Quest for the right Drug
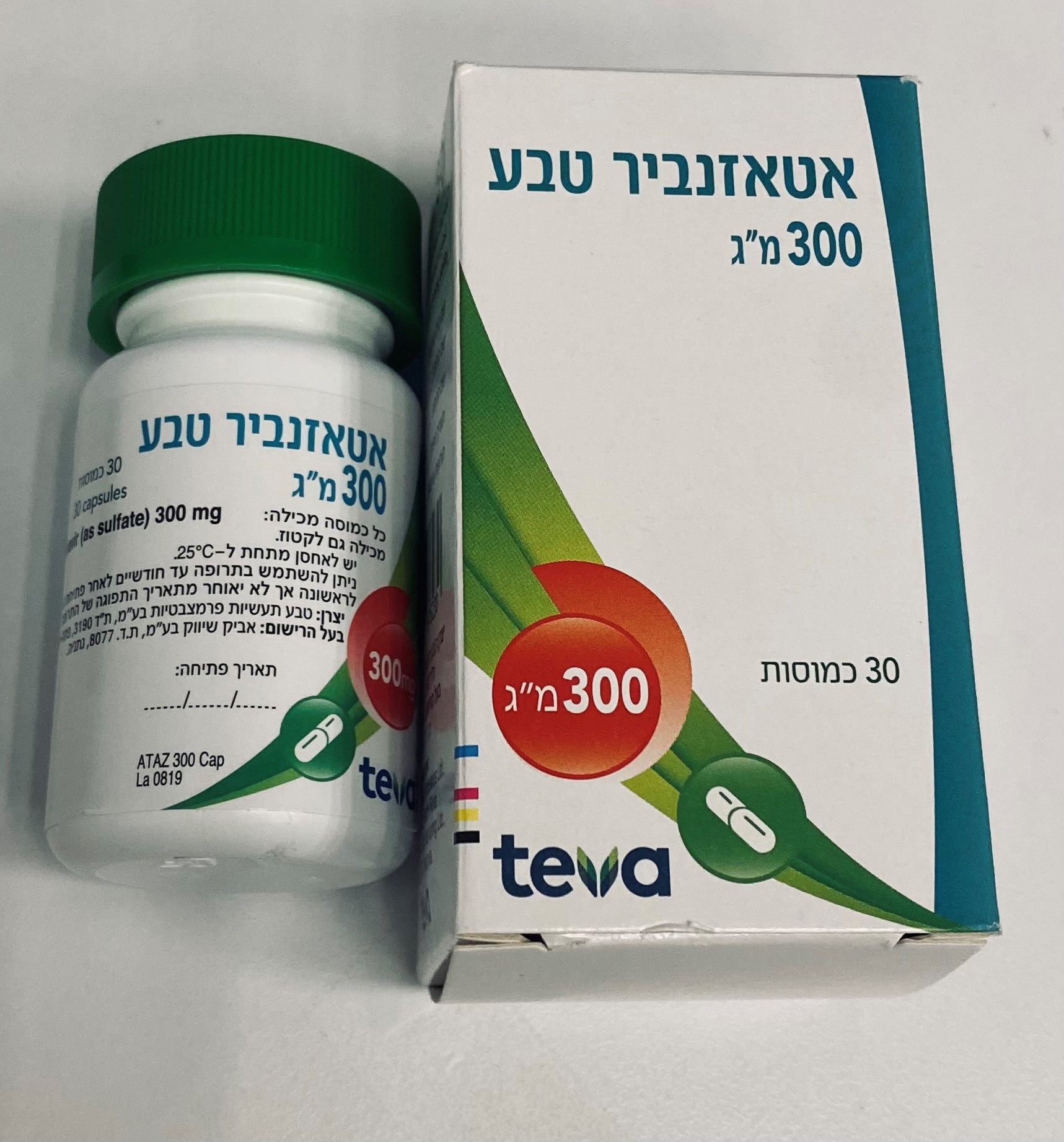
אטאזנביר טבע ® 300 מ"ג ATAZANAVIR TEVA ® 300 MG (ATAZANAVIR AS SULFATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות : CAPSULES
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
11.2. Pharmacodynamics Cardiac Electrophysiology Concentration- and dose-dependent prolongation of the PR interval in the electrocardiogram has been observed in healthy subjects receiving atazanavir. In a placebo-controlled study AI424-076, the mean (±SD) maximum change in PR interval from the predose value was 24 (±15) msec following oral dosing with 400 mg of atazanavir (n=65) compared to (±11) msec following dosing with placebo (n=67). The PR interval prolongations in this study were asymptomatic. There is limited information on the potential for a pharmacodynamic interaction in humans between atazanavir and other drugs that prolong the PR interval of the electrocardiogram [see Warnings and Precautions (5.1)]. Electrocardiographic effects of atazanavir were determined in a clinical pharmacology study of 72 healthy subjects. Oral doses of 400 mg (maximum recommended dosage) and 800 mg (twice the maximum recommended dosage) were compared with placebo; there was no concentrationdependent effect of atazanavir on the QTc interval (using Fridericia's correction). In 1793 subjects with HIV-1 infection receiving antiretroviral regimens, QTc prolongation was comparable in the atazanavir and comparator regimens. No atazanavir-treated healthy subject or subjects with HIV-1 infection in clinical trials had a QTc interval >500 msec [see Warnings and Precautions (5.1)].
Pharmacokinetic Properties
11.3. Pharmacokinetics The pharmacokinetics of atazanavir were evaluated in healthy adult subjects who either were healthy, or with HIV infection,, after administration of atazanavir 400 mg once daily and after administration of atazanavir 300 mg with ritonavir 100 mg once daily (see Table 17). Table 17: Steady-State Pharmacokinetics of atazanavir in Healthy Subjects or Subjects with HIV-1 Infection in the Fed State 300 mg with ritonavir 400 mg once daily 100 mg once daily Subjects with Healthy Subjects Subjects with HIV- Healthy Subjects HIV-1 Infection Parameter (n=14) 1 Infection (n=13) (n=28) (n=10) Cmax (ng/mL) Geometric mean (CV%) 5199 (26) 2298 (71) 6129 (31) 4422 (58) Mean (SD) 5358 (1371) 3152 (2231) 6450 (2031) 5233 (3033) Tmax (h) Median 2.5 2.0 2.7 3.0 AUC (ng*h/mL) Geometric mean (CV%) 28132 (28) 14874 (91) 57039 (37) 46073 (66) Mean (SD) 29303 (8263) 22262 (20159) 61435 (22911) 53761 (35294) T-half (h) Mean (SD) 7.9 (2.9) 6.5 (2.6) 18.1 (6.2)a 8.6 (2.3) Cmin (ng/mL) Geometric mean (CV%) 159 (88) 120 (109) 1227 (53) 636 (97) Mean (SD) 218 (191) 273 (298)b 1441 (757) 862 (838) a. n=26 b. n=12 Figure1 displays the mean plasma concentrations of atazanavir at steady state after atazanavir 400 mg once daily (as two 200-mg capsules) with a light meal and after atazanavir 300 mg (as two 150-mg capsules) with ritonavir 100 mg once daily with a light meal in adult subjects with HIV-1 infection. Figure 1 : Mean (SD) Steady-State Plasma Concentrations of Atazanavir 400 mg (n=13) and 300 mg with Ritonavir (n=10) for HIV-Infected Adult subjects with HIV-1 Infection Absorption Atazanavir is rapidly absorbed with a Tmax of approximately 2.5 hours. Atazanavir demonstrates nonlinear pharmacokinetics with greater than dose-proportional increases in AUC and Cmax values over the dose range of 200 to 800 mg once daily. Steady state is achieved between Days 4 and 8, with an accumulation of approximately 2.3 fold. Food Effect Administration of atazanavir with food enhances bioavailability and reduces pharmacokinetic variability. Administration of a single 400-mg dose of atazanavir with a light meal (357 kcal, 8.2 g fat, 10.6 g protein) resulted in a 70% increase in AUC and 57% increase in Cmax relative to the fasting state. Administration of a single 400-mg dose of atazanavir with a high-fat meal (721 kcal, 37.3 g fat, 29.4 g protein) resulted in a mean increase in AUC of 35% with no change in Cmax relative to the fasting state. Administration of atazanavir with either a light meal or high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately one-half compared to the fasting state. Coadministration of a single 300-mg dose of atazanavir and a 100-mg dose of ritonavir with a light meal (336 kcal, 5.1 g fat, 9.3 g protein) resulted in a 33% increase in the AUC and a 40% increase in both the Cmax and the 24-hour concentration of atazanavir relative to the fasting state. Coadministration with a high-fat meal (951 kcal, 54.7 g fat, 35.9 g protein) did not affect the AUC of atazanavir relative to fasting conditions and the Cmax was within 11% of fasting values. The 24-hour concentration following a high- fat