Quest for the right Drug
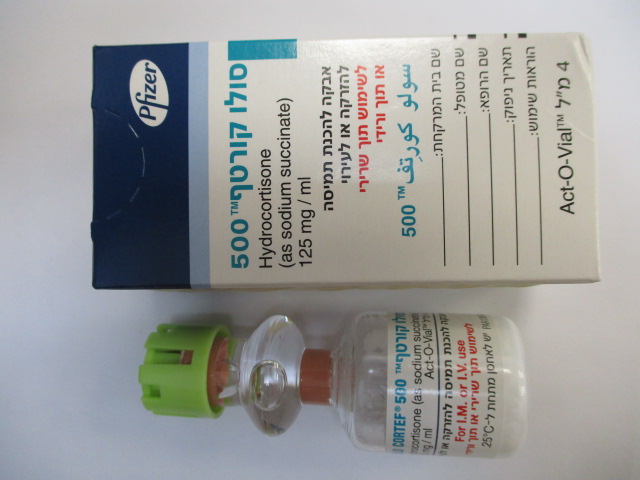
סולו קורטף 500 SOLU CORTEF 500 (HYDROCORTISONE AS SODIUM SUCCINATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-שרירי, תוך-ורידי : I.M, I.V
צורת מינון:
אבקה להמסה להזרקהאינפוזיה : POWDER FOR SOLUTION FOR INJ/INF
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
WARNINGS Serious Neurologic Adverse Reactions with Epidural Administration Serious neurologic events, some resulting in death, have been reported with epidural injection of corticosteroids. Specific events reported include, but are not limited to, spinal cord infarction, paraplegia, quadriplegia, cortical blindness, and stroke. These serious neurologic events have been reported with and without use of fluoroscopy. The safety and effectiveness of epidural administration of corticosteroids have not been established, and corticosteroids are not approved for this use. General: Injection of SOLU CORTEF® may result in dermal and/or subdermal changes forming depressions in the skin at the injection site. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy. Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy (see ADVERSE REACTIONS). Increased dosage of rapidly acting corticosteroids is indicated in patients on corticosteroid therapy subjected to any unusual stress before, during, and after the stressful situation. Results from one multicenter, randomized, placebo-controlled study with methylprednisolone hemisuccinate, an IV corticosteroid, showed an increase in early (at 2 weeks) and late (at 6 months) mortality in patients with cranial trauma who were determined not to have other clear indications for corticosteroid treatment. High doses of systemic corticosteroids, including SOLU CORTEF®, should not be used for the treatment of traumatic brain injury. Cardio-renal: Average and large doses of corticosteroids can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion. Literature reports suggest an apparent association between use of corticosteroids and left ventricular free wall rupture after a recent myocardial infarction; therefore, therapy with corticosteroids should be used with great caution in these patients. There have been cases reported in which concomitant use of amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (see CONTRAINDICATIONS and PRECAUTIONS: Drug Interactions, Amphotericin B injection and potassium-depleting agents). Endocrine: Hypothalamic-pituitary adrenal (HPA) axis suppression, Cushing’s syndrome, and hyperglycemia. Monitor patients for these conditions with chronic use. Corticosteroids can produce reversible HPA axis suppression with the potential for glucocorticosteroid insufficiency after withdrawal of treatment. Drug induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. Immunosuppression and Increased Risk of Infection Corticosteroids, including SOLU-CORTEF, suppress the immune system and increase the risk of infection with any pathogen, including viral, bacterial, fungal, protozoan, or helminthic pathogens. Corticosteroids can: • Reduce resistance to new infections • Exacerbate existing infections • Increase the risk of disseminated infections • Increase the risk of reactivation or exacerbation of latent infections • Mask some signs of infection Corticosteroid-associated infections can be mild but can be severe and at times fatal. The rate of infectious complications increases with increasing corticosteroid dosages. Monitor for the development of infection and consider SOLU-CORTEF withdrawal or dosage reduction as needed. Do not administer SOLU-CORTEF by an intraarticular, intrabursal, or intratendinous route in the presence of acute local infection. Tuberculosis If SOLU-CORTEF is used to treat a condition in patients with latent tuberculosis or tuberculin reactivity, reactivation of the disease may occur. Closely monitor such patients for reactivation. .During prolonged SOLU-CORTEF therapy, patients with latent tuberculosis or tuberculin reactivity should receive chemoprophylaxis. Varicella Zoster and Measles Viral Infections Varicella and measles can have a serious or even fatal course in non-immune patients taking corticosteroids. In corticosteroid-treated patients who have not had these diseases or are nonimmune, particular care should be taken to avoid exposure to varicella and measles: • If a SOLU-CORTEF-treated patient is exposed to varicella, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If varicella develops, treatment with antiviral agents may be considered. • If a SOLU-CORTEF-treated patient is exposed to measles, prophylaxis with immunoglobulin (IG) may be indicated. Hepatitis B Virus Reactivation Hepatitis B virus reactivation can occur in patients who are hepatitis B carriers treated with immunosuppressive dosages of corticosteroids, including SOLU-CORTEF. Reactivation can also occur infrequently in corticosteroid-treated patients who appear to have resolved hepatitis B infection. Screen patients for hepatitis B infection before initiating immunosuppressive (e.g., prolonged) treatment with SOLU-CORTEF. For patients who show evidence of hepatitis B infection, recommend consultation with physicians with expertise in managing hepatitis B regarding monitoring and consideration for hepatitis B antiviral therapy. Fungal Infections Corticosteroids, including SOLU-CORTEF, may exacerbate systemic fungal infections; therefore, avoid SOLU-CORTEF use in the presence of such infections unless SOLU- CORTEF is needed to control drug reactions. For patients on chronic SOLU-CORTEF therapy who develop systemic fungal infections, SOLU-CORTEF withdrawal or dosage reduction is recommended. Amebiasis Corticosteroids, including SOLU-CORTEF, may activate latent amebiasis. Therefore, it is recommended that latent amebiasis or active amebiasis be ruled out before