Quest for the right Drug
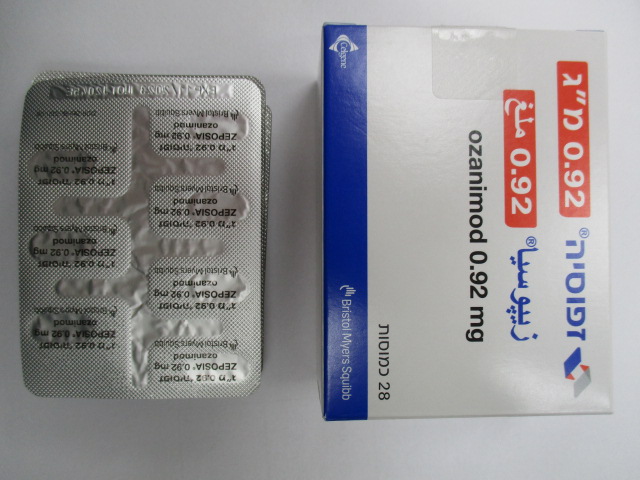
זפוסיה 0.92 מ"ג ZEPOSIA 0.92 MG (OZANIMOD AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Immunosuppressants, Sphingosine-1-phosphate (S1P) receptor modulators, ATC code: L04AE02 Mechanism of action Ozanimod is a potent sphingosine 1-phosphate (S1P) receptor modulator, which binds with high affinity to sphingosine 1-phosphate receptors 1 and 5. Ozanimod has minimal or no activity on S1P 2, S1P3, and S1P4. In vitro, ozanimod and its major active metabolites demonstrated similar activity and selectivity for S1P1 and S1P5. The mechanism by which ozanimod exerts therapeutic effects in MS and UC is unknown, but may involve the reduction of lymphocyte migration into the central nervous system (CNS) and intestine. The ozanimod-induced reduction of lymphocytes in the peripheral circulation has differential effects on leucocyte subpopulations, with greater decreases in cells involved in the adaptive immune response. Ozanimod has minimal impact on cells involved in innate immune response, which contribute to immunosurveillance. Ozanimod is extensively metabolised in humans to form a number of circulating active metabolites including two major metabolites (see section 5.2). In humans, approximately 94% of circulating total active substances exposure are represented by ozanimod (6%) and the two major metabolites CC112273 (73%), and CC1084037 (15%) (see section 5.2). Pharmacodynamic effects Reduction of peripheral blood lymphocytes In active-controlled MS and placebo-controlled UC clinical studies, mean lymphocyte counts decreased to approximately 45% of baseline by 3 months (approximate mean blood lymphocyte count 0.8 x 109/L) and remained stable during treatment with ozanimod. After discontinuing ozanimod 0.92 mg, the median time to recovery of peripheral blood lymphocytes to the normal range was approximately 30 days, with approximately 80% to 90% of patients recovering to normal within 3 months (see sections 4.4 and 4.8). Reduction in faecal calprotectin (FCP) In patients with UC, treatment with ozanimod resulted in a decrease in the inflammatory marker, faecal calprotectin (FCP) during the induction period, which was then maintained throughout the maintenance period. Heart rate and rhythm Ozanimod may cause a transient reduction in HR on initiation of dosing (see sections 4.4 and 4.8). This negative chronotropic effect is mechanistically related to the activation of G-protein-coupled inwardly rectifying potassium (GIRK) channels via S1P1 receptor stimulation by ozanimod and its active metabolites leading to cellular hyperpolarisation and reduced excitability with a maximal effect on HR seen within 5 hours post dose. Due to its functional antagonism at S1P 1 receptors, a dose escalation schedule with ozanimod 0.23 mg followed by 0.46 mg, and 0.92 mg successively desensitises GIRK channels until the maintenance dose is reached. After the dose escalation period, with continued administration of ozanimod, HR returns to baseline. Potential to prolong the QT interval In a randomised, positive - and placebo-controlled thorough QT study using a 14-day dose-escalation regimen of 0.23 mg daily for 4 days, 0.46 mg daily for 3 days, 0.92 mg daily for 3 days, and 1.84 mg daily for 4 days in healthy subjects, no evidence of QTc prolongation was observed as demonstrated by the upper boundary of the 95% one-sided confidence interval (CI) that was below the 10 ms. Concentration-QTc analysis for ozanimod and the major active metabolites CC112273 and CC1084037, using data from another Phase 1 study showed the upper boundary of the 95% CI for model derived QTc (corrected for placebo and baseline) below 10 ms at maximum concentrations achieved with ozanimod doses ≥ 0.92 mg once daily. Clinical efficacy and safety Multiple sclerosis Ozanimod was evaluated in two Phase 3 