meal was increased by approximately 33% due to delayed absorption; the median Tmax increased from 2.0 to 5.0 hours. Coadministration of Atazanavir with ritonavir with either a light or a high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately 25% compared to the fasting state. Distribution Atazanavir is 86% bound to human serum proteins and protein binding is independent of concentration. Atazanavir binds to both alpha-1-acid glycoprotein (AAG) and albumin to a similar extent (89% and 86%, respectively). In a multiple-dose study in subjects with HIV-1 infection dosed with atazanavir 400 mg once daily with a light meal for 12 weeks, atazanavir was detected in the cerebrospinal fluid and semen. The cerebrospinal fluid/plasma ratio for atazanavir (n=4) ranged between 0.0021 and 0.0226 and seminal fluid/plasma ratio (n=5) ranged between 0.11 and 4.42. Metabolism Atazanavir is extensively metabolized in humans. The major biotransformation pathways of atazanavir in humans consisted of monooxygenation and dioxygenation. Other minor biotransformation pathways for atazanavir or its metabolites consisted of glucuronidation, N-dealkylation, hydrolysis, and oxygenation with dehydrogenation. Two minor metabolites of atazanavir in plasma have been characterized. Neither metabolite demonstrated in vitro antiviral activity. In vitro studies using human liver microsomes suggested that atazanavir is metabolized by CYP3A. Elimination Following a single 400-mg dose of 14C-atazanavir, 79% and 13% of the total radioactivity was recovered in the feces and urine, respectively. Unchanged drug accounted for approximately 20% and 7% of the administered dose in the feces and urine, respectively. The mean elimination half-life of atazanavir in healthy subjects (n=214) and adult subjects with HIV-1 infection (n=13) was approximately 7 hours at steady state following a dose of 400 mg daily with a light meal. Specific Populations Renal Impairment In healthy subjects, the renal elimination of unchanged atazanavir was approximately 7% of the administered dose. Atazanavir has been studied in adult subjects with severe renal impairment (n=20), including those on hemodialysis, at multiple doses of 400 mg once daily. The mean atazanavir Cmax was 9% lower, AUC was 19% higher, and Cmin was 96% higher in subjects with severe renal impairment not undergoing hemodialysis (n=10), than in age-, weight-, and gender-matched subjects with normal renal function. In a 4-hour dialysis session, 2.1% of the administered dose was removed. When atazanavir was administered either prior to, or following hemodialysis (n=10), the geometric means for Cmax, AUC, and Cmin were approximately 25% to 43% lower compared to subjects with normal renal function. The mechanism of this decrease is unknown. Atazanavir is not recommended for use in treatment-experienced patients with HIV-1 who have end stage renal disease managed with hemodialysis [see Dosage and Administration (2.7)]. Hepatic Impairment Atazanavir has been studied in adult subjects with moderate-to-severe hepatic impairment (14 Child-Pugh B and 2 Child-Pugh C subjects) after a single 400-mg dose. The mean ALC,(0-∞) was 42% greater in subjects with impaired hepatic function than in healthy subjects. The mean half-life of atazanavir in hepatically impaired subjects was 12.1 hours compared to 6.4 hours in healthy subjects. A dose reduction to 300 mg is recommended for patients with moderate hepatic impairment (Child-Pugh Class B) who have not experienced prior virologic failure as increased concentrations of atazanavir are expected. atazanavir is not recommended for use in patients with severe hepatic impairment. The pharmacokinetics of atazanavir in combination with ritonavir has not been studied in subjects with hepatic impairment; thus, coadministration of atazanavir with ritonavir is not recommended for use in patients with any degree of hepatic impairment [see Dosage and Administration (2.8)]. Pediatrics The pharmacokinetic parameters for atazanavir at steady state in pediatric subjects taking the cspsule formulation were predicted by a population pharmacokinetic model and are summarized in Table 18 by weight ranges that correspond to the recommended doses [see Dosage and Administration (2.4).] Table 18: Predicted Steady-State Pharmacokinetics of Atazanavir (capsule formulation) with Ritonavir in Pediatric Subjects with HIV-1 Infection Cmax ng/mL AUC ng*h/mL Cmin ng/mL Body Weight atazanavir/ritonavir Geometric Mean Geometric Mean Geometric Mean (range in kg) Dose (mg) (CV%) (CV%) (CV%) 15 to <35 200/100 3303 (86%) 37235 (84%) 538 (99%) ≥35 300/100 2980 (82%) 37643 (83%) 653 (89%) Pregnancy The pharmacokinetic data from pregnant women with HIV-1 infection receiving atazanavir Capsules with ritonavir are presented in