Quest for the right Drug
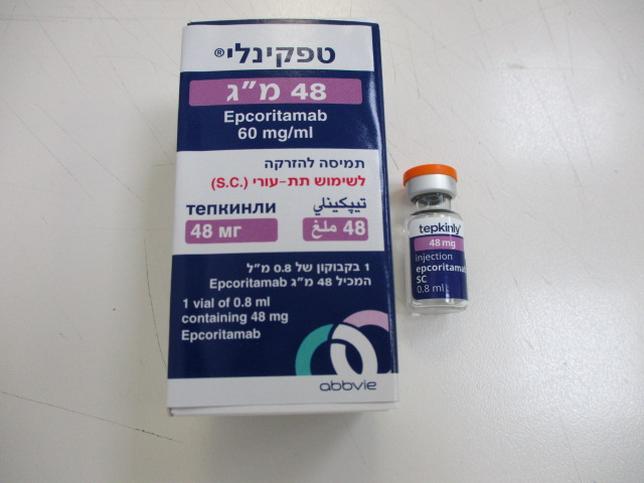
טפקינלי 48 מ"ג TEPKINLY 48MG (EPCORITAMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Posology : מינונים
4.2 Posology and method of administration Tepkinly must only be administered under the supervision of a healthcare professional qualified in the use of anti-cancer therapy. At least 1 dose of tocilizumab for use in the event of CRS should be available prior to epcoritamab administration for Cycle 1. Access to an additional dose of tocilizumab within 8 hours of use of the previous tocilizumab dose should be available. Posology Recommended pre-medication and dose schedule Tepkinly should be administered according to the following dosing schedule in 28-day cycles which is outlined in Table 1. Table 1 Dosing schedule Dosing schedule Cycle of Days Epcoritamab dose (mg)a treatment Weekly Cycle 1 1 0.16 mg (Step-up dose 1) 8 0.8 mg (Step-up dose 2) 15 48 mg (First full dose) 22 48 mg Weekly Cycles 2 - 3 1, 8, 15, 22 48 mg Every two weeks Cycles 4 - 9 1, 15 48 mg Every four weeks Cycles 10 + 1 48 mg a 0.16 mg is a priming dose, 0.8 mg is an intermediate dose and 48 mg is a full dose. Tepkinly should be administered until disease progression or unacceptable toxicity. Details on recommended pre-medication for cytokine release syndrome (CRS) are shown in Table 2. Table 2 Epcoritamab pre-medication Cycle Patient requiring pre- Pre-medication Administration medication Cycle 1 All patients Prednisolone (100 mg oral or • 30-120 minutes prior to intravenous) or dexamethasone each weekly (15 mg oral or intravenous) or administration of equivalent epcoritamab • And for three consecutive days following each weekly administration of epcoritamab in Cycle 1 • Diphenhydramine • 30-120 minutes prior to (50 mg oral or each weekly intravenous) or administration of equivalent epcoritamab • Paracetamol (650 to 1,000 mg oral) Cycle 2 and Patients who Prednisolone (100 mg oral or • 30-120 minutes prior to beyond experienced Grade 2 or intravenous) or next administration of 3a CRS with previous dexamethasone (15 mg oral epcoritamab after a grade dose or intravenous) or 2 or 3a CRS event equivalent • And for three consecutive days following the next administration of epcoritamab until epcoritamab is given without subsequent CRS of Grade 2 or higher a Patients will be permanently discontinued from epcoritamab after a Grade 4 CRS event. Prophylaxis against Pneumocystis jirovecii pneumonia (PCP) and herpes virus infections is strongly recommended especially during concurrent use of steroids. Tepkinly should be administered to adequately hydrated patients. Patients at an increased risk for clinical tumour lysis syndrome (CTLS) are recommended to receive hydration and prophylactic treatment with a uric acid lowering agent. Patients should be monitored for signs and symptoms of CRS and/or immune effector cell-associated neurotoxicity syndrome (ICANS) following epcoritamab administration. Patients should be hospitalised for 24 hours after administration of the Cycle 1 Day 15 dose of 48 mg to monitor for signs and symptoms of CRS and/or ICANS. Patients should be counselled on the signs and symptoms associated with CRS and ICANS and on seeking immediate medical attention should signs or symptoms occur at any time (see section 4.4). Dose modifications and management of adverse reactions Cytokine release syndrome (CRS) Patients treated with epcoritamab may develop CRS. Evaluate for and treat other causes of fever, hypoxia, and hypotension. If CRS is suspected, manage according to the recommendations in Table 3. Patients who experience CRS should be monitored more frequently during next scheduled epcoritamab administration. Table 3 CRS grading and management guidance Gradea Recommended therapy Epcoritamab dose modification Grade 1 Provide supportive care such as Hold epcoritamab until resolution • Fever (temperature ≥ 38 °C) antipyretics and of CRS event intravenous hydration Dexamethasoneb may be initiated In cases of advanced age, high tumour burden, circulating tumour cells, fever refractory to antipyretics • Anti-cytokine therapy, tocilizumabd, should be considered For CRS with concurrent ICANS refer to Table 4 Grade 2 Provide supportive care such as Hold epcoritamab until resolution • Fever (temperature ≥ 38 °C) antipyretics and of CRS event intravenous hydration and Dexamethasoneb should be considered • Hypotension not requiring vasopressors Anti-cytokine therapy, tocilizumabd, is recommended and/or If CRS is refractory to dexamethasone and • Hypoxia requiring low-flow tocilizumab: oxygene by nasal cannula or blow- • Alternative by immunosuppressantsg and methylprednisolone 1,000 mg/day intravenously should be administered until clinical improvement For CRS with concurrent ICANS refer to Table 4 Grade 3 Provide supportive care such as Hold epcoritamab until