended, as delayed administration of atorvastatin after administration of rifampicin has been associated with a significant reduction in atorvastatin plasma concentrations. The effect of rifampicin on atorvastatin concentrations in hepatocytes is, however, unknown and if concomitant administration cannot be avoided, patients should be carefully monitored for efficacy. Transport inhibitors: Inhibitors of transport proteins (e.g. ciclosporin) can increase the systemic exposure of atorvastatin (see Table 1). The effect of inhibition of hepatic uptake transporters on atorvastatin concentrations in hepatocytes is unknown. If concomitant administration cannot be avoided, a dose reduction of ATOZET and clinical monitoring for efficacy is recommended (see Table 1). Gemfibrozil / fibric acid derivatives: The use of fibrates alone is occasionally associated with muscle- related events, including rhabdomyolysis. The risk of these events may be increased with the concomitant use of fibric acid derivatives and atorvastatin. Ezetimibe: The use of ezetimibe alone is associated with muscle-related events, including rhabdomyolysis. The risk of these events may therefore be increased with concomitant use of ezetimibe and atorvastatin. Appropriate clinical monitoring of these patients is recommended. Colestipol: Plasma concentrations of atorvastatin and its active metabolites were lower (by approx. 25%) when colestipol was co-administered with atorvastatin. However, lipid effects were greater when atorvastatin and colestipol were co-administered than when either medicinal product was given alone. Fusidic acid: The risk of myopathy including rhabdomyolysis may be increased by the concomitant administration of systemic fusidic acid with statins. The mechanism of this interaction (whether it is pharmacodynamic or pharmacokinetic, or both) is yet unknown. There have been reports of rhabdomyolysis (including some fatalities) in patients receiving this combination. If treatment with systemic fusidic acid is necessary, atorvastatin treatment should be discontinued throughout the duration of the fusidic acid treatment. Also see section 4.4. Colchicine: Although interaction studies with atorvastatin and colchicine have not been conducted, cases of myopathy have been reported with atorvastatin co-administered with colchicine, and caution should be exercised when prescribing atorvastatin with colchicine. Daptomycin: The risk of myopathy and/or rhabdomyolysis may be increased by concomitant administration of HMG-CoA reductase inhibitors and daptomycin. Consideration should be given to suspending ATOZET temporarily in patients taking daptomycin unless the benefits of concomitant administration outweigh the risk (see section 4.4). Boceprevir: Exposure to atorvastatin was increased when administered with boceprevir. When co- administration with ATOZET is required, starting with the lowest possible dose of ATOZET should be considered with titration up to desired clinical effect while monitoring for safety, without exceeding a daily dose of 10/20 mg. For patients currently taking ATOZET, the dose of ATOZET should not exceed a daily dose of 10/20 mg during co-administration with boceprevir. Effects of ATOZET on the pharmacokinetics of other medicinal products Ezetimibe In preclinical studies, it has been shown that ezetimibe does not induce cytochrome P450 drug metabolising enzymes. No clinically significant pharmacokinetic interactions have been observed between ezetimibe and drugs known to be metabolised by cytochromes P450 1A2, 2D6, 2C8, 2C9, and 3A4, or N-acetyltransferase. Anticoagulants: Concomitant administration of ezetimibe (10 mg once daily) had no significant effect on bioavailability of warfarin and prothrombin