randomised, double-blind, double-dummy, parallel-group, active controlled clinical trials of similar design and endpoints, in patients with relapsing remitting MS (RRMS). Study 1 – SUNBEAM, was a 1-year study with patients continuing assigned treatment beyond month 12 until the last enrolled patient completed the study. Study 2 -RADIANCE was a 2-year study. The dose of ozanimod was 0.92 mg and 0.46 mg given orally once daily, with a starting dose of 0.23 mg on days 1-4, followed by an escalation to 0.46 mg on days 5-7, and followed by the assigned dose on day 8 and thereafter. The dose of IFN β-1a, the active comparator, was 30 mcg given intramuscularly once weekly. Both studies included patients with active disease as defined by having at least one relapse within the prior year, or one relapse within the prior two years with evidence of at least a gadolinium-enhancing (GdE) lesion in the prior year and had an Expanded Disability Status Scale (EDSS) score from 0 to 5.0. Neurological evaluations were performed at baseline, every 3 months, and at the time of a suspected relapse. MRIs were performed at baseline (Studies 1 and 2), 6 months (SUNBEAM), 1 year (Studies 1 and 2), and 2 years (RADIANCE). The primary outcome of both SUNBEAM and RADIANCE was the annualised relapse rate (ARR) over the treatment period (minimum of 12 months) for SUNBEAM and 24 months for RADIANCE. The key secondary outcome measures included 1) the number of new or enlarging MRI T2 hyperintense lesions over 12 and 24 months; 2) the number of MRI T1 GdE lesions at 12 and 24 months; and 3) the time to confirmed disability progression, defined as at least a 1-point increase from baseline EDSS sustained for 12 weeks. Confirmed disability progression was prospectively evaluated in a pooled analysis of Studies 1 and 2. In SUNBEAM, 1346 patients were randomised to receive ozanimod 0.92 mg (n = 447), ozanimod 0.46 mg (n = 451), or IFN β-1a IM (n = 448); 94% of ozanimod treated 0.92 mg, 94% of ozanimod treated 0.46 mg, and 92% of IFN β-1a IM treated patients completed the study. In RADIANCE, 1313 patients were randomised to receive ozanimod 0.92 mg (n = 433), ozanimod 0.46 mg (n = 439), or IFN β-1a IM (n = 441); 90% of ozanimod treated 0.92 mg, 85% of ozanimod treated 0.46 mg, and 85% of IFN β-1a IM treated patients completed the study. Patients enrolled across the 2 studies had a mean age of 35.5 years (range 18-55), 67% were female, mean time since MS symptom onset was 6.7 years. The median EDSS score at baseline was 2.5; approximately one-third of the patients had been treated with a disease-modifying therapy (DMT), predominately interferon or glatiramer acetate. At baseline, the mean number of relapses in the prior year was 1.3 and 45% of patients had one or more T1 Gd-enhancing lesions (mean 1.7). The results for SUNBEAM and RADIANCE are shown in Table 3. The efficacy has been demonstrated for ozanimod 0.92 mg with a dose effect observed for study endpoints shown in Table 3. Demonstration of efficacy for 0.46 mg was less robust since this dose did not show a significant effect for the primary endpoint in RADIANCE when considering the preferred negative binomial model strategy. Table 3: Key clinical and MRI endpoints in RMS patients from Study 1 - SUNBEAM and Study 2 - RADIANCE Endpoints SUNBEAM RADIANCE (≥ 1 year)* (2 year) Ozanimod IFN β-1a IM Ozanimod IFN β-1a IM 0.92 mg 30 mcg 0.92 mg 30 mcg (n = 447) (n = 448) (n = 433) (n = 441) % % % % Clinical endpoints Annualized relapse rate 0.181 0.350 0.172 0.276 (Primary endpoint) 48% (p < 0.0001) 38% (p < 0.0001) Relative reduction Proportion relapse-free ** 78% 76% 66% 64% (p = 0.0002)1 (p = 0.0012)1 Proportion with 3-month confirmed disability 7.6% Ozanimod vs. 7.8% IFN β-1a IM Progression (CDP)†2 0.95 (0.679, 1.330) Hazard ratio (95% CI) Proportion with 6-month 5.8% Ozanimod vs. 4.0% IFN β-1a IM CDP†2# 1.413 (0.922, 2.165) Hazard