Table 19. Table 19: Steady-State Pharmacokinetics of Atazanavir with Ritonavir in Pregnant Women with HIV-1 Infection in the Fed State Pharmacokinetic Parameter Atazanavir 300 mg with ritonavir 100 mg 2nd Trimester 3rd Trimester Postpartumb (n=5a) (n=20) (n=34) Cmax ng/mL 3078.85 3291.46 5721.21 Geometric mean (CV%) (50) (48) (31) AUC ng*h/mL 27657.1 34251.5 61990.4 Geometric mean (CV%) (43) (43) (32) Cmin ng/mLc 538.70 668.48 1462.59 Geometric mean (CV%) (46) (50) (45) a. Available data during the 2nd trimester are limited. b. Atazanavir peak concentrations and AUCs were found to be approximately 28% to 43% higher during the postpartum period (4-12 weeks) than those observed historically in non-pregnant patients with HIV-1 infection. Atazanavir plasma trough concentrations were approximately 2.2- fold higher during the postpartum period when compared to those observed historically in non- pregnant patients with HIV-1 infection. c. Cmin is concentration 24 hours post-dose. Drug Interaction Data Atazanavir is a metabolism-dependent CYP3A inhibitor, with a Kinact value of 0.05 to 0.06 min-1 and Ki value of 0.84 to 1.0 µM. Atazanavir is also a direct inhibitor for UGT1A1 (Ki=1.9 µM) and CYP2C8 (Ki=2.1 µM). Atazanavir has been shown in vivo not to induce its own metabolism nor to increase the biotransformation of some drugs metabolized by CYP3A. In a multiple-dose study, atazanavir decreased the urinary ratio of endogenous 6β-OH cortisol to cortisol versus baseline, indicating that CYP3A production was not induced. Clinically significant interactions are not expected between atazanavir and substrates of CYP2C19, CYP2C9, CYP2D6, CYP2B6, CYP2A6, CYP1A2, or CYP2E1. Clinically significant interactions are not expected between atazanavir when administered with ritonavir and substrates of CYP2C8. See the complete prescribing information for ritonavir for information on other potential drug interactions with ritonavir. Based on known metabolic profiles, clinically significant drug interactions are not expected between Atazanavir Teva and dapsone, trimethoprim/sulfamethoxazole, azithromycin, or erythromycin. Atazanavir Teva does not interact with substrates of CYP2D6 (eg, nortriptyline, desipramine, metoprolol). Drug interaction studies were performed with atazanavir and other drugs likely to be coadministered and some drugs commonly used as probes for pharmacokinetic interactions. The effects of coadministration of atazanavir on the AUC, Cmax, and Cmin are summarized in Tables 20 and 21. Neither didanosine EC nor diltiazem had a significant effect on atazanavir exposures (see Table 21 for effect of atazanavir on didanosine EC or diltiazem exposures). Atazanavir did not have a significant effect on the exposures of didanosine (when administered as the buffered tablet), stavudine, or fluconazole. For information regarding clinical recommendations, see Drug Interactions (7). Table 20: Drug Interactions: Pharmacokinetic Parameters for Atazanavir in the Presence of Coadministered Drugsa Coadministe Coadministered Atazanavir Ratio (90% Confidence Interval) of red Drug Drug Dose/Schedule Dose/Schedule Atazanavir Pharmacokinetic Parameters with/without Coadministered Drug; No Effect = 1.00 Cmax AUC Cmin atenolol 50 mg QD, d 7-11 400 mg QD, d 1-11 1.00 0.93 0.74 (n=19) and d 19-23 (n=19) (0.89, 1.12) (0.85, 1.01) (0.65, 0.86) Coadministe Coadministered Atazanavir Ratio (90% Confidence Interval) of red Drug Drug Dose/Schedule Dose/Schedule Atazanavir Pharmacokinetic Parameters with/without Coadministered Drug; No Effect = 1.00 Cmax AUC Cmin clarithromycin 500 mg BID, d 7-10 400 mg QD, d 1-10 1.06 1.28 1.91 (n=29) and d 18-21 (n=29) (0.93, 1.20) (1.16, 1.43) (1.66, 2.21) ddI: 200 mg x 1 dose, 400 mg x 1 dose 0.11 0.13 0.16 didanosine d4T: 40 mg x 1 dose simultaneously with (0.06, 0.18) (0.08, 0.21) (0.10, 0.27) (ddI) (n=31) ddI and d4T (buffered (n=31) tablets) plus ddl: 200 mg x 1 dose, 400 mg x 1 dose 1.12 1.03 1.03 stavudine d4T: 40 mg x 1 dose 1 h after ddI + d4T (0.67, 1.18) (0.64, 1.67) (0.61, 1.73) (d4T)b (n=32) (n=32) efavirenz 600 mg QD, d 7-20 400 mg QD, d 1-20 0.41 0.26 0.07 (n=27) (n=27) (0.33, 0.51) (0.22, 0.32) (0.05, 0.10) 600 mg QD, d 7-20 400 mg QD, d 1-6 1.14 1.39 1.48 (n=13) (n=23) then 300 (0.83, 1.58) (1.02, 1.88) (1.24, 1.76) mg/ritonavir 100 mg QD, 2 h before efavirenz, d 7-20 (n=13) 600 mg QD, 300 mg QD/ritonavir 1.17 1.00 0.58 d 11-24 (pm) 100 mg QD, d 1-10 (1.08, 1.27) (0.91, 1.10) (0.49, 0.69) (n=14) (pm) (n=22), then 400 mg QD/ritonavir 100 mg QD, d 11-24 (pm), (simultaneously with efavirenz) (n=14) famotidine 40 mg BID, d 7-12 400 mg QD, d 1-6 0.53 0.59 0.58 (n=15) (n=45), d 7-12 (0.34, 0.82) (0.40, 0.87) (0.37, 0.89) (simultaneous administration) (n=15) 40 mg BID, d 7-12 400 mg QD (pm), d 1- 1.08 0.95 0.79 (n=14) 6 (n=14), d 7-12 (10 h (0.82, 1.41) (0.74, 1.21) (0.60, 1.04) after, 2 h before famotidine) (n=14) 40 mg BID, d 11-20 300 mg QD/ritonavir 0.86 0.82 0.72 (n=14)c 100 mg QD, d 1-10 (0.79, 0.94) (0.75, 0.89) (0.64, 0.81) (n=46), d 11-20d (simultaneous administration) (n=14) 20 mg BID, d 11-17 300 mg QD/ritonavir 0.91 0.90 0.81 (n=18) 100 mg QD/tenofovir (0.84, 0.99) (0.82, 0.98) (0.69, 0.94) DF 300 mg QD, d 1- 10 (am) (n=39), d 11- 17 (am) (simultaneous Coadministe Coadministered Atazanavir Ratio (90% Confidence Interval) of red Drug Drug Dose/Schedule Dose/Schedule Atazanavir Pharmacokinetic Parameters with/without Coadministered Drug; No Effect = 1.00 Cmax AUC Cmin administration with am famotidine) (n=18)d,e 40 mg QD (pm), 300 mg QD/ritonavir 0.89 0.88 0.77 d 18-24 100 mg QD/tenofovir (0.81, 0.97) (0.80, 0.96) (0.63, 0.93) (n=20) DF 300 mg QD, d 1-10 (am) (n=39), d 18-24 (am) (12 h after pm famotidine) (n=20)e 40 mg BID, d 18-24 300 mg QD/ritonavir 0.74 0.79 0.72 (n=18) 100 mg QD/tenofovir (0.66, 0.84) (0.70, 0.88) (0.63, 0.83) DF 300 mg QD, d 1-10 (am) (n=39), d 18-24 (am) (10 h after pm famotidine and 2 h before am famotidine) (n=18)e 40 mg BID, d 11-20 300 mg QD/ritonavir 1.02 1.03 0.86 (n=15) 100 mg QD, d 1-10 (0.87, 1.18) (0.86, 1.22) (0.68, 1.08) (am) (n=46), then 400 mg QD/ritonavir 100 mg QD, d 11-20 (am) (n=15) grazoprevir/ grazoprevir 200 mg 300 mg QD/ritonavir 1.12 1.43 1.23 elbasvir QD 100 mg QD, d 1- 35 (1.01, 1.24) (1.30, 1.57) (1.13, 1.34) d 1 - 35 (n = 11) (n = 11) elbasvir 50 mg QD 300 mg QD/ritonavir 1.02 1.07 1.15 d 1 - 35 100 mg QD, d 1 - 35 (0.96, 1.08) (0.98,1.17) (1.02, 1.29) (n = 8) (n = 8) ketoconazole 200 mg QD, d 7-13 400 mg QD, d 1-13 0.99 1.10 1.03 (n=14) (n=14) (0.77, 1.28) (0.89, 1.37) (0.53, 2.01) f,g nevirapine 200 mg BID, 300 mg QD/ritonavir 0.72 0.58 0.28 d 1-23 100 mg QD, d 4-13, (0.60, 0.86) (0.48, 0.71) (0.20, 0.40) (n=23) then 1.02 0.81 0.41 400 mg QD/ritonavir (0.85, 1.24) (0.65, 1.02) (0.27, 0.60) 100 mg QD, d 14-23 (n=23)h omeprazole 40 mg QD, d 7-12 400 mg QD, d 1-6 0.04 0.06 0.05 (n=16)i (n=48), d 7-12 (n=16) (0.04, 0.05) (0.05, 0.07) (0.03, 0.07) 40 mg QD, d 11-20 300 mg QD/ritonavir 0.28 0.24 0.22 (n=15)i 100 mg QD, d 1-20 (0.24, 0.32) (0.21, 0.27) (0.19, 0.26) (n=15) Coadministe Coadministered Atazanavir Ratio (90% Confidence Interval) of red Drug Drug Dose/Schedule Dose/Schedule Atazanavir Pharmacokinetic Parameters with/without Coadministered Drug; No Effect = 1.00 Cmax AUC Cmin 20 mg QD, d 17-23 300 mg QD/ritonavir 0.61 0.58 0.54 (am) (n=13) 100 mg QD, d 7-16 (0.46, 0.81) (0.44, 0.75) (0.41, 0.71) (pm) (n=27), d 17-23 (pm) (n=13)j,k 20 mg QD, d 17-23 300 mg QD/ritonavir 0.69 0.70 0.69 (am) (n=14) 100 mg QD, d 7-16 (0.58, 0.83) (0.57, 0.86) (0.54, 0.88) (am) (n=27), then 400 mg QD/ritonavir 100 mg QD, d 17-23 (am) (n=14)l,m pitavastatin 4 mg QD for 5 days 300 mg QD for 5 days 1.13 1.06 NA (0.96, 1.32) (0.90, 1.26) rifabutin 150 mg QD, d 15-28 400 mg QD, d 1-28 1.34 1.15 1.13 (n=7) (n=7) (1.14, 1.59) (0.98, 1.34) (0.68, 1.87) rifampin 600 mg QD, d 17-26 300 mg QD/ritonavir 0.47 0.28 0.02 (n=16) 100 mg QD, d 7-16 (0.41, 0.53) (0.25, 0.32) (0.02, 0.03) (n=48), d 17-26 (n=16) ritonavirn 100 mg QD, d 11-20 300 mg QD, d 1-20 1.86 3.38 11.89 (n=28) (n=28) (1.69, 2.05) (3.13, 3.63) (10.23, 13.82) tenofovir DFo 300 mg QD, d 9-16 400 mg QD, d 2-16 0.79 0.75 0.60 (n=34) (n=34) (0.73, 0.86) (0.70, 0.81) (0.52, 0.68) 300 mg QD, d 15-42 300 mg/ritonavir 100 0.72p 0.75p 0.77p (n=10) mg QD, d 1-42 (n=10) (0.50, 1.05) (0.58, 0.97) (0.54, 1.10) voriconazole 200 mg BID, d 2-3, 300 mg/ritonavir 100 0.87 0.88 0.80 (Subjects 22-30; mg QD, d 11-30 (0.80, 0.96) (0.82, 0.95) (0.72, 0.90) with at least 400 mg BID, d 1, 21 (n=20) one (n=20) functional CYP2C19 allele) voriconazole 50 mg BID, d 2-3, 22- 300 mg/ritonavir 100 0.81 0.80 0.69 (Subjects 30; mg QD, d 11-30 (0.66, 1.00) (0.65, 0.97) (0.54, 0.87) without a 100 mg BID, d 1, 21 (n=8) functional (n=8) CYP2C19 allele) a. Data provided are under fed conditions unless otherwise noted. b. All drugs were given under fasted conditions. c. Atazanavir 300 mg with ritonavir 100 mg once daily coadministered with famotidine 40 mg twice daily resulted in atazanavir geometric mean Cmax that was similar and AUC and Cmin values that were 1.79- and 4.46-fold higher relative to Atazanavir 400 mg once daily alone. d. Similar results were noted when famotidine 20 mg BID was administered 2 hours after and 10 hours before atazanavir 300 mg with ritonavir 100 mg and tenofovir DF 300 mg. e. coadmivistration of Atazanavir with ritonavir 100 mg and tenofovir DF was administered after a light meal. f. Study was conducted in subjects with HIV-1 infection. g. Compared with atazanavir 400 mg historical data without nevirapine (n=13), the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 