resolution • Fever (temperature ≥ 38 °C) antipyretics and of CRS event intravenous hydration and In the event of Grade 3 CRS Dexamethasonec should be administered lasting longer than 72 hours, • Hypotension requiring a epcoritamab should be vasopressor with or without Anti-cytokine therapy, discontinued vasopressin tocilizumabd, is recommended If more than 2 separate events of and/or If CRS is refractory to dexamethasone and Grade 3 CRS, even if each event tocilizumab: resolved to Grade 2 within Gradea Recommended therapy Epcoritamab dose modification • Hypoxia requiring high-flow • Alternative 72 hours, epcoritamab should be oxygenf by nasal cannula, immunosuppressantsg and discontinued facemask, non-rebreather mask, methylprednisolone or venturi mask 1,000 mg/day intravenously should be administered until clinical improvement For CRS with concurrent ICANS refer to Table 4 Grade 4 Provide supportive care such as Permanently discontinue • Fever (temperature ≥ 38 °C) antipyretics and epcoritamab intravenous hydration and Dexamethasonec should be administered • Hypotension requiring ≥ 2 vasopressors (excluding Anti-cytokine therapy, vasopressin) tocilizumabd, is recommended and/or If CRS is refractory to dexamethasone and tocilizumab: • Hypoxia requiring positive • Alternative pressure ventilation (e.g., CPAP, immunosuppressantsg and BiPAP, intubation and mechanical methylprednisolone ventilation) 1,000 mg/day intravenously should be administered until clinical improvement For CRS with concurrent ICANS refer to Table 4 a CRS graded according to ASTCT consensus criteria b Dexamethasone should be administered at 10-20 mg per day (or equivalent) c Dexamethasone should be administered at 10-20 mg intravenously every 6 hours d Tocilizumab 8 mg/kg intravenously over 1 hour (not to exceed 800 mg per dose). Repeat tocilizumab after at least 8 hours as needed. Maximum of 2 doses in a 24-hour period e Low-flow oxygen is defined as oxygen delivered at < 6 L/minute f High-flow oxygen is defined as oxygen delivered at ≥ 6 L/minute g Riegler L et al. (2019) Immune effector cell-associated neurotoxicity syndrome (ICANS) Patients should be monitored for signs and symptoms of ICANS. Other causes of neurologic symptoms should be ruled out. If ICANS is suspected, manage according to the recommendations in Table 4. Table 4 ICANS grading and management guidance Gradea Recommended therapy Epcoritamab dose modification Grade 1b Treatment with dexamethasoned Hold epcoritamab ICE scorec 7-9 b until resolution of or, depressed level of Consider non-sedating anti-seizure medicinal products (e.g., event consciousnessb: awakens levetiracetam) until resolution of ICANS spontaneously No concurrent CRS: • Anti-cytokine therapy not recommended For ICANS with concurrent CRS: • Treatment with dexamethasoned • Choose immunosuppressant alternativese to tocilizumab, if possible Grade 2b Treatment with dexamethasonef Hold epcoritamab ICE scorec 3-6 until resolution of or, depressed level of Consider non-sedating anti-seizure medicinal products (e.g., event consciousnessb: awakens levetiracetam) until resolution of ICANS to voice No concurrent CRS: • Anti-cytokine therapy not recommended For ICANS with concurrent CRS: • Treatment with dexamethasoned • Choose immunosuppressant alternativese to tocilizumab, if possible Grade 3b Treatment with dexamethasoneg Permanently ICE scorec 0-2 • If no response, initiate methylprednisolone discontinue or, depressed level of 1,000 mg/day epcoritamab consciousnessb: awakens only to tactile stimulus, Consider non-sedating anti-seizure medicinal products (e.g., or levetiracetam) until resolution of ICANS seizuresb, either: No concurrent CRS: • any clinical seizure, focal or • Anti-cytokine therapy not recommended generalised that resolves rapidly, or For ICANS with concurrent CRS: • non-convulsive seizures on • Treatment with dexamethasone electroencephalogram (EEG) that resolve with intervention, or o If no response, initiate raised intracranial methylprednisolone 1,000 mg/day pressure: focal/local • Choose immunosuppressant alternativese to oedemab on tocilizumab, if possible neuroimagingc Gradea Recommended therapy Epcoritamab dose modification Grade 4b Treatment with dexamethasoneg Permanently ICE scorec, b 0 • If no response, initiate methylprednisolone discontinue 1,000 mg/day epcoritamab or, depressed level of consciousnessb either: Consider non-sedating anti-seizure medicinal products (e.g., • patient is unarousable or requires vigorous or repetitive levetiracetam) until resolution of ICANS tactile stimuli to arouse, or • stupor or coma, or No concurrent CRS: • Anti-cytokine therapy not recommended b seizures , either: • life-threatening prolonged For ICANS with concurrent CRS: seizure (> 5 minutes), or • Treatment with dexamethasone • repetitive clinical or electrical o If no response, initiate