ratio (95% CI) MRI endpoints Mean number of new or 1.465 2.836 1.835 3.183 enlarging T2 hyperintense lesions per MRI3 48% (p < 0.0001) 42% (p < 0.0001) Relative reduction Mean number of T1 Gd 0.160 0.433 0.176 0.373 enhancing lesions4 63% (p < 0.0001) 53% (p = 0.0006) Relative reduction * Mean duration was 13.6 months ** Nominal p-value for endpoints not included in the hierarchical testing and not adjusted for multiplicity † Disability progression defined as 1-point increase in EDSS confirmed 3 months or 6 months later # In a post hoc analysis of 6-month CDP which included data from the open-label extension (Study 3), the HR (95% CI) was found to be 1.040 (0.730, 1.482).) 1 Log rank test 2 Prospectively planned pooled analysis of Studies 1 and 2 3 Over 12 months for Study 1 and over 24 months for Study 2 4 At 12 months for Study 1 and at 24 months for Study 2 In SUNBEAM and RADIANCE, treatment with ozanimod 0.92 mg resulted in reductions in mean percent change from baseline in normalised brain volume compared to IFN beta-1a IM (-0.41% versus -0.61%, and -0.71% versus -0.94%, respectively, nominal p-value < 0.0001 for both studies). The studies enrolled DMT naive and previously treated patients with active disease, as defined by clinical or imaging features. Post-hoc analyses of patient populations with differing baseline levels of disease activity, including active and highly active disease, showed that the efficacy of ozanimod on clinical and imaging endpoints was consistent with the overall population. Long-term Data Patients with RRMS who completed the SUNBEAM, RADIANCE, Phase 2 extension or Phase 1 PK/PD studies could enter an open-label extension (Study 3 - DAYBREAK) and received ozanimod 0.92 mg once daily to assess the long-term safety and efficacy of ZEPOSIA. In total, 2494 subjects were treated in DAYBREAK with ozanimod 0.92 mg once daily (736 patients switched from interferon beta-1a IM 30 mcg once weekly, 877 switched from ozanimod 0.46 mg once daily, and 881 continued with ozanimod 0.92 mg once daily) with a median duration of treatment of 68 months up to a maximum of 81 months. The adjusted annualised relapse rate (ARR) for all subjects over the treatment period was 0.098 (95% CI: 0.082, 0.117) with 69.1% of patients remaining relapse free. Subjects who continued on ozanimod 0.92 mg into DAYBREAK had an ARR of 0.090 (95% CI: 0.073, 0.111). A total of 379 (15.2%) of subjects experienced 6-month confirmed disability progression over the study. Ulcerative colitis The efficacy and safety of ozanimod were evaluated in two multicentre, randomised, double-blind, placebo-controlled clinical studies [TRUENORTH-I (induction period) and TRUENORTH-M (maintenance period)] in adult patients, aged less than 75 years, with moderately to severely active ulcerative colitis. TRUENORTH-I included patients who were randomised 2:1 to ozanimod 0.92 mg or placebo. The 10-week induction period (TRUENORTH-I) was followed by a 42-week, randomised, withdrawal maintenance period (TRUENORTH-M) for a total of 52 weeks of therapy. Ozanimod was administered as monotherapy (i.e., without concomitant use of biologics and non-corticosteroid immunosuppressants) for UC. The study included patients with moderately to severely active ulcerative colitis defined at baseline (week 0) as a Mayo score of 6 to 12, including a Mayo endoscopy subscore ≥ 2. TRUENORTH-I (induction study) In TRUENORTH-I, patients were randomised to either ozanimod 0.92 mg given, orally once daily (n = 429) or placebo (n = 216) beginning with a dose titration (see section 4.2). Patients received concomitant aminosalicylates (e.g., mesalazine 71%; sulfasalazine 13%) and/or oral corticosteroids (33%) at a stable dose prior to and during the induction period. There were 30% of patients who had an inadequate response, loss of response or intolerant to TNF blockers. Of these patients