Quest for the right Drug
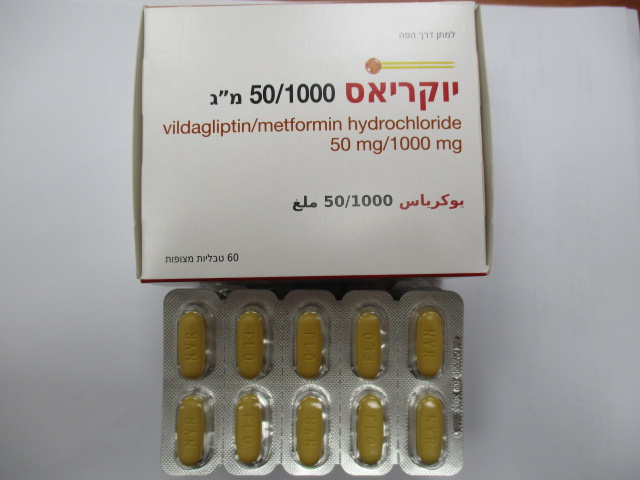
יוקריאס 50/1000 מ"ג EUCREAS 50/1000 MG (METFORMIN HYDROCHLORIDE, VILDAGLIPTIN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Drugs used in diabetes, combinations of oral blood glucose lowering drugs, ATC code: A10BD08. Mechanism of action Eucreas combines two antihyperglycaemic agents with complimentary mechanisms of action to improve glycaemic control in patients with type 2 diabetes: vildagliptin, a member of the islet enhancer class, and metformin hydrochloride, a member of the biguanide class. Vildagliptin, a member of the islet enhancer class, is a potent and selective dipeptidyl-peptidase-4 (DPP-4) inhibitor. Metformin acts primarily by decreasing endogenous hepatic glucose production. Pharmacodynamic effects Vildagliptin Vildagliptin acts primarily by inhibiting DPP-4, the enzyme responsible for the degradation of the incretin hormones GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). The administration of vildagliptin results in a rapid and complete inhibition of DPP-4 activity resulting in increased fasting and postprandial endogenous levels of the incretin hormones GLP-1 and GIP. By increasing the endogenous levels of these incretin hormones, vildagliptin enhances the sensitivity of beta cells to glucose, resulting in improved glucose-dependent insulin secretion. Treatment with vildagliptin 50-100 mg daily in patients with type 2 diabetes significantly EUC API SEP22 V3 EU SmPC 07.2022 improved markers of beta cell function including HOMA-β (Homeostasis Model Assessment–β), proinsulin to insulin ratio and measures of beta cell responsiveness from the frequently-sampled meal tolerance test. In non-diabetic (normal glycaemic) individuals, vildagliptin does not stimulate insulin secretion or reduce glucose levels. By increasing endogenous GLP-1 levels, vildagliptin also enhances the sensitivity of alpha cells to glucose, resulting in more glucose-appropriate glucagon secretion. The enhanced increase in the insulin/glucagon ratio during hyperglycaemia due to increased incretin hormone levels results in a decrease in fasting and postprandial hepatic glucose production, leading to reduced glycaemia. The known effect of increased GLP-1 levels delaying gastric emptying is not observed with vildagliptin treatment. Metformin Metformin is a biguanide with antihyperglycaemic effects, lowering both basal and postprandial plasma glucose. It does not stimulate insulin secretion and therefore does not produce hypoglycaemia or increased weight gain. Metformin may exert its glucose-lowering effect via three mechanisms: - by reduction of hepatic glucose production through inhibition of gluconeogenesis and glycogenolysis; - in muscle, by modestly increasing insulin sensitivity, improving peripheral glucose uptake and utilisation; - by delaying intestinal glucose absorption. Metformin stimulates intracellular glycogen synthesis by acting on glycogen synthase and increases the transport capacity of specific types of membrane glucose transporters (GLUT-1 and GLUT-4). In humans, independently of its action on glycaemia, metformin has favourable effects on lipid metabolism. This has been shown at therapeutic doses in controlled, medium-term or long-term clinical studies: metformin reduces serum levels of total cholesterol, LDL cholesterol and triglycerides. The prospective randomised UKPDS (UK Prospective Diabetes Study) study has established the long-term benefit of intensive blood glucose control in type 2 diabetes. Analysis of the results for overweight patients treated with metformin after failure of diet alone showed: - a significant reduction in the absolute risk of any diabetes-related complication in the metformin group (29.8 events/1000 patient-years) versus diet alone (43.3 events/1000 patient-years), p=0.0023, and versus the combined sulphonylurea and insulin monotherapy groups (40.1 events/1000 patient-years), p=0.0034; - a significant reduction in the absolute risk of diabetes-related mortality: metformin 7.5 events/1000 patient-years, diet alone 12.7 events/1000 patient-years, p=0.017; - a significant reduction in the absolute risk of overall mortality: metformin 13.5 events/1000 patient-years versus diet alone 20.6 events/1000 patient-years (p=0.011), and versus the combined sulphonylurea and insulin monotherapy groups 18.9 events/1000 patient-years (p=0.021); - a significant reduction in the absolute risk of myocardial infarction: metformin 11 events/1000 patient-years, diet alone 18 events/1000 patient-years (p=0.01). Clinical