1.42 (0.98, 2.05), 1.64 (1.11, 2.42), and 1.25 (0.66, 2.36), respectively, for atazanavir/ritonavir 300/100 mg; and 2.02 (1.42, 2.87), 2.28 (1.54, 3.38), and 1.80 (0.94, 3.45), respectively, for atazanavir/ritonavir 400/100 mg. h. Parallel group design; n=23 for atazanavir/ritonavir and nevirapine, n=22 for atazanavir 300 mg/ritonavir 100 mg without nevirapine. Subjects were treated with nevirapine prior to study entry. i. Omeprazole 40 mg was administered on an empty stomach 2 hours before atazanavir. j. Omeprazole 20 mg was administered 30 minutes prior to a light meal in the morning and atazanavir 300 mg with ritonavir 100 mg in the evening after a light meal, separated by 12 hours from omeprazole. k. Atazanavir 300 mg with ritonavir 100 mg once daily separated by 12 hours from omeprazole 20 mg daily resulted in increases in atazanavir geometric mean AUC (10%) and Cmin (2.4-fold), with a decrease in Cmax (29%) relative to atazanavir 400 mg once daily in the absence of omeprazole (study days 1-6). l. Omeprazole 20 mg was given 30 minutes prior to a light meal in the morning and atazanavir 400 mg with ritonavir 100 mg once daily after a light meal, 1 hour after omeprazole. Effects on atazanavir concentrations were similar when atazanavir 400 mg with ritonavir 100 mg was separated from omeprazole 20 mg by 12 hours. m. Atazanavir 400 mg with ritonavir 100 mg once daily administered with omeprazole 20 mg once daily resulted in increases in atazanavir geometric mean AUC (32%) and Cmin (3.3-fold), with a decrease in Cmax (26%) relative to atazanavir 400 mg once daily in the absence of omeprazole (study days 1-6). n. Compared with atazanavir 400 mg QD historical data, administration of atazanavir/ritonavir 300/100 mg QD increased the atazanavir geometric mean values of Cmax, AUC, and Cmin by 18%, 103%, and 671%, respectively. o. Note that similar results were observed in studies where administration of tenofovir DF and atazanavir was separated by 12 hours. p. Ratio of atazanavir with ritonavir and tenofovir DF to atazanavir with ritonavir. Atazanavir 300 mg with ritonavir 100 mg results in higher atazanavir exposure than atazanavir 400 mg (see footnote o). The geometric mean values of atazanavir pharmacokinetic parameters when coadministered with ritonavir and tenofovir DF were: Cmax = 3190 ng/mL, AUC = 34459 ng*h/mL, and Cmin = 491 ng/mL. Study was conducted in subjects with HIV-1 infection. NA = not available. Table 21: Drug Interactions: Pharmacokinetic Parameters for Coadministered Drugs in the Presence of Atazanavira Coadministered Atazanavir Ratio (90% Confidence Interval) of Coadministered Coadministered Drug Dose/Schedule Drug Pharmacokinetic Parameters with/without Drug atazanavir; No Effect = 1.00 Dose/Schedule Cmax AUC Cmin acetaminophen 1 gm BID, d 1- 300 mg 0.87 0.97 1.26 20 (n=10) QD/ritonavir (0.77, 0.99) (0.91, 1.03) (1.08, 1.46) 100 mg QD, d 11- Coadministered Atazanavir Ratio (90% Confidence Interval) of Coadministered Coadministered Drug Dose/Schedule Drug Pharmacokinetic Parameters with/without Drug atazanavir; No Effect = 1.00 Dose/Schedule Cmax AUC Cmin 20 (n=10) atenolol 50 mg QD, d 7- 400 mg QD, d 1-11 1.34 1.25 1.02 11 (n=19) and d (n=19) (1.26, 1.42) (1.16, 1.34) (0.88, 1.19) 19-23 clarithromycin 500 mg BID, d 400 mg QD, d 1-10 1.50 1.94 2.60 7-10 (n=21) and (n=21) (1.32, 1.71) (1.75, 2.16) (2.35, 2.88) d18-21 OH- OH-clarithromycin: OH- clarithromycin: 0.30 clarithromycin: 0.28 (0.26, 0.34) 0.38 (0.24, 0.33) (0.34, 0.42) ddI (enteric- 400 mg d 1 400 mg QD, d 2-8 0.64 0.66 1.13 coated [EC] (fasted), d 8 (n=34) (0.55, 0.74) (0.60, 0.74) (0.91, 1.41) capsules)b (fed) (n=34) 400 mg d 1 300 mg 0.62 0.66 1.25 (fasted), d 19 QD/ritonavir (0.52, 0.74) (0.59, 0.73) (0.92, 1.69) (fed) 100 mg QD, d 9-19 (n=31) (n=31) diltiazem 180 mg QD, d 7- 400 mg QD, d 1-11 1.98 2.25 2.42 11 (n=28) and d (n=28) (1.78, 2.19) (2.09, 2.16) (2.14, 2.73) 19-23 desacetyl- desacetyl-diltiazem: desacetyl- diltiazem: 2.65 diltiazem: 2.72 (2.45, 2.87) 2.21 (2.44, 3.03) (2.02, 2.42) ethinyl estradiol Ortho-Novum® 400 mg QD, d16-29 ethinyl estradiol: ethinyl estradiol: ethinyl estradiol: & norethindronec 7/7/7 QD, (n=19) 1.15 1.48 1.91 d 1–29 (0.99, 1.32) (1.31, 1.68) (1.57, 2.33) (n=19) norethindrone: norethindrone: 2.10 norethindrone: 1.67 (1.68, 2.62) 3.62 (1.42, 1.96) (2.57, 5.09) ethinyl estradiol Ortho Tri- 300 mg ethinyl estradiol: ethinyl estradiol: ethinyl & norgestimated Cyclen® QD, d QD/ritonavir 0.84 0.81 estradiol: 1–28 (n=18), 100 mg QD, (0.74, 0.95) (0.75, 0.87) 0.63 then Ortho Tri- d29-42 17-deacetyl 17-deacetyl (0.55, 0.71) Cyclen® LO (n=14) norgestimate:f norgestimate:f 17-deacetyl QD, d 29–42e 1.68 1.85 norgestima (n=14) (1.51, 1.88) (1.67, 2.05) te:f 2.02 (1.77, 2.31) glecaprevir/ 300 mg 300 mg ≥4.06g ≥6.53g ≥14.3g