Quest for the right Drug
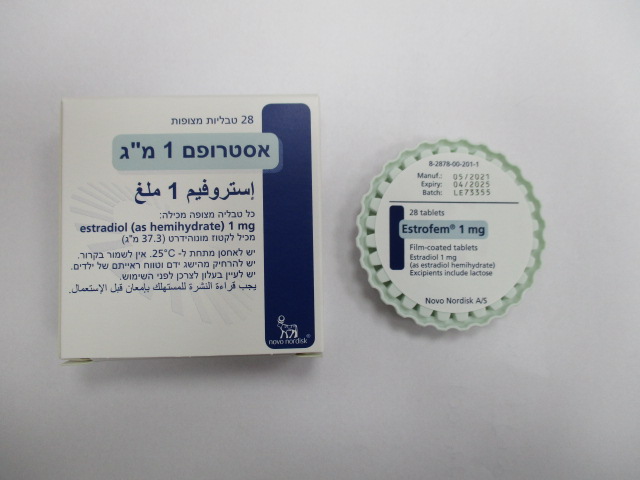
אסטרופם 1 מ"ג ESTROFEM 1 MG (ESTRADIOL AS HEMIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Clinical experience In clinical trials less than 10% of the patients experienced adverse drug reactions. The most frequently reported adverse reactions are breast tenderness/breast pain, abdominal pain, oedema, and headache. The adverse reactions listed below occurred in the clinical trials during Estrofem treatment. System organ Very common Common Uncommon Rare class > 1/10 > 1/100; > 1/1,000; > 1/10,000; < 1/10 < 1/100 < 1/1,000 Psychiatric Depression disorders Nervous system Headache disorders Eye disorders Vision abnormal Vascular Venous disorders embolism Gastrointestinal Abdominal pain Dyspepsia, disorders or nausea vomiting, flatulence or bloating Hepatobiliary Cholelithiasis disorders Skin and Rash or urticaria subcutaneous tissue disorders Musculoskeletal Leg cramps and connective tissue disorders Reproductive Breast system and breast tenderness, disorders breast enlargement or breast pain General Oedema disorders and administration site conditions System organ Very common Common Uncommon Rare class > 1/10 > 1/100; > 1/1,000; > 1/10,000; < 1/10 < 1/100 < 1/1,000 Investigations Weight increased Post-marketing experience In addition to the above mentioned adverse drug reactions, those presented below have been spontaneously reported, and are by an overall judgment considered possibly related to Estrofem treatment. The reporting rate of these spontaneous adverse drug reactions is very rare (< 1/10,000, not known (cannot be estimated from the available data)). Post-marketing experience is subject to underreporting especially with regard to trivial and well-known adverse drug reactions. The presented frequencies should be interpreted in that light: – Immune system disorder: Generalised hypersensitivity reactions (e.g. anaphylactic reaction/shock) – Nervous system disorder: Deterioration of migraine, stroke, dizziness, depression – Gastrointestinal disorder: Diarrhoea – Skin and subcutaneous tissue disorders: Alopecia – Reproductive system and breast disorders: Irregular vaginal bleeding* – Investigations: Increased blood pressure. The following adverse reactions have been reported in association with other oestrogen treatment: – Myocardial infarction, congestive heart disease – Venous thromboembolism, i.e. deep leg or pelvic venous thrombosis and pulmonary embolism – Gall bladder disease – Skin and subcutaneous disorders: chloasma, erythema multiforme, erythema nodosum, vascular purpura, pruritus – Vaginal candidiasis – Oestrogen-dependent neoplasms benign and malignant. e.g. endometrial cancer (see section 4.4), endometrial hyperplasia or increase in size of uterine fibroids* – Insomnia – Epilepsy – Libido disorder NOS (not otherwise specified) – Deterioration of asthma – Probable dementia (see section 4.4). * In non-hysterectomised women Breast cancer risk The increased risk in users of oestrogen-only therapy is lower than that seen in users of oestrogen- progestagen combinations. The level of risk is dependent on the duration of use (see section 4.4). Absolute risk estimations based on results of the largest randomised placebo-controlled trial (WHI study) and the largest meta-analysis of prospective epidemiological studies are presented below. Largest meta-analysis of prospective epidemiological studies Estimated additional risk of breast cancer after 5 years’ use in women with BMI 27 (kg/m²) Age at start Incidence per 1,000 Risk ratio Additional cases per HRT never-users of HRT 1,000 HRT users (years) over a 5-year period after 5 years (50-54 years)* Oestrogen-only HRT 50 13.3 1.2 2.7 Combined oestrogen-progestagen 50 13.3 1.6 8.0 * Taken from baseline incidence rates in England in 2015 in women with BMI 27 (kg/m²). Note: Since the background incidence of breast cancer differs by EU country, the number of additional cases of breast cancer will also change proportionally. Estimated additional risk of breast cancer after 10 years’ use in women with BMI 27 (kg/m²) Age at start Incidence per 1,000 Risk ratio Additional cases per HRT never-users of HRT 1,000 HRT users (years) over a 10 year period after 10 years (50-59 years)* Oestrogen-only HRT 50 26.6 1.3 7.1 Combined oestrogen-progestagen 50 26.6 1.8 20.8 * Taken from baseline incidence rates in England in 2015 in women with