efficacy and safety EUC API SEP22 V3 EU SmPC 07.2022 Vildagliptin added to patients whose glycaemic control was not satisfactory despite treatment with metformin monotherapy resulted after 6-month treatment in additional statistically significant mean reductions in HbA1c compared to placebo (between group differences of -0.7% to -1.1% for vildagliptin 50 mg and 100 mg, respectively). The proportion of patients who achieved a decrease in HbA1c of ≥ 0.7% from baseline was statistically significantly higher in both vildagliptin plus metformin groups (46% and 60%, respectively) versus the metformin plus placebo group (20%). In a 24-week trial, vildagliptin (50 mg twice daily) was compared to pioglitazone (30 mg once daily) in patients inadequately controlled with metformin (mean daily dose: 2020 mg). Mean reductions from baseline HbA1c of 8.4% were -0.9% with vildagliptin added to metformin and -1.0% with pioglitazone added to metformin. A mean weight gain of +1.9 kg was observed in patients receiving pioglitazone added to metformin compared to +0.3 kg in those receiving vildagliptin added to metformin. In a clinical trial of 2 years’ duration, vildagliptin (50 mg twice daily) was compared to glimepiride (up to 6 mg/day – mean dose at 2 years: 4.6 mg) in patients treated with metformin (mean daily dose: 1894 mg). After 1 year mean reductions in HbA1c were -0.4% with vildagliptin added to metformin and -0.5% with glimepiride added to metformin, from a mean baseline HbA1c of 7.3%. Body weight change with vildagliptin was -0.2 kg vs +1.6 kg with glimepiride. The incidence of hypoglycaemia was significantly lower in the vildagliptin group (1.7%) than in the glimepiride group (16.2%). At study endpoint (2 years), the HbA1c was similar to baseline values in both treatment groups and the body weight changes and hypoglycaemia differences were maintained. In a 52-week trial, vildagliptin (50 mg twice daily) was compared to gliclazide (mean daily dose: 229.5 mg) in patients inadequately controlled with metformin (metformin dose at baseline 1928 mg/day). After 1 year, mean reductions in HbA1c were -0.81% with vildagliptin added to metformin (mean baseline HbA1c 8.4%) and -0.85% with gliclazide added to metformin (mean baseline HbA1c 8.5%); statistical non-inferiority was achieved (95% CI -0.11 – 0.20). Body weight change with vildagliptin was +0.1 kg compared to a weight gain of +1.4 kg with gliclazide. In a 24-week trial the efficacy of the fixed dose combination of vildagliptin and metformin (gradually titrated to a dose of 50 mg/500 mg twice daily or 50 mg/1000 mg twice daily) as initial therapy in drug-naïve patients was evaluated. Vildagliptin/ metformin 50 mg/1000 mg twice daily reduced HbA1c by -1.82%, vildagliptin/metformin 50 mg/500 mg twice daily by -1.61% metformin 1000 mg twice daily by -1.36% and vildagliptin 50 mg twice daily by -1.09% from a mean baseline HbA1c of 8.6%. The decrease in HbA1c observed in patients with a baseline ≥ 10.0% was greater. A 24-week randomised, double-blind, placebo-controlled trial was conducted in 318 patients to evaluate the efficacy and safety of vildagliptin (50 mg twice daily) in combination with metformin (≥ 1500 mg daily) and glimepiride (≥4 mg daily). Vildagliptin in combination with metformin and glimepiride significantly decreased HbA1c compared with placebo. The placebo- adjusted mean reduction from a mean baseline HbA1c of 8.8% was -0.76%. A five-year multi-centre, randomised, double-blind study (VERIFY) was conducted in patients with type 2 diabetes to evaluate the effect of an early combination therapy with EUC API SEP22 V3 EU SmPC 07.2022 vildagliptin and metformin (N = 998) against standard-of-care initial metformin monotherapy followed by combination with vildagliptin (sequential treatment group) (N = 1,003) in newly diagnosed patients with type 2 diabetes. The combination regimen of vildagliptin 50 mg twice daily plus metformin resulted in a statistically and clinically significant relative reduction in hazard for “time to confirmed initial treatment failure” (HbA1c value ≥7%) vs metformin monotherapy in treatment-naïve patients with type 2 diabetes over the 5-year study duration (HR [95%CI]: 0.51 [0.45, 0.58]; p<0.001). The incidence of initial treatment failure (HbA1c value ≥7%) was 429 (43.6%) patients in the combination treatment group and 614 (62.1%) patients in the sequential treatment group. A 24-week randomised, double-blind, placebo-controlled trial was conducted in 449 patients to evaluate the efficacy and safety of vildagliptin (50 mg