with prior biologic therapy, 63% received at least two or more biologics including TNF blockers; 36% failed to ever respond to at least one TNF blocker; 65% lost response to a TNF blocker; 47% received an integrin receptor blocker (e.g., vedolizumab). There were 41% of patients who failed and/or were intolerant to immunomodulators. At baseline, patients had a median Mayo score of 9, with 65% of patients less than or equal to 9 and 35% having greater than 9. The primary endpoint was clinical remission at week 10, and the key secondary endpoints at week 10 were clinical response, endoscopic improvement, and mucosal healing. A significantly greater proportion of patients treated with ozanimod achieved clinical remission, clinical response, endoscopic improvement, and mucosal healing compared to placebo at week 10 as shown in Table 4. Table 4: Proportion of patients meeting efficacy endpoints in the induction period from TRUENORTH-I (at week 10) Ozanimod 0.92 mg Placebo Treatment (N = 429) (N = 216) Difference %a (95% CI) n % n % 12% Clinical remissionb 79 18% 13 6% (7.5, 17.2)f Without prior TNF blocker 66/299 22% 10/151 7% exposure Prior TNF blocker exposure 13/130 10% 3/65 5% 22% Clinical responsec 205 48% 56 26% (14.4, 29.3)f Without prior TNF blocker 157/299 53% 44/151 29% exposure Prior TNF blocker exposure 48/130 37% 12/65 19% Ozanimod 0.92 mg Placebo Treatment (N = 429) (N = 216) Difference %a (95% CI) n % n % 16% Endoscopic improvementd 117 27% 25 12% (9.7, 21.7)f Without prior TNF blocker 97/299 32% 18/151 12% exposure Prior TNF blocker exposure 20/130 15% 7/65 11% 9% Mucosal healinge 54 13% 8 4% (4.9, 12.9)g Without prior TNF blocker 47/299 16% 6/151 4% exposure Prior TNF blocker exposure 7/130 5% 2/65 3% CI = confidence interval; TNF = tumour necrosis factor. a Treatment difference (adjusted for stratification factors of prior TNF blocker exposure and corticosteroid use at baseline). b Clinical remission is defined as: RBS = 0, SFS ≤ 1 (and a decrease of ≥ 1 point from the baseline SFS), and endoscopy subscore ≤ 1 without friability. c Clinical response is defined as a reduction from baseline in the 9-point Mayo score of ≥ 2 points and ≥ 35%, and a reduction from baseline in the RBS of ≥ 1 or an absolute RBS of ≤ 1 point. d Endoscopic improvement is defined as a Mayo endoscopic score ≤ 1 without friability. e Mucosal healing defined as both Mayo endoscopic score ≤ 1 point without friability and histological remission (Geboes score < 2.0, indicating no neutrophils in the epithelial crypts or lamina propria, no increase in eosinophils, and no crypt destruction, erosions, ulcerations, or granulation tissue) f p < 0.0001. g p < 0.001. Rectal bleeding (RBS) and stool frequency (SFS) subscores Decreases in rectal bleeding and stool frequency subscores were observed as early as week 2 (i.e., 1 week after completing the required 7-day dose titration) in patients treated with ozanimod. A nominally significantly greater proportion of subjects achieved symptomatic remission, defined as RBS = 0, SFS ≤ 1 and a decrease from baseline of ≥ 1, with ozanimod 0.92 mg than with placebo at Week 5 (27% vs 15%) and at Week 10 of the Induction Period (37.5% versus 18.5%). Patients who had a decrease from baseline in SFS and/or RBS of at least 1 point but did not achieve clinical response or clinical remission at week 10 of TRUENORTH-I, had an increased rate of symptomatic remission after an additional 5 weeks of ozanimod treatment, 21% (26/126). The rate of symptomatic remission in these patients continued to increase through an additional 46 weeks of treatment, 50% (41/82). TRUENORTH-M (maintenance study) In order to be randomised to treatment in the maintenance study (TRUENORTH-M), patients had to have received ozanimod 0.92 mg and be in clinical response at week 10 of the induction period. Patients could have come from either TRUENORTH-I or