initiating SOLU-CORTEF in patients who have spent time in the tropics or patients with unexplained diarrhea. Strongyloides Infestation Corticosteroids, including SOLU-CORTEF, should be used with great care in patients with known or suspected Strongyloides (threadworm) infestation. In such patients, corticosteroid-induced immunosuppression may lead to Strongyloides hyperinfection and dissemination with widespread larval migration, often accompanied by severe enterocolitis and potentially fatal gram-negative septicemia. Cerebral Malaria Avoid corticosteroids, including SOLU-CORTEF, in patients with cerebral malaria. Vaccination: Administration of live or live-attenuated vaccines is contraindicated in patients receiving immunosuppressive doses of corticosteroids. Killed or inactivated vaccines may be administered. However, the response to such vaccines cannot be predicted. Immunization procedures may be undertaken in patients who are receiving corticosteroids as replacement therapy (e.g., for Addison’s disease). Neurologic: Reports of severe medical events have been associated with the intrathecal route of administration (see ADVERSE REACTIONS, Neurologic/Psychiatric). Ophthalmic: Use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to bacteria, fungi, or viruses. The use of oral corticosteroids is not recommended in the treatment of optic neuritis and may lead to an increase in the risk of new episodes. Corticosteroids should be used cautiously in patients with ocular herpes simplex because of corneal perforation. Corticosteroids should not be used in active ocular herpes simplex. Kaposi’s Sarcoma: Kaposi’s sarcoma has been reported to occur in patients receiving corticosteroid therapy, most often for chronic conditions. Discontinuation of corticosteroids may result in clinical improvement of Kaposi’s sarcoma. PRECAUTIONS General: The lowest possible dose of corticosteroid should be used to control the condition under treatment. When reduction in dosage is possible, the reduction should be gradual. Since complications of treatment with glucocorticoids are dependent on the size of the dose and the duration of treatment, a risk/benefit decision must be made in each individual case as to dose and duration of treatment and as to whether daily or intermittent therapy should be used. Cardio-renal: As sodium retention with resultant edema and potassium loss may occur in patients receiving corticosteroids, these agents should be used with caution in patients with congestive heart failure, hypertension, or renal insufficiency. Endocrine: Drug-induced secondary adrenocortical insufficiency may be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. Metabolic clearance of corticosteroids is decreased in hypothyroid patients and increased in hyperthyroid patients. Changes in thyroid status of the patient may necessitate adjustment in dosage. Gastrointestinal: Steroids should be used with caution in active or latent peptic ulcers, diverticulitis, fresh intestinal anastomoses, and non-specific ulcerative colitis, since they may increase the risk of a perforation. Signs of peritoneal irritation following gastrointestinal perforation in patients receiving corticosteroids may be minimal or absent. There is an enhanced effect due to decreased metabolism of corticosteroids in patients with cirrhosis. Musculoskeletal: Corticosteroids decrease bone formation and increase bone resorption both through their effect on calcium regulation (e.g., decreasing absorption and increasing excretion) and inhibition of osteoblast function. This, together with a decrease in the protein matrix of the bone secondary to an increase in protein catabolism, and reduced sex hormone production, may lead to inhibition of bone growth in pediatric patients and the development of osteoporosis at any age. Special consideration should be given to patients at increased risk of osteoporosis (i.e., postmenopausal women) before initiating corticosteroid therapy. Local injection of a steroid into a previously infected site is not usually recommended. Neurologic-psychiatric: An acute myopathy has been observed with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (e.g., myasthenia gravis), or in patients receiving concomitant therapy with neuromuscular blocking drugs (e.g., pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevation of creatine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years. Psychic derangements may appear when corticosteroids are used, ranging from euphoria, insomnia, mood swings, personality changes, and severe depression to frank psychotic manifestations. Also, existing emotional instability or psychotic tendencies may be aggravated by corticosteroids. Ophthalmic: Intraocular pressure may become elevated in some individuals. If steroid therapy is continued for more than 6 weeks, intraocular pressure should be monitored. Other: Pheochromocytoma crisis, which can be fatal, has been reported after administration of systemic corticosteroids. In patients with suspected pheochromocytoma, consider the risk of pheochromocytoma crisis prior to administering corticosteroids. Tumor Lysis Syndrome: In post marketing experience tumor lysis syndrome (TLS) has been reported in patients with malignancies, including hematological malignancies and solid tumors, following the use of systemic corticosteroids alone or in combination with other chemotherapeutic agents. Patients at high risk of TLS, such as patients with tumors that have a high proliferative rate, high tumor burden and high sensitivity to cytotoxic agents, should be monitored closely and appropriate precautions should be taken.
Effects on Driving

שימוש לפי פנקס קופ''ח כללית 1994
Acute adrenocortical insufficiency, status asthmaticus, anaphylaxis
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