twice daily) in combination with a stable dose of basal or premixed insulin (mean daily dose 41 units), with concomitant use of metformin (N = 276) or without concomitant metformin (N = 173). Vildagliptin in combination with insulin significantly decreased HbA1c compared with placebo. In the overall population, the placebo- adjusted mean reduction from a mean baseline HbA1c 8.8% was -0.72%. In the subgroups treated with insulin with or without concomitant metformin the placebo-adjusted mean reduction in HbA1c was -0.63% and -0.84%, respectively. The incidence of hypoglycaemia in the overall population was 8.4% and 7.2% in the vildagliptin and placebo groups, respectively. Patients receiving vildagliptin experienced no weight gain (+0.2 kg) while those receiving placebo experienced weight reduction (-0.7 kg). In another 24-week study in patients with more advanced type 2 diabetes not adequately controlled on insulin (short and longer acting, average insulin dose 80 IU/day), the mean reduction in HbA1c when vildagliptin (50 mg twice daily) was added to insulin was statistically significantly greater than with placebo plus insulin (0.5% vs. 0.2%). The incidence of hypoglycaemia was lower in the vildagliptin group than in the placebo group (22.9% vs. 29.6%). Cardiovascular risk A meta-analysis of independently and prospectively adjudicated cardiovascular events from 37 phase III and IV monotherapy and combination therapy clinical studies of up to more than 2 years duration (mean exposure 50 weeks for vildagliptin and 49 weeks for comparators) was performed and showed that vildagliptin treatment was not associated with an increase in cardiovascular risk versus comparators. The composite endpoint of adjudicated major adverse cardiovascular events (MACE) including acute myocardial infarction, stroke or cardiovascular death was similar for vildagliptin versus combined active and placebo comparators [Mantel–Haenszel risk ratio (M-H RR) 0.82 (95% CI 0.61-1.11)]. A MACE occurred in 83 out of 9,599 (0.86%) vildagliptin-treated patients and in 85 out of 7,102 (1.20%) comparator-treated patients. Assessment of each individual MACE component showed no increased risk (similar M-H RR). Confirmed heart failure (HF) events defined as HF requiring hospitalisation or new onset of HF were reported in 41 (0.43%) vildagliptin-treated patients and 32 (0.45%) comparator-treated patients with M-H RR 1.08 (95% CI 0.68-1.70).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Eucreas Absorption EUC API SEP22 V3 EU SmPC 07.2022 Bioequivalence has been demonstrated between Eucreas at three dose strengths (50 mg/500 mg, 50 mg/850 mg and 50 mg/1000 mg) versus free combination of vildagliptin and metformin hydrochloride tablets at the corresponding doses. Food does not affect the extent and rate of absorption of vildagliptin from Eucreas. The rate and extent of absorption of metformin from Eucreas 50 mg/1000 mg were decreased when given with food as reflected by the decrease in Cmax by 26%, AUC by 7% and delayed Tmax (2.0 to 4.0 h). The following statements reflect the pharmacokinetic properties of the individual active substances of Eucreas. Vildagliptin Absorption Following oral administration in the fasting state, vildagliptin is rapidly absorbed with peak plasma concentrations observed at 1.7 hours. Food slightly delays the time to peak plasma concentration to 2.5 hours, but does not alter the overall exposure (AUC). Administration of vildagliptin with food resulted in a decreased Cmax (19%) compared to dosing in the fasting state. However, the magnitude of change is not clinically significant, so that vildagliptin can be given with or without food. The absolute bioavailability is 85%. Distribution The plasma protein binding of vildagliptin is low (9.3%) and vildagliptin distributes equally between plasma and red blood cells. The mean volume of distribution of vildagliptin at steady- state after intravenous administration (Vss) is 71 litres, suggesting extravascular distribution. Biotransformation Metabolism is the major elimination pathway for vildagliptin in humans, accounting for 69% of the dose. The major metabolite (LAY 151) is pharmacologically inactive and is the hydrolysis product of the cyano moiety, accounting for 57% of the dose, followed by the amide hydrolysis product (4% of dose). DPP-4 contributes partially to the hydrolysis of vildagliptin based on an in vivo study using DPP-4 deficient rats. Vildagliptin is not metabolised by CYP 450 enzymes to any quantifiable extent, and accordingly the metabolic clearance