from a group who received ozanimod 0.92 mg open-label. Patients were (re)-randomised in a double-blinded fashion (1:1) to receive either ozanimod 0.92 mg (n = 230) or placebo (n = 227) for 42 weeks. The total study duration was 52 weeks, including both the induction and maintenance periods. Efficacy assessments were at week 52. Concomitant aminosalicylates were required to remain stable through week 52. Patients on concomitant corticosteroids were to taper their dose upon entering the maintenance period. At study entry, 35% of patients were in clinical remission, 29% of patients were on corticosteroids and 31% of patients who were previously treated with TNF blockers. As shown in the Table 5, the primary endpoint was the proportion of patients in clinical remission at week 52. Key secondary endpoints at week 52 were the proportion of patients with clinical response, endoscopic improvement, maintenance of clinical remission at week 52 in the subset of patients in remission at week 10, corticosteroid-free clinical remission, mucosal healing and durable clinical remission. Table 5: Proportion of patients meeting efficacy endpoints in the maintenance period in TRUENORTH-M (at week 52) Ozanimod 0.92 Placebo Treatment mg (N = 227) difference %a (N = 230) (95% CI) n % n % 19% Clinical remissionb 85 37% 42 19% (10.8, 26.4)i Without prior TNF blocker exposure 63/154 41% 35/158 22% Prior TNF blocker exposure 22/76 29% 7/69 10% 19% Clinical responsec 138 60% 93 41% (10.4, 28.0)i Without prior TNF blocker exposure 96/154 62% 76/158 48% Prior TNF blocker exposure 42/76 55% 17/69 25% 19% Endoscopic improvementd 105 46% 60 26% (11.0, 27.7)j Without prior TNF blocker exposure 77/154 50% 48/158 30% Prior TNF blocker exposure 28/76 37% 12/69 17% Maintenance of clinical remission at 24% week 52 in the subset of patients in 41/79 52% 22/75 29% (9.1, 38.6)k remission at week 10e Without prior TNF blocker exposure 37/64 58% 19/58 33% Prior TNF blocker exposure 4/15 27% 3/17 18% Corticosteroid-free clinical 15% 73 32% 38 17% remissionf (7.8, 22.6)j Without prior TNF blocker exposure 55/154 36% 31/158 20% Prior TNF blocker exposure 18/76 24% 7/69 10% 16% Mucosal healingg 68 30% 32 14% (8.2, 22.9)j Without prior TNF blocker exposure 51/154 33% 28/158 18% Prior TNF blocker exposure 17/76 22% 4/69 6% 8% Durable clinical remissionh 41 18% 22 10% (2.8, 13.6)l Without prior TNF blocker exposure 37/154 24% 19/158 12% Prior TNF blocker exposure 4/76 5% 3/69 4% CI = confidence interval; TNF = tumor necrosis factor. a Treatment difference (adjusted for stratification factors of clinical remission and concomitant corticosteroid use at week 10). b Clinical remission is defined as: RBS = 0 point and SFS ≤ 1 point (and a decrease of ≥ 1 point from the baseline SFS) and endoscopy subscore ≤ 1 point without friability. c Clinical response is defined as: A reduction from baseline in the 9-point Mayo score of ≥ 2 points and ≥ 35%, and a reduction from baseline in the RBS of ≥ 1 point or an absolute RBS of ≤ 1 point. d Endoscopic improvement is defined as: Endoscopy subscore of ≤ 1 point without friability. e Maintenance of remission defined as clinical remission at week 52 in the subset of patients in clinical remission at week 10. f Corticosteroid-free remission is defined as clinical remission at week 52 while off corticosteroids for ≥ 12 weeks. g Mucosal healing is defined as both Mayo endoscopic score ≤ 1 without friability and histological remission (Geboes score < 2.0, indicating no neutrophils in the epithelial crypts or lamina propria, no increase in eosinophils, and no crypt destruction, erosions, ulcerations, or granulation tissue) h Durable clinical remission is defined as clinical remission at week 10 and at week 52 in all subjects who entered the maintenance period. i p < 0.0001. j p < 0.001. k p = 0.0025. l p = 0.0030 Steroid free mucosal healing and