Quest for the right Drug
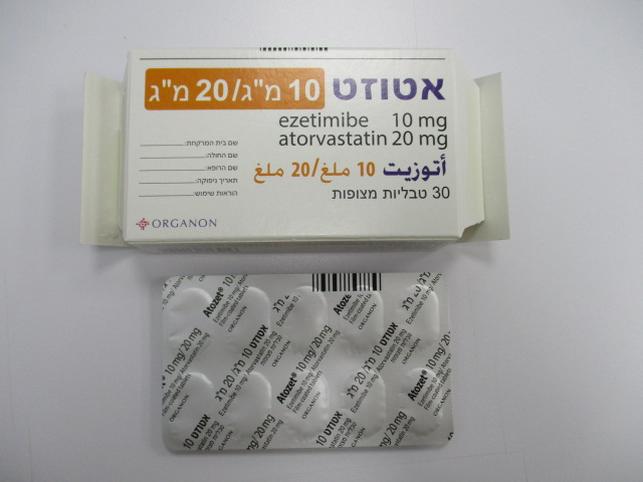
אטוזט 10 מ"ג/20 מ"ג ATOZET10 MG/20 MG (ATORVASTATIN AS CALCIUM TRIHYDRATE, EZETIMIBE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Myopathy/Rhabdomyolysis In post-marketing experience with ezetimibe, cases of myopathy and rhabdomyolysis have been reported. Most patients who developed rhabdomyolysis were taking a statin concomitantly with ezetimibe. However, rhabdomyolysis has been reported very rarely with ezetimibe monotherapy and very rarely with the addition of ezetimibe to other agents known to be associated with increased risk of rhabdomyolysis. ATOZET contains atorvastatin. Atorvastatin, like other HMG-CoA reductase inhibitors, may in rare occasions affect the skeletal muscle and cause myalgia, myositis, and myopathy that may progress to rhabdomyolysis, a potentially life-threatening condition characterised by markedly elevated creatine phosphokinase (CPK) levels (> 10 times ULN), myoglobinaemia and myoglobinuria, which may lead to renal failure. Before the treatment ATOZET should be prescribed with caution in patients with pre-disposing factors for rhabdomyolysis. A CPK level should be measured before starting treatment in the following situations: • renal impairment, • hypothyroidism, • personal or familial history of hereditary muscular disorders, • previous history of muscular toxicity with a statin or fibrate, • previous history of liver disease and/or where substantial quantities of alcohol are consumed, • in elderly (age > 70 years), the necessity of such measurement should be considered, according to the presence of other predisposing factors for rhabdomyolysis, • situations where an increase in plasma levels may occur, such as interactions (see section 4.5) and special populations including genetic subpopulations (see section 5.2). In such situations, the risk of treatment should be considered in relation to possible benefit, and clinical monitoring is recommended. If CPK levels are significantly elevated (> 5 times ULN) at baseline, treatment should not be started. Creatine phosphokinase measurement Creatine phosphokinase (CPK) should not be measured following strenuous exercise or in the presence of any plausible alternative cause of CPK increase as this makes value interpretation difficult. If CPK levels are significantly elevated at baseline (> 5 times ULN), levels should be remeasured within 5 to 7 days later to confirm the results. Whilst on treatment • Patients must be asked to promptly report muscle pain, cramps, or weakness especially if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing ATOZET. • If such symptoms occur whilst a patient is receiving treatment with ATOZET, their CPK levels should be measured. If these levels are found to be significantly elevated (> 5 times ULN), treatment should be stopped. • If muscular symptoms are severe and cause daily discomfort, even if the CPK levels are elevated to ≤ 5 times ULN, treatment discontinuation should be considered. • If symptoms resolve and CPK levels return to normal, then re-introduction of ATOZET or introduction of another statin-containing product may be considered at the lowest dose and with close monitoring. • ATOZET must be discontinued if clinically significant elevation of CPK levels (> 10 times ULN) occur, or if rhabdomyolysis is diagnosed or suspected. • There have been very rare reports of an immune-mediated necrotising myopathy (IMNM) during or after treatment with some statins. IMNM is clinically characterised by persistent proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment. Due to the atorvastatin component of ATOZET, the risk of rhabdomyolysis is increased when ATOZET is administered concomitantly with certain medicinal products that may increase the plasma concentration of atorvastatin such as potent inhibitors of CYP3A4 or transport proteins (e.g. ciclosporin, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole, and HIV protease inhibitors including ritonavir, lopinavir, atazanavir, indinavir, darunavir, tipranavir/ritonavir, etc). The risk of myopathy may also be increased with the concomitant use of gemfibrozil and other fibric acid derivatives, antivirals for the treatment of hepatitis C (HCV) (boceprevir, telaprevir, elbasvir/grazoprevir), erythromycin, or niacin. If possible, alternative (non-interacting) therapies should be considered instead of these medicinal products (see section 4.8). In cases where co-administration of these medicinal products with ATOZET is necessary, the benefit and the risk of concurrent treatment should be carefully considered. When patients are receiving medicinal products that increase the plasma concentration of atorvastatin, a lower maximum dose of ATOZET is recommended. In addition, in the case of potent CYP3A4 inhibitors, a lower starting dose of ATOZET should be considered and appropriate clinical monitoring of these patients is recommended (see section 4.5). Atorvastatin must not be co-administered with systemic formulations of fusidic acid or within 7 days of stopping fusidic acid treatment. In patients where the use of systemic fusidic acid is considered essential, statin treatment should be discontinued throughout the duration of fusidic acid treatment. There have been reports of rhabdomyolysis (including some fatalities) in patients receiving fusidic acid and statins in combination (see section 4.5). The