Quest for the right Drug
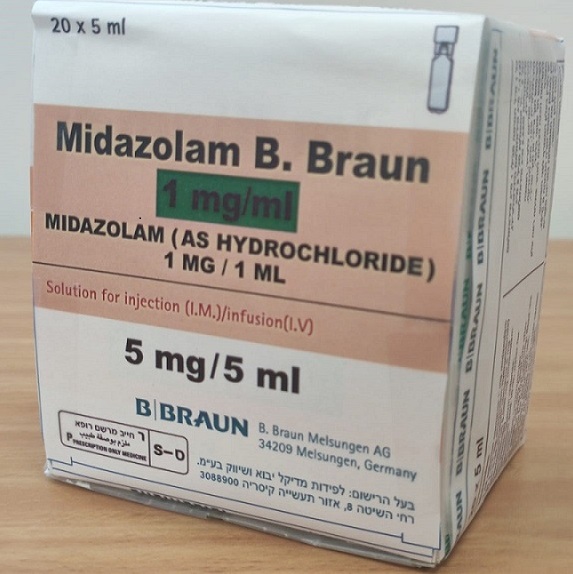
מידאזולאם ב.בראון 1 מ"ג/מ"ל MIDAZOLAM B.BRAUN 1 MG/ML (MIDAZOLAM AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-ורידי : I.M, I.V
צורת מינון:
תמיסה להזרקהאינפוזיה : SOLUTION FOR INJECTION / INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Hypnotics and sedatives (benzodiazepine derivatives), ATC code: N05CD08. Mechanism of action The central actions of benzodiazepines are mediated through an enhancement of the GABAergic neurotransmission at inhibitory synapses. In the presence of benzodiazepines the affinity of the GABA receptor for the neurotransmitter is enhanced through positive allosteric modulation resulting in an increased action of released GABA on the postsynaptic transmembrane chloride ion flux. Chemically midazolam is a derivative of the imidazobenzodiazepine group. The basic nitrogen in position 2 of the imidazobenzodiazepine ring system enables the active ingredient of midazolam to form water- soluble salts with acids, producing a stable and well tolerated injection solution. At physiological pH the diazepine ring closes and the free base is formed resulting in a lipophilic substance with rapid onset of action. Rapid metabolic transformation and redistribution are key reasons for short duration of effects. Pharmacodynamic effects Midazolam has hypnotic and sedative effects characterised by a rapid onset and short duration. It also exerts anxiolytic, anticonvulsant and muscle-relaxant effects. Midazolam impairs psychomotor function after single and/or multiple doses but causes minimal haemodynamic changes. After i.m. or i.v. administration anterograde amnesia of short duration occurs (the patient does not remember events that occurred during the maximal activity of the compound).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Absorption after i.m. injection Absorption of midazolam from the muscle tissue is rapid and complete. Maximum plasma concentrations are reached within 30 minutes. The absolute bioavailability after i.m. injection is over 90%. Distribution When midazolam is injected i.v., the plasma concentration-time curve shows one or two distinct disposition phases. The volume of distribution at steady state is 0.7-1.2 l/kg. 96-98% of midazolam is bound to plasma proteins. The major binding protein is albumin. There is a slow and insignificant passage of midazolam into the cerebrospinal fluid. In humans, midazolam has been shown to cross the placenta slowly and to enter foetal circulation. Small quantities of midazolam are found in human milk. Midazolam is not a substrate for any of the drug transporters tested so far (cellular efflux transporter: P- glycoprotein; cellular uptake transporters: OAT1, OAT2, OAT3, OCT1, OCT2, OATP1A2, OATP1B1, OATP1B3.1, OATP1B3.2, OATP2B1 and rOatp1b2, which is found in rats only). Biotransformation Midazolam is almost entirely eliminated by biotransformation. The fraction of the dose extracted by the liver has been estimated to be 30-60%. Midazolam is hydroxylated by the cytochrome P450 CYP3A4 and CYP3A5 isozymes and the major urinary and plasma metabolite is 1’-hydroxymidazolam (also known as alpha- hydroxymidazolam). Plasma concentrations of 1’-hydroxymidazolam are 12% of those of the parent compound. 1’-hydroxymidazolam is pharmacologically active, but contributes only minimally (about 10%) to the effects of intravenous midazolam. Elimination In young healthy volunteers, the elimination half-life of midazolam ranges from 1.5 to 2.5 hours. The elimination half-life of the metabolite is shorter than 1 hour; therefore after midazolam administration the concentration of the parent compound and the main metabolite decline in parallel. Plasma clearance of midazolam is in the range of 300–500 ml/min. Midazolam’s metabolites are excreted mainly by the renal route (60-80% of the injected dose) and recovered as glucuroconjugated 1’- hydroxymidazolam. Less than 1% of the dose is recovered in urine as unchanged drug. When midazolam is given by i.v. infusion, its elimination kinetics do not differ from those following bolus injection. Repeated administrations of midazolam do not induce drug metabolising enzymes. Pharmacokinetics in special populations Elderly In adults over 60 years of age, the elimination half-life may be prolonged up to four times. Children The elimination half-life after i.v. administration is shorter in children 3-10 years old (1-1.5 hours) as compared with that in adults. The difference is consistent with an increased metabolic clearance in children. Neonates In neonates the elimination half-life is on average 6-12 hours, probably due to liver immaturity and the clearance is reduced. Neonates with asphyxia-related hepatic and renal impairment are at risk of generating unexpectedly high serum midazolam concentration due to a significantly decreased and variable clearance (see section 4.4). Obese The mean half-life is greater in obese than in non-obese patients (5.9 vs 2.3 hours). This is due to an increase of approximately 50% in the volume of distribution corrected for total body weight. The clearance is not significantly different in obese and non-obese patients. Patients with hepatic impairment The clearance in cirrhotic patients may be reduced and the elimination may be longer when compared to those in healthy volunteers (see section 4.4). Patients with renal impairment The pharmacokinetics of unbound midazolam are not altered in patients with severe renal impairment. The pharmacologically mildly active major midazolam metabolite, 1’-hydroxymidazolam glucuronide, which is excreted through the kidney, accumulates in patients with severe renal impairment. This accumulation may produce a prolonged sedation. Midazolam should therefore be administered carefully and titrated to the desired effect (see section 4.4). Critically ill patients The elimination half-life of midazolam is prolonged up to six times in the critically ill. Patients with cardiac insufficiency The elimination half-life is longer in patients with congestive heart failure compared with that in healthy subjects (see section 4.4).

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