pibrentasvir glecaprevir QD/ritonavir (3.15, 5.23) (5.24, 8.14) (9.85, 20.7) (n=12) 100 mg QD (n=12) 120 mg 300 mg ≥1.29g ≥1.64g ≥2.29g pibrentasvir QD/ritonavir (1.15, 1.45) (1.48, 1.82) (1.95, 2.68) (n=12) 100 mg QD Coadministered Atazanavir Ratio (90% Confidence Interval) of Coadministered Coadministered Drug Dose/Schedule Drug Pharmacokinetic Parameters with/without Drug atazanavir; No Effect = 1.00 Dose/Schedule Cmax AUC Cmin (n=12) grazoprevir/ grazoprevir 200 300 mg 6.24 10.58 11.64 elbasvir mg QD/ritonavir (4.42, 8.81) (7.78, 14.39) (7.96, 17.02) QD 100 mg QD d 1 - 35 d 1 - 35 (n = 12) (n=12) elbasvir 50 mg 300 mg 4.15 4.76 6.45 QD QD/ritonavir (3.46, 4.97) (4.07, 5.56) (5.51 7.54) d 1 - 35 100 mg QD (n = 10) d 1 - 35 (n=10) methadone Stable 400 mg QD, d 2-15 (R)-methadoneh (R)-methadoneh (R)-methadoneh maintenance (n=16) 0.91 1.03 1.11 dose, d 1-15 (0.84, 1.0) (0.95, 1.10) (1.02, 1.20) (n=16) total: 0.85 total: 0.94 total: 1.02 (0.78, 0.93) (0.87, 1.02) (0.93, 1.12) nevirapine,i,J 200 mg BID, d 300 mg QD/ 1.17 1.25 1.32 1-23 (n=23) ritonavir 100 mg (1.09, 1.25) (1.17, 1.34) (1.22, 1.43) QD, d 4-13, then 1.21 1.26 1.35 400 mg QD/ (1.11, 1.32) (1.17, 1.36) (1.25, 1.47) ritonavir 100 mg QD, d 14-23 (n=23) omeprazolek 40 mg single 400 mg QD, d 1-12 1.24 1.45 NA dose, (n=16) (1.04, 1.47) (1.20, 1.76) d 7 and d 20 (n=16) rifabutin 300 mg QD, d 1- 600 mg QD,1 1.18 2.10 3.43 10 then 150 mg d 11-20 (0.94, 1.48) (1.57, 2.79) (1.98, 5.96) QD, (n=3) 25-O-desacetyl- 25-O-desacetyl- 25-O-desacetyl- d 11-20 rifabutin: 8.20 rifabutin: 22.01 rifabutin: 75.6 (n=3) (5.90, 11.40) (15.97, 30.34) (30.1, 190.0) 150 mg twice 300 mg QD/ 2.49m 1.48m 1.40m weekly, d 1-15 ritonavir 100 mg (2.03, 3.06) (1.19, 1.84) (1.05, 1.87) (n=7) QD, d 1-17 (n=7) 25-O-desacetyl- 25-O-desacetyl- 25-O-desacetyl- rifabutin: 7.77 rifabutin: 10.90 rifabutin: 11.45 (6.13, 9.83) (8.14, 14.61) (8.15, 16.10) pitavastatin 4 mg QD for 5 300 mg QD for 5 1.60 1.31 NA days days (1.39, 1.85) (1.23, 1.39) rosiglitazonen 4 mg single 400 mg QD, d 2-7, 1.08 1.35 NA dose, then (1.03, 1.13) (1.26, 1.44) NA d 1, 7, 17 300 mg QD/ 0.97 0.83 (n=14) ritonavir 100 mg (0.91, 1.04) (0.77, 0.89) QD, d 8-17 (n=14) rosuvastatin 10 mg single 300 mg QD/ ↑7-foldo ↑ 3-foldo NA Coadministered Atazanavir Ratio (90% Confidence Interval) of Coadministered Coadministered Drug Dose/Schedule Drug Pharmacokinetic Parameters with/without Drug atazanavir; No Effect = 1.00 Dose/Schedule Cmax AUC Cmin dose ritonavir 100 mg QD for 7 days saquinavirp (soft 1200 mg QD, 400 mg QD, 4.39 5.49 6.86 gelatin capsules) d 1-13 d 7-13 (3.24, 5.95) (4.04, 7.47) (5.29, 8.91) (n=7) (n=7) sofosbuvir/ 400 mg 300 mg/100 mg 1.29 1.40 NA velpatasvir/ sofosbuvir ritonavir single dose (1.09, 1.52) (1.25, 1.57) voxilaprevir single dose (n=15) sofosbuvir sofosbuvir (n=15) metabolite metabolite GS-331007 GS-331007 1.05 1.25 (0.99, 1.12) (1.16, 1.36) 100 mg 300 mg/100 mg 1.29 1.93 NA velpatasvir ritonavir single dose (1.07, 1.56) (1.58, 2.36) single dose (n=15) (n=15) 100 mg 300 mg/100 mg 4.42 4.31 NA voxilaprevir ritonavir single dose (3.65, 5.35) (3.76, 4.93) single dose (n=15) (n=15) Tenofovir DFq 300 mg QD, d 9- 400 mg QD, d 2-16 1.14 1.24 1.22 16 (n=33) and d (n=33) (1.08, 1.20) (1.21, 1.28) (1.15, 1.30) 24-30 (n=33) 300 mg QD, d 1- 300 mg 1.34 1.37 1.29 7 (pm) (n=14) QD/ritonavir (1.20, 1.51) (1.30, 1.45) (1.21, 1.36) d 25-34 (pm) 100 mg QD, d 25- (n=12) 34 (am) (n=12)r voriconazole 200 mg BID, d 300 mg/ritonavir 0.90 0.67 0.61 (Subjects with at 2-3, 22-30; 100 mg QD, d 11- (0.78, 1.04) (0.58, 0.78) (0.51, 0.72) least one 400 mg BID, d 30 functional 1, 21 (n=20) CYP2C19 allele) (n=20) 300 mg/ritonavir 4.38 5.61 7.65 voriconazole 50 mg BID, d 2- 100 mg QD, d 11- (3.55, 5.39) (4.51, 6.99) (5.71, 10.2) (Subjects without 3, 22-30; 30 a functional 100 mg BID, d (n=8) CYP2C19 allele) 1, 21 (n=8) lamivudine + 150 mg 400 mg QD, d 7-12 lamivudine: 1.04 lamivudine: 1.03 lamivudine: 1.12 zidovudine lamivudine + (n=19) (0.92, 1.16) (0.98, 1.08) (1.04, 1.21) 300 mg zidovudine: 1.05 zidovudine: 1.05 zidovudine: 0.69 zidovudine BID, (0.88, 1.24) (0.96, 1.14) (0.57, 0.84) d 1-12 zidovudine zidovudine zidovudine (n=19) glucuronide: 0.95 glucuronide: glucuronide: (0.88, 1.02) 1.00 0.82 (0.97, 1.03) (0.62, 1.08) a. Data provided are under fed conditions unless otherwise noted. b. 400 mg ddI EC and atazanavir were administered together with food on Days 8 and 19. c. Upon further dose normalization of ethinyl estradiol 25 mcg with atazanavir relative to ethinyl estradiol 35 mcg without atazanavir, the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 0.82 (0.73, 0.92), 1.06 (0.95, 1.17), and 1.35 (1.11, 1.63), respectively. d. Upon further dose normalization of ethinyl estradiol 35 mcg with atazanavir/ritonavir relative to ethinyl estradiol 