patient should be advised to seek medical advice immediately if they experience any symptoms of muscle weakness, pain or tenderness. Statin therapy may be re-introduced seven days after the last dose of fusidic acid. In exceptional circumstances, where prolonged systemic fusidic acid is needed, e.g. for the treatment of severe infections, the need for co-administration of ATOZET and fusidic acid should only be considered on a case by case basis and under close medical supervision. Daptomycin Cases of myopathy and/or rhabdomyolysis have been reported with HMG-CoA reductase inhibitors (e.g. atorvastatin and ezetimibe/atorvastatin) co-administered with daptomycin. Caution should be used when prescribing HMG-CoA reductase inhibitors with daptomycin, as either agent can cause myopathy and/or rhabdomyolysis when given alone. Consideration should be given to temporarily suspend ATOZET in patients taking daptomycin unless the benefits of concomitant administration outweigh the risk. Consult the prescribing information of daptomycin to obtain further information about this potential interaction with HMG-CoA reductase inhibitors (e.g. atorvastatin and ezetimibe/atorvastatin) and for further guidance related to monitoring (see section 4.5). Liver Enzymes In controlled co-administration trials in patients receiving ezetimibe and atorvastatin, consecutive transaminase elevations (≥ 3 times the upper limit of normal [ULN]) have been observed (see section 4.8). Liver function tests should be performed before the initiation of treatment and periodically thereafter. Patients who develop any signs or symptoms suggestive of liver injury should have liver function tests performed. Patients who develop increased transaminase levels should be monitored until the abnormality(ies) resolve. Should an increase in transaminases of greater than 3 times the ULN persist, reduction of dose or withdrawal of ATOZET is recommended. ATOZET should be used with caution in patients who consume substantial quantities of alcohol and/or have a history of liver disease. Hepatic Insufficiency Due to the unknown effects of the increased exposure to ezetimibe in patients with moderate or severe hepatic insufficiency, ATOZET is not recommended (see section 5.2). Fibrates The safety and efficacy of ezetimibe administered with fibrates have not been established; therefore, co-administration of ATOZET and fibrates is not recommended (see section 4.5). Ciclosporin Caution should be exercised when initiating ATOZET in the setting of ciclosporin. Ciclosporin concentrations should be monitored in patients receiving ATOZET and ciclosporin (see section 4.5). Anticoagulants If ATOZET is added to warfarin, another coumarin anticoagulant, or fluindione, the International Normalised Ratio (INR) should be appropriately monitored (see section 4.5). Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) In a post-hoc analysis of stroke subtypes in patients without coronary heart disease (CHD) who had a recent stroke or transient ischaemic attack (TIA) there was a higher incidence of haemorrhagic stroke in patients initiated on atorvastatin 80 mg compared to placebo. The increased risk was particularly noted in patients with prior haemorrhagic stroke or lacunar infarct at study entry. For patients with prior haemorrhagic stroke or lacunar infarct, the balance of risks and benefits of atorvastatin 80 mg is uncertain, and the potential risk of haemorrhagic stroke should be carefully considered before initiating treatment (see section 5.1). Interstitial lung disease Exceptional cases of interstitial lung disease have been reported with some statins, especially with long term therapy (see section 4.8). Presenting features can include dyspnoea, non-productive cough and deterioration in general health (fatigue, weight loss and fever). If it is suspected a patient has developed interstitial lung disease, statin therapy should be discontinued. Diabetes mellitus Some evidence suggests that statins as a class raise blood glucose and in some patients, at high risk of future diabetes, may produce a level of hyperglycaemia where formal diabetes care is appropriate. This risk, however, is outweighed by the reduction in vascular risk with statins and therefore should not be a reason for stopping statin treatment. Patients at risk (fasting glucose 5.6 to 6.9 mmol/L, BMI > 30kg/m2, raised triglycerides, hypertension) should be monitored both clinically and biochemically according to national guidelines. Excipients ATOZET contains lactose. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency, or glucose-galactose malabsorption should not take this medicine. ATOZET contains less than 1 mmol (23 mg) sodium per tablet and is considered to be essentially sodium-free.
Effects on Driving
4.7 Effects on ability to drive and use machines ATOZET has negligible influence on the ability to drive and use machines. However, when driving vehicles or operating machines, it should be taken into account that dizziness has been reported.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
08.03.18 - עלון לצרכן 11.01.21 - עלון לצרכן אנגלית 11.01.21 - עלון לצרכן עברית 08.03.18 - עלון לצרכן ערבית 24.01.21 - עלון לצרכן ערבית 15.11.22 - עלון לצרכן אנגלית 15.11.22 - עלון לצרכן עברית 15.11.22 - עלון לצרכן ערבית 26.04.20 - החמרה לעלון 11.01.21 - החמרה לעלון 15.11.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אטוזט 10 מ"ג/20 מ"ג