of vildagliptin is not anticipated to be affected by co-medications that are CYP 450 inhibitors and/or inducers. In vitro studies demonstrated that vildagliptin does not inhibit/induce CYP 450 enzymes. Therefore, vildagliptin is not likely to affect metabolic clearance of co-medications metabolised by CYP 1A2, CYP 2C8, CYP 2C9, CYP 2C19, CYP 2D6, CYP 2E1 or CYP 3A4/5. Elimination 14 Following oral administration of [ C] vildagliptin, approximately 85% of the dose was excreted into the urine and 15% of the dose was recovered in the faeces. Renal excretion of the unchanged vildagliptin accounted for 23% of the dose after oral administration. After intravenous administration to healthy subjects, the total plasma and renal clearances of vildagliptin are 41 and 13 l/h, respectively. The mean elimination half-life after intravenous administration is approximately 2 hours. The elimination half-life after oral administration is approximately 3 hours. Linearity / non-linearity The Cmax for vildagliptin and the area under the plasma concentrations versus time curves (AUC) increased in an approximately dose proportional manner over the therapeutic dose range. Characteristics in patients EUC API SEP22 V3 EU SmPC 07.2022 Gender: No clinically relevant differences in the pharmacokinetics of vildagliptin were observed between male and female healthy subjects within a wide range of age and body mass index (BMI). DPP-4 inhibition by vildagliptin is not affected by gender. Age: In healthy elderly subjects (≥ 70 years), the overall exposure of vildagliptin (100 mg once daily) was increased by 32%, with an 18% increase in peak plasma concentration as compared to young healthy subjects (18-40 years). These changes are not considered to be clinically relevant, however. DPP-4 inhibition by vildagliptin is not affected by age. Hepatic impairment: In subjects with mild, moderate or severe hepatic impairment (Child-Pugh A-C) there were no clinically significant changes (maximum ~30%) in exposure to vildagliptin. Renal impairment: In subjects with mild, moderate, or severe renal impairment, systemic exposure to vildagliptin was increased (Cmax 8-66%; AUC 32-134%) and total body clearance was reduced compared to subjects with normal renal function. Ethnic group: Limited data suggest that race does not have any major influence on vildagliptin pharmacokinetics. Metformin Absorption After an oral dose of metformin, the maximum plasma concentration (Cmax) is achieved after about 2.5 h. Absolute bioavailability of a 500 mg metformin tablet is approximately 50-60% in healthy subjects. After an oral dose, the non-absorbed fraction recovered in faeces was 20-30%. After oral administration, metformin absorption is saturable and incomplete. It is assumed that the pharmacokinetics of metformin absorption are non-linear. At the usual metformin doses and dosing schedules, steady state plasma concentrations are reached within 24-48 h and are generally less than 1 μg/ml. In controlled clinical trials, maximum metformin plasma levels (Cmax) did not exceed 4 μg/ml, even at maximum doses. Food slightly delays and decreases the extent of the absorption of metformin. Following administration of a dose of 850 mg, the plasma peak concentration was 40% lower, AUC was decreased by 25% and time to peak plasma concentration was prolonged by 35 minutes. The clinical relevance of this decrease is unknown. Distribution Plasma protein binding is negligible. Metformin partitions into erythrocytes. The mean volume of distribution (Vd) ranged between 63-276 litres. Biotransformation Metformin is excreted unchanged in the urine. No metabolites have been identified in humans. Elimination Metformin is eliminated by renal excretion. Renal clearance of metformin is > 400 ml/min, indicating that metformin is eliminated by glomerular filtration and tubular secretion. Following an oral dose, the apparent terminal elimination half-life is approximately 6.5 h. When renal function is impaired, renal clearance is decreased in proportion to that of creatinine and thus the elimination half-life is prolonged, leading to increased levels of metformin in plasma.

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
27.10.21 - עלון לצרכן אנגלית 27.10.21 - עלון לצרכן עברית 27.10.21 - עלון לצרכן ערבית 12.10.22 - עלון לצרכן עברית 14.12.22 - עלון לצרכן אנגלית 14.12.22 - עלון לצרכן ערבית 22.02.15 - החמרה לעלון 18.10.15 - החמרה לעלון 23.08.20 - החמרה לעלון 25.11.20 - החמרה לעלון 02.09.21 - החמרה לעלון 12.10.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
יוקריאס 50/1000 מ"ג