steroid-free (2-component) symptomatic remission A significantly greater proportion of patients continuously treated with ozanimod 0.92 mg vs re- randomised to placebo achieved corticosteroid-free (at least 12 weeks) symptomatic remission (42.2% ozanimod versus 30.4% placebo) and corticosteroid-free (at least 12 weeks) endoscopic improvement (40.0% ozanimod versus 23.3% placebo) at week 52. Histologic remission at week 10 and 52 Histologic remission (defined as Geboes index score < 2.0 points), was assessed at week 10 of TRUENORTH-I and at week 52 of TRUENORTH-M. At week 10, a significantly greater proportion of patients treated with ozanimod 0.92 mg achieved histologic remission (18%) compared to patients treated with placebo (7%). At week 52, maintenance of this effect was observed with a significantly greater proportion of patients in histologic remission in patients treated with ozanimod 0.92 mg (34%) compared to patients treated with placebo (16%). Long-term data Patients who did not achieve clinical response at the end of the induction period, lost response in the maintenance period or completed the TRUENORTH study were eligible to enter an open label extension study (OLE) and received ozanimod 0.92 mg. Among patients who entered the OLE, clinical remission, clinical response, endoscopic improvement, and symptomatic remission were generally maintained through week 142. No new safety concerns were identified in this study extension in patients with ulcerative colitis (with a mean treatment duration of 22 months).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Ozanimod is extensively metabolised in humans to form a number of circulating active metabolites, including two major active metabolites, CC112273 and CC1084037, with similar activity and selectivity for S1P1 and S1P5 to the parent. The maximum plasma concentration (Cmax) and area under the curve (AUC) for ozanimod, CC112273, and CC1084037 increased proportionally over the dose range of ozanimod 0.46 mg to 0.92 mg (0.5 to 1 times the recommended dose). Following multiple dosing, approximately 94% of circulating total active substances are represented by ozanimod (6%), CC112273 (73%), and CC1084037 (15%). At a dose of 0.92 mg orally once daily in RRMS, the geometric mean [coefficient of variation (CV%)] Cmax and AUC0-24h at steady state were 231.6 pg/mL (37.2%) and 4223 pg*h/mL (37.7%), respectively, for ozanimod and 6378 pg/mL (48.4%) and 132861 pg*h/mL (45.6%), respectively, for CC112273. Cmax and AUC0-24h for CC1084037 are approximately 20% of that for CC112273. Factors affecting CC112273 are applicable for CC1084037 as they are interconverting metabolites. Population pharmacokinetic analysis indicated that there were no meaningful differences in these pharmacokinetic parameters in patients with relapsing MS or UC. Absorption The Tmax of ozanimod is approximately 6–8 hours. The Tmax of CC112273 is approximately 10 hours. Administration of ozanimod with a high-fat, high-calorie meal had no effect on ozanimod exposure (Cmax and AUC). Therefore, ozanimod may be taken without regard to meals. Distribution The mean (CV%) apparent volume of distribution of ozanimod (Vz/F) was 5590 L (27%), indicating extensive tissue distribution. Binding of ozanimod to human plasma proteins is approximately 98.2%. Binding of CC112273 and CC1084037 to human plasma proteins is approximately 99.8% and 99.3%, respectively. Biotransformation Ozanimod is widely metabolised by multiple biotransformation pathways including aldehyde dehydrogenase and alcohol dehydrogenase (ALDH/ADH), cytochrome P450 (CYP) isoforms 3A4 and 1A1, and gut microflora and no single enzyme system predominates the overall metabolism. Following repeated dosing, the AUCs of the two major active metabolites CC112273 and CC1084037 exceed the AUC of ozanimod by 13-fold and 2.5-fold, respectively. In vitro studies indicated