time in a study of twelve healthy adult males. However, there have been post-marketing reports of increased International Normalised Ratio (INR) in patients who had ezetimibe added to warfarin or fluindione. If ATOZET is added to warfarin, another coumarin anticoagulant, or fluindione, INR should be appropriately monitored (see section 4.4). Atorvastatin Digoxin: When multiple doses of digoxin and 10 mg atorvastatin were co-administered, steady-state digoxin concentrations increased slightly. Patients taking digoxin should be monitored appropriately. Oral contraceptives: Co-administration of atorvastatin with an oral contraceptive produced increases in plasma concentrations of norethisterone and ethinyl estradiol. Warfarin: In a clinical study in patients receiving chronic warfarin therapy, co-administration of atorvastatin 80 mg daily with warfarin caused a small decrease of about 1.7 seconds in prothrombin time during the first 4 days of dosing, which returned to normal within 15 days of atorvastatin treatment. Although only very rare cases of clinically significant anticoagulant interactions have been reported, prothrombin time should be determined before starting ATOZET in patients taking coumarin anticoagulants and frequently enough during early therapy to ensure that no significant alteration of prothrombin time occurs. Once a stable prothrombin time has been documented, prothrombin times can be monitored at the intervals usually recommended for patients on coumarin anticoagulants. If the dose of ATOZET is changed or discontinued, the same procedure should be repeated. Atorvastatin therapy has not been associated with bleeding or with changes in prothrombin time in patients not taking anticoagulants. Table 1 Effect of Co-administered Medicinal Products on the Pharmacokinetics of Atorvastatin Co-administered Medicinal Product Atorvastatin ATOZET and Dosing Regimen Dose (mg) Change in AUC& Clinical Recommendation# Tipranavir 500 mg BID/ Ritonavir 40 mg on Day 1, ↑ 9.4-fold In cases where co- 200 mg BID, 8 days (Days 14 to 21) 10 mg on Day 20 administration with ATOZET is necessary, do not exceed 10/10 mg ATOZET daily. Clinical monitoring of these patients is Ciclosporin 5.2 mg/kg/day, stable 10 mg OD for ↑ 8.7-fold recommended. dose 28 days Lopinavir 400 mg BID/ Ritonavir 20 mg OD for ↑ 5.9-fold In cases where co- 100 mg BID, 14 days 4 days administration with ATOZET is necessary, lower maintenance doses of ATOZET are recommended. At ATOZET doses exceeding 10/20 mg, clinical monitoring of these patients is Clarithromycin 500 mg BID, 9 days 80 mg OD for ↑ 4.4-fold recommended. 8 days Saquinavir 400 mg BID/ Ritonavir 40 mg OD for ↑ 3.9-fold In cases where co- 300 mg BID from Days 5-7, increased 4 days administration with to 400 mg BID on Day 8), Days 5-18, ATOZET is necessary, 30 min after atorvastatin dosing lower maintenance doses of ATOZET are recommended. At ATOZET doses exceeding 10/40 mg, clinical monitoring of these patients is Darunavir 300 mg BID/ 10 mg OD for ↑ 3.3-fold recommended. Ritonavir 100 mg BID, 9 days 4 days Itraconazole 200 mg OD, 4 days 40 mg SD ↑ 3.3-fold Fosamprenavir 700 mg BID/ 10 mg OD for ↑ 2.5-fold Ritonavir 100 mg BID, 14 days 4 days Fosamprenavir 1400 mg BID, 14 days 10 mg OD for ↑ 2.3-fold 4 days Nelfinavir 1250 mg BID, 14 days 10 mg OD for ↑ 1.7-fold^ No specific 28 days recommendation. Grapefruit juice, 240 mL OD* 40 mg SD ↑ 37% Concomitant intake of large quantities of grapefruit juice and ATOZET is not recommended. Diltiazem 240 mg OD, 28 days 40 mg SD ↑ 51% After initiation or following dose adjustments of diltiazem, appropriate clinical monitoring of these patients is recommended. Erythromycin 500 mg QID, 7 days 10 mg SD ↑ 33%^ Lower maximum dose and clinical monitoring of these patients is recommended. Amlodipine 10 mg, single dose 80 mg SD ↑ 18% No specific recommendation. Cimetidine 300 mg QID, 2 weeks 10 mg OD for ↓ less than 1%^ No specific 4 weeks recommendation. Antacid suspension of magnesium and 10 mg OD for ↓ 35%^ No specific aluminium hydroxides, 30 mL QID, 4 weeks recommendation. 