BMI 27 (kg/m²). Note: Since the background incidence of breast cancer differs by EU country, the number of additional cases of breast cancer will also change proportionately. US WHI Studies – Additional risk of breast cancer after 5 years’ use Age range Incidence per 1,000 Risk ratio and Additional cases per (years) women in placebo 95% CI 1,000 HRT users arm over 5 years over 5 years (95% CI) CEE oestrogen-only 50-79 21 0.8 (0.7-1.0) -4 (-6-0)* CEE+MPA oestrogen-progestagen** 50-79 17 1.2 (1.0-1.5) 4 (0-9) * WHI study in women with no uterus which did not show an increase in risk of breast cancer. ** When the analysis was restricted to women who had not used HRT prior to the study, there was no increased risk apparent during the first 5 years of treatment. After 5 years the risk was higher than in non-users. Endometrial cancer risk Postmenopausal women with a uterus The endometrial cancer risk is about 5 in every 1,000 women with a uterus not using HRT. In women with a uterus, use of oestrogen-only HRT is not recommended because it increases the risk of endometrial cancer (see section 4.4). Depending on the duration of oestrogen-only use and oestrogen dose, the increase in risk of endometrial cancer in epidemiological studies varied from between 5 and 55 extra cases diagnosed in every 1,000 women between the ages of 50 and 65. Adding a progestagen to oestrogen-only therapy for at least 12 days per cycle can prevent this increased risk. In the Million Women Study the use of 5 years of combined (sequential or continuous) HRT did not increase the risk of endometrial cancer (RR of 1.0 (0.8-1.2)). Ovarian cancer risk Use of oestrogen-only or combined oestrogen-progestagen HRT has been associated with a slightly increased risk of having ovarian cancer diagnosed (see section 4.4). A meta-analysis from 52 epidemiological studies reported an increased risk of ovarian cancer in women currently using HRT compared to women who have never used HRT (RR 1.43, 95% CI 1.31- 1.56). For women aged 50 to 54 years taking 5 years of HRT, this results in about 1 extra case per 2,000 users. In women aged 50 to 54 who are not taking HRT, about 2 women in 2,000 will be diagnosed with ovarian cancer over a 5-year period. Risk of venous thromboembolism HRT is associated with a 1.3 to 3-fold increased relative risk of developing venous thromboembolism (VTE), i.e. deep vein thrombosis or pulmonary embolism. The occurrence of such an event is more likely in the first year of using HRT (see section 4.4). Results of the WHI studies are presented below. WHI Studies – Additional risk of VTE over 5 years’ use Age range (years) Incidence per Risk ratio and Additional cases 1,000 women in 95% CI per 1,000 HRT placebo arm over users over 5 years 5 years (95% CI) Oral oestrogen-only* 50-59 7 1.2 (0.6-2.4) 1 (-3-10) Oral combined oestrogen-progestagen 50-59 4 2.3 (1.2-4.3) 5 (1-13) * Study in women with no uterus Risk of coronary artery disease The risk of coronary artery disease is slightly increased in users of combined oestrogen-progestagen HRT over the age of 60 (see section 4.4). Risk of ischaemic stroke The use of oestrogen-only and oestrogen-progestagen therapy is associated with an up to 1.5-fold increased relative risk of ischaemic stroke. The risk of haemorrhagic stroke is not increased during use of HRT. This relative risk is not dependent on age or on duration of use, but the baseline risk is strongly age- dependent. The overall risk of stroke in women who use HRT will increase with age (see section 4.4). WHI Studies Combined – Additional risk of ischaemic stroke* over 5 years’ use Age range Incidence per 1,000 Risk ratio and Additional cases per (years) women in placebo arm 95% CI 1,000 HRT users over 5 years over 5 years (95% CI) 50-59 8 1.3 (1.1-1.6) 3 (1-5) * No differentiation was made between ischaemic and haemorrhagic stroke. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: /https://sideeffects.health.gov.il.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/10/2005
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
24.01.21 - עלון לצרכן אנגלית 24.01.21 - עלון לצרכן עברית 24.01.21 - עלון לצרכן ערבית 13.12.23 - עלון לצרכן עברית 29.02.24 - עלון לצרכן אנגלית 29.02.24 - עלון לצרכן עברית 29.02.24 - עלון לצרכן ערבית 31.07.13 - החמרה לעלון 16.08.16 - החמרה לעלון 13.01.21 - החמרה לעלון 11.01.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אסטרופם 1 מ"ג