that monoamine oxidase B (MAO-B) is responsible for the formation of CC112273 (via an intermediate minor active metabolite RP101075) while CYP2C8 and oxido-reductases are involved in the metabolism of CC112273. CC1084037 is formed directly from CC112273 and undergoes reversible metabolism to CC112273. The interconversion between these 2 active metabolites is mediated by carbonyl reductases (CBR), aldo-keto reductase (AKR) 1C1/1C2, and/or 3β- and 11β- hydroxysteroid dehydrogenase (HSD). Elimination The mean (CV%) apparent oral clearance for ozanimod was approximately 192 L/h (37%). The mean (CV%) plasma half-life (t1/2) of ozanimod was approximately 21 hours (15%). Steady state for ozanimod was achieved within 7 days, with the estimated accumulation ratio following repeated oral administration of 0.92 mg once daily of approximately 2. The model-based mean (CV%) effective half-life (t1/2) of CC112273 was approximately 11 days (104%) in RMS patients, with mean (CV%) time to steady state of approximately 45 days (45%) and accumulation ratio of approximately 16 (101%) indicating the predominance of CC112273 over ozanimod. Plasma levels of CC112273 and its direct, interconverting metabolite CC1084037 declined in parallel in the terminal phase, yielding similar t1/2 for both metabolites. Steady state attainment and accumulation ratio for CC1084037 are expected to be similar to CC112273. Following a single oral 0.92 mg dose of [14C]-ozanimod, approximately 26% and 37% of the radioactivity was recovered from urine and faeces, respectively, primarily composed of inactive metabolites. Ozanimod, CC112273, and CC1084037 concentrations in urine were negligible, indicating that renal clearance is not an important excretion pathway for ozanimod, CC112273, and CC1084037. Pharmacokinetics in specific groups of patients Renal impairment In a dedicated renal impairment trial, following a single oral dose of 0.23 mg ozanimod, exposures (AUClast) for ozanimod and CC112273 were approximately 27% higher and 23% lower, respectively, in patients with end stage renal disease (N = 8) compared to patients with normal renal function (n = 8). Based on this trial, renal impairment had no clinically important effects on pharmacokinetics of ozanimod or CC112273. No dose adjustment is needed in patients with renal impairment. Hepatic impairment In single dose and multiple dose studies in subjects with chronic liver disease, there was no meaningful impact of mild or moderate chronic hepatic impairment (Child-Pugh class A or B) on the pharmacokinetics of ozanimod or the major metabolite CC112273 on Day 1, Day 5, or Day 8 of dosing. After dose escalation in the second trial, administration of 0.92 mg ozanimod resulted in increased CC112273 and CC1084037 mean unbound AUC0-last (measured up to 64 days post-dose) in subjects with mild or moderate chronic hepatic impairment of 99.64% to 129.74% relative to healthy control subjects. Patients with mild or moderate chronic hepatic impairment (Child-Pugh class A or B) are recommended to complete the 7-day dose escalation regimen, and then take 0.92 mg once every other day (see section 4.2). The pharmacokinetics of ozanimod were not evaluated in patients with severe hepatic impairment. Use in patients with severe hepatic impairment is contraindicated (Child-Pugh class C) (see section 4.3). Elderly Population pharmacokinetic analysis showed that steady state exposure (AUC) of CC112273 in patients over 65 years of age were approximately 3 - 4% greater than patients 45 – 65 years of age and 27% greater than adult patients under 45 years of age. There is not a meaningful difference in the pharmacokinetics in elderly patients. Paediatric population Zeposia is not indicated for children and adolescents under 18 years old. No data are available on administration of ozanimod to paediatric or adolescent patients (< 18 years of age).