methylprednisolone 1,000 mg/day seizures without return to • Choose immunosuppressant alternativese to baseline in between, tocilizumab, if possible or motor findingsb: • deep focal motor weakness such as hemiparesis or paraparesis, or raised intracranial pressure / cerebral oedemab, with signs/symptoms such as: • diffuse cerebral oedema on neuroimaging, or • decerebrate or decorticate posturing, or • cranial nerve VI palsy, or • papilloedema, or • cushing’s triad a ICANS graded according to ASTCT ICANS Consensus Grading b ICANS grade is determined by the most severe event (ICE score, level of consciousness, seizures, motor findings, raised ICP/cerebral oedema) not attributable to any other cause c If patient is arousable and able to perform Immune Effector Cell-Associated Encephalopathy (ICE) Assessment, assess: Orientation (oriented to year, month, city, hospital = 4 points); Naming (name 3 objects, e.g., point to clock, pen, button = 3 points); Following Commands (e.g., “show me 2 fingers” or “close your eyes and stick out your tongue” = 1 point); Writing (ability to write a standard sentence = 1 point); and Attention (count backwards from 100 by ten = 1 point). If patient is unarousable and unable to perform ICE Assessment (Grade 4 ICANS) = 0 points. d Dexamethasone should be administered at 10 mg intravenously every 12 hours e Riegler L et al. (2019) f Dexamethasone 10-20 mg intravenously every 12 hours g Dexamethasone 10-20 mg intravenously every 6 hours Table 5 Recommended dose modifications for other adverse reactions Adverse Reaction1 Severity1 Action Infections (see section 4.4) Grades 1-4 • Withhold epcoritamab in patients with active infection, until the infection resolves • For Grade 4, consider permanent discontinuation of Tepkinly Neutropenia or febrile Absolute neutrophil count • Withhold epcoritamab until neutropenia (see section 4.8) less than 0.5 x 109/L absolute neutrophil count is 0.5 x 109/L or higher Thrombocytopenia (see section Platelet count • Withhold epcoritamab until 9 4.8) less than 50 x 10 /L platelet count is 50 x 109/L or higher Other adverse reactions (see Grade 3 or higher • Withhold epcoritamab until the section 4.8) toxicity resolves to Grade 1 or baseline 1 Based on National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE), Version 5.0. Missed or delayed dose A re-priming Cycle (identical to Cycle 1 with standard CRS prophylaxis) is required: • If there are more than 8 days between the priming dose (0.16 mg) and intermediate dose (0.8 mg), or • If there are more than 14 days between the intermediate dose (0.8 mg) and first full dose (48 mg), or • If there are more than 6 weeks between full doses (48 mg) After the re-priming cycle, the patient should resume treatment with Day 1 of the next planned treatment cycle (subsequent to the cycle during which the dose was delayed). Special populations Renal impairment Dose adjustments are not considered necessary in patients with mild to moderate renal impairment. Epcoritamab has not been studied in patients with severe renal impairment to end stage renal disease. No dose recommendations can be made for patients with severe renal impairment to end-stage renal disease (see section 5.2). Hepatic impairment Dose adjustments are not considered necessary in patients with mild hepatic impairment. Epcoritamab has not been studied in patients with severe hepatic impairment (defined as total bilirubin > 3 times ULN and any AST) and data are limited in patients with moderate hepatic impairment (defined as total bilirubin > 1.5 to 3 times ULN and any AST). No dose recommendations can be made for patients with moderate to severe hepatic impairment (see section 5.2). Elderly No dose adjustment is necessary in patients ≥ 65 years of age (see sections 5.1 and 5.2). Paediatric population The safety and efficacy of Tepkinly in children aged less than 18 years of age have not yet been established. No data are available. Method of administration Tepkinly is for subcutaneous use. It should be administered by subcutaneous injection only, preferably in the lower part of the abdomen or the thigh. Change of injection site from left to right side or vice versa is recommended especially during the weekly administration schedule (i.e., Cycles 1-3). For instructions on dilution or preparation of the medicinal product before administration, see section 6.6.

פרטי מסגרת הכללה בסל
א. התרופה תינתן כמונותרפיה למבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. ב. במהלך מחלתו יהיה חולה זכאי לטיפול באחד מהבאים – Epcoritamab, Glofitamab ג. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או רופא מומחה בהמטולוגיה.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
17/03/2024
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
יצרן
ABBVIE S.R.L., ITALYבעל רישום
ABBVIE BIOPHARMACEUTICALS LTD, ISRAELרישום
176 08 37756 00
מחיר
0 ₪
מידע נוסף