25 mcg without atazanavir/ritonavir, the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 1.17 (1.03, 1.34), 1.13 (1.05, 1.22), and 0.88 (0.77, 1.00), respectively. e. All subjects were on a 28 day lead-in period; one full cycle of Ortho Tri-Cyclen®. Ortho Tri- Cyclen® contains 35 mcg of ethinyl estradiol. Ortho Tri-Cyclen® LO contains 25 mcg of ethinyl estradiol. Results were dose normalized to an ethinyl estradiol dose of 35 mcg. f. 17-deacetyl norgestimate is the active component of norgestimate. g. Effect of atazanavir and ritonavir on the first dose of glecaprevir and pibrentasvir is reported. h. (R)-methadone is the active isomer of methadone. i. Study was conducted in subjects with HIV-1 infection. j. Subjects were treated with nevirapine prior to study entry. k. Omeprazole was used as a metabolic probe for CYP2C19. Omeprazole was given 2 hours after atazanavir on Day 7; and was given alone 2 hours after a light meal on Day 20. l. Not the recommended therapeutic dose of atazanavir. m. When compared to rifabutin 150 mg QD alone d1-10 (n=14). Total of rifabutin + 25-O-desacetyl- rifabutin: AUC 2.19 (1.78, 2.69). n. Rosiglitazone used as a probe substrate for CYP2C8. o. Mean ratio (with/without coadministered drug). ↑ indicates an increase in rosuvastatin exposure. p. The combination of atazanavir and saquinavir 1200 mg QD produced daily saquinavir exposures similar to the values produced by the standard therapeutic dosing of saquinavir at 1200 mg TID. However, the Cmax is about 79% higher than that for the standard dosing of saquinavir (soft gelatin capsules) alone at 1200 mg TID. q. Note that similar results were observed in a study where administration of tenofovir DF and atazanavir was separated by 12 hours. r. Administration of tenofovir DF and atazanavir was temporally separated by 12 hours. NA = not available. 11.4. Microbiology Mechanism of Action Atazanavir (ATV) is an azapeptide HIV-1 protease inhibitor (PI). The compound selectively inhibits the virus-specific processing of viral Gag and Gag-Pol polyproteins in HIV-1 infected cells, thus preventing formation of mature virions. Antiviral Activity in Cell Culture Atazanavir exhibits anti-HIV-1 activity with a mean 50% effective concentration (EC50) in the absence of human serum of 2 to 5 nM against a variety of laboratory and clinical HIV-1 isolates grown in peripheral blood mononuclear cells, macrophages, CEM-SS cells, and MT-2 cells. Atazanavir has activity against HIV-1 Group M subtype viruses A, B, C, D, AE, AG, F, G, and J isolates in cell culture. Atazanavir has variable activity against HIV-2 isolates (1.9-32 nM), with EC50 values above the EC50 values of failure isolates. Two-drug combination antiviral activity studies with atazanavir showed no antagonism in cell culture with PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir), NNRTIs (delavirdine, efavirenz, and nevirapine), NRTIs (abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir DF, and zidovudine), the HIV-1 fusion inhibitor enfuvirtide, and two compounds used in the treatment of viral hepatitis, adefovir and ribavirin, without enhanced cytotoxicity. Resistance In Cell Culture: HIV-1 isolates with a decreased susceptibility to atazanavir have been selected in cell culture and obtained from patients treated with atazanavir or atazanavir/ritonavir. HIV-1 isolates with 93- to 183-fold reduced susceptibility to atazanavir from three different viral strains were selected in cell culture by 5 months. The substitutions in these HIV-1 viruses that contributed to atazanavir resistance include I50L, N88S, I84V, A71V, and M46I. Changes were also observed at the protease cleavage sites following drug selection. Recombinant viruses containing the I50L substitution without other major PI substitutions were growth impaired and displayed increased susceptibility in cell culture to other PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir). The I50L and I50V substitutions yielded selective resistance to atazanavir and amprenavir, respectively, and did not appear to be cross- resistant. Clinical Studies of Treatment-Naive Patients: Comparison of Ritonavir-Boosted atazanavir vs. Unboosted atazanavir : Study AI424-089 compared atazanavir 300 mg once daily with ritonavir 100 mg vs. atazanavir 400 mg once daily when administered with lamivudine and extended- release stavudine in treatment-naive subjects with HIV-1 infection . A summary of the number of virologic failures and virologic failure isolates with atazanavir resistance in each arm is shown in Table 22. Table 22: Summary of Virologic Failuresa at Week 96 in Study AI424-089: Comparison of Ritonavir Boosted atazanavir vs. Unboosted Atazanavir: Randomized Patients Atazanavir 300 mg + Atazanavir 400 mg ritonavir 100 mg (n=105) (n=95) Virologic