פרטי מסגרת הכללה בסל
התרופה האמורה תינתן לטיפול במקרים האלה:א. כמונותרפיה לטיפול בחולים עם אבחנה וודאית של טרשת נפוצה (על פי הקריטריונים העדכניים על שם McDonald) עם מחלה פעילה או Clinically isolated syndrome (CIS), בהתאם לתנאי הרישום. הטיפול לא יינתן לחולים עם מחלה פרוגרסיבית ראשונית (PPMS) או פרוגרסיבית שניונית פעילה (SPMS) שאינם מטופלים בתרופות ייעודיות לטרשת נפוצה.התחלת הטיפול בתרופה תיעשה לפי מרשם של נוירו אימונולוג שעבר השתלמות עמיתים, או נוירולוג ילדים שעבר השתלמות עמיתים בטרשת נפוצה, או מומחה בנוירולוגיה העובד במרפאת טרשת נפוצה או מרפאה נוירואימונולוגית ייעודית.ב. מחלת מעי דלקתית מסוג Ulcerative colitis בחולים שמיצו טיפול קודם – טיפול לא ביולוגי או טיפול ביולוגי.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2021
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
167 35 36601 99
מחיר
0 ₪
מידע נוסף
עלון מידע לצרכן
14.02.22 - עלון לצרכן אנגלית 14.02.22 - עלון לצרכן עברית 14.02.22 - עלון לצרכן ערבית 14.02.22 - עלון לצרכן 12.07.21 - עלון לצרכן אנגלית 12.07.21 - עלון לצרכן עברית 12.07.21 - עלון לצרכן ערבית 02.09.21 - עלון לצרכן 09.03.22 - עלון לצרכן אנגלית 09.03.22 - עלון לצרכן עברית 09.03.22 - עלון לצרכן ערבית 12.07.21 - עלון לצרכן אנגלית 28.12.23 - עלון לצרכן עברית 17.01.24 - עלון לצרכן עברית 19.01.24 - עלון לצרכן אנגלית 19.01.24 - עלון לצרכן עברית 19.01.24 - עלון לצרכן ערבית 31.03.24 - עלון לצרכן אנגלית 31.03.24 - עלון לצרכן עברית 31.03.24 - עלון לצרכן ערבית 31.03.24 - עלון לצרכן 31.03.24 - עלון לצרכן 03.05.24 - עלון לצרכן עברית 21.06.24 - עלון לצרכן עברית 25.06.24 - עלון לצרכן אנגלית 25.06.24 - עלון לצרכן עברית 25.06.24 - עלון לצרכן ערבית 22.07.24 - עלון לצרכן אנגלית 22.07.24 - עלון לצרכן עברית 22.07.24 - עלון לצרכן ערבית 22.07.24 - עלון לצרכן 25.07.24 - עלון לצרכן עברית 10.08.24 - עלון לצרכן אנגלית 10.08.24 - עלון לצרכן עברית 10.08.24 - עלון לצרכן ערבית 04.01.22 - החמרה לעלון 09.03.22 - החמרה לעלון 28.12.23 - החמרה לעלון 03.05.24 - החמרה לעלון 25.07.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
זפוסיה 0.92 מ"ג