2 weeks Efavirenz 600 mg OD, 14 days 10 mg for 3 days ↓ 41% No specific recommendation. Rifampicin 600 mg OD, 7 days (co- 40 mg SD ↑ 30% If co-administration administered) cannot be avoided, simultaneous co- administration of ATOZET with Rifampicin 600 mg OD, 5 days (doses 40 mg SD ↓ 80% rifampicin is separated) recommended, with clinical monitoring. Gemfibrozil 600 mg BID, 7 days 40 mg SD ↑ 35% Not recommended. Fenofibrate 160 mg OD, 7 days 40 mg SD ↑ 3% Not recommended. Boceprevir 800 mg TID, 7 days 40 mg SD ↑ 2.3-fold Lower starting dose and clinical monitoring of these patients is recommended. The dose of ATOZET should not exceed a daily dose of 10/20 mg during co- administration with boceprevir. Elbasvir 50 mg OD/Grazoprevir 10 mg SD ↑1.94-fold The dose of ATOZET 200 mg OD, 13 days should not exceed a daily dose of 10/20 mg during co- administration with products containing elbasvir or grazoprevir. Glecaprevir 400 mg OD/Pibrentasvir 10 mg OD for 7 ↑ 8.3-fold Co-administration with 120 mg OD, 7 days days products containing glecaprevir or pibrentasvir is contraindicated (see section 4.3). & Data given as x-fold change represent a simple ratio between co-administration and atorvastatin alone (i.e., 1-fold = no change). Data given as % change represent % difference relative to atorvastatin alone (i.e., 0% = no change). # See sections 4.4 and 4.5 for clinical significance. * Contains one or more components that inhibit CYP3A4 and can increase plasma concentrations of medicinal products metabolised by CYP3A4. Intake of one 240 mL glass of grapefruit juice also resulted in a decreased AUC of 20.4% for the active orthohydroxy metabolite. Large quantities of grapefruit juice (over 1.2 l daily for 5 days) increased AUC of atorvastatin 2.5 fold and AUC of active (atorvastatin and metabolites). ^ Total atorvastatin equivalent activity Increase is indicated as “↑”, decrease as “↓” OD = once daily; SD = single dose; BID = twice daily; TID = three times daily; QID = four times daily Table 2 Effect of Atorvastatin on the Pharmacokinetics of Co-administered Medicinal Products Atorvastatin and Dosing Co-administered Medicinal Product ATOZET Regimen Medicinal Product/Dose Change in AUC& Clinical (mg) Recommendation 80 mg OD for 10 days Digoxin 0.25 mg OD, ↑ 15% Patients taking digoxin 20 days should be monitored appropriately. 40 mg OD for 22 days Oral contraceptive OD, No specific 2 months recommendation. -norethisterone 1 mg ↑ 28% -ethinyl estradiol 35 μg ↑ 19% 80 mg OD for 15 days * Phenazone, 600 mg ↑ 3% No specific SD recommendation 10 mg OD for 4 days Fosamprenavir 1400 mg ↓ 27% No specific BID, 14 days recommendation & Data given as % change represent % difference relative to atorvastatin alone (i.e., 0% = no change) * Co-administration of multiple doses of atorvastatin and phenazone showed little or no detectable effect in the clearance of phenazone. Increase is indicated as “↑”, decrease as “↓” OD = once daily; SD = single dose; BID = twice daily

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
08.03.18 - עלון לצרכן 11.01.21 - עלון לצרכן אנגלית 11.01.21 - עלון לצרכן עברית 08.03.18 - עלון לצרכן ערבית 24.01.21 - עלון לצרכן ערבית 15.11.22 - עלון לצרכן אנגלית 15.11.22 - עלון לצרכן עברית 15.11.22 - עלון לצרכן ערבית 26.04.20 - החמרה לעלון 11.01.21 - החמרה לעלון 15.11.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אטוזט 10 מ"ג/20 מ"ג