Failure (≥50 copies/mL) at Week 96 15 (16%) 34 (32%) Virologic Failure with Genotypes and 5 17 Phenotypes Data Virologic Failure Isolates with ATV-resistance 0/5 (0%)b 4/17 (24%)b at Week 96 Virologic Failure Isolates with I50L Emergence 0/5 (0%)b 2/17 (12%)b at Week 96c Virologic Failure Isolates with Lamivudine 2/5 (40%)b 11/17 (65%)b Resistance at Week 96 a Virologic failure includes subjects who were never suppressed through Week 96 and on study at Week 96, had virologic rebound or discontinued due to insufficient viral load response. b Percentage of Virologic Failure Isolates with genotypic and phenotypic data. c Mixture of I50I/L emerged in 2 other atazanavir 400 mg-treated subjects. Neither isolate was phenotypically resistant to atazanavir. Clinical Studies of Treatment-Naive subjects Receiving atazanavir 300 mg with Ritonavir 100 mg: In Phase 3 Study AI424-138, an as-treated genotypic and phenotypic analysis was conducted on samples from subjects who experienced virologic failure (HIV-1 RNA ≥400 copies/mL) or discontinued before achieving suppression on atazanavir with ritonavir (n=39; 9%) and lopinavir/ritonavir (n=39; 9%) through 96 weeks of treatment. In the atazanavir with ritonavir arm, one of the virologic failure isolates had a 56- fold decrease in atazanavir susceptibility emerge on therapy with the development of PI resistance- associated substitutions L10F, V32I, K43T, M46I, A71I, G73S, I85I/V, and L90M. The NRTI resistance- associated substitution M184V also emerged on treatment in this isolate conferring emtricitabine resistance. Two atazanavir with ritonavir -virologic failure isolates had baseline phenotypic atazanavir resistance and IAS-defined major PI resistance-associated substitutions at baseline. The I50L substitution emerged on study in one of these failure isolates and was associated with a 17-fold decrease in atazanavir susceptibility from baseline and the other failure isolate with baseline atazanavir resistance and PI substitutions (M46M/I and I84I/V) had additional IAS-defined major PI substitutions (V32I, M46I, and I84V) emerge on atazanavir treatment associated with a 3-fold decrease in atazanavir susceptibility from baseline. Five of the treatment failure isolates in the atazanavir with ritonavir arm developed phenotypic emtricitabine resistance with the emergence of either the M184I (n=1) or the M184V (n=4) substitution on therapy and none developed phenotypic tenofovir disoproxil resistance. In the lopinavir/ritonavir arm, one of the virologic failure subjects isolates had a 69-fold decrease in lopinavir susceptibility emerge on therapy with the development of PI substitutions L10V, V11I, I54V, G73S, and V82A in addition to baseline PI substitutions L10L/I, V32I, I54I/V, A71I, G73G/S, V82V/A, L89V, and L90M. Six lopinavir/ritonavir virologic failure isolates developed the M184V substitution and phenotypic emtricitabine resistance and two developed phenotypic tenofovir disoproxil resistance. Clinical Studies of Treatment-Naive subjects Receiving atazanavir 400 mg without Ritonavir: atazanavir - resistant clinical isolates from treatment-naive subjects who experienced virologic failure on atazanavir 400 mg treatment without ritonavir often developed an I50L substitution (after an average of 50 weeks of atazanavir therapy), often in combination with an A71V substitution, but also developed one or more other PI substitutions (eg, V32I, L33F, G73S, V82A, I85V, or N88S) with or without the I50L substitution. In treatment-naive subjects, viral isolates that developed the I50L substitution, without other major PI substitutions, showed phenotypic resistance to atazanavir but retained in cell culture susceptibility to other PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir); however, there are no clinical data available to demonstrate the effect of the I50L substitution on the efficacy of subsequently administered PIs. Clinical Studies of Treatment-Experienced subjects: In studies of treatment-experienced subjects treated with atazanavir or atazanavir with ritonavir, most atazanavir -resistant isolates from patients who experienced virologic failure developed substitutions that were associated with resistance to multiple PIs and displayed decreased susceptibility to multiple PIs. The most common protease substitutions to develop in the viral isolates of subjects who failed treatment with atazanavir 300 mg once daily and ritonavir 100 mg once daily (together with tenofovir DF and an NRTI) included V32I, L33F/V/I, E35D/G, M46I/L, I50L, F53L/V, I54V, 71V/T/I, G73S/T/C, V82A/T/L, I85V, and L89V/Q/M/T. Other substitutions that developed on atazanavir with ritonavir treatment including E34K/A/Q, G48V, I84V, N88S/D/T, and L90M occurred in less than 10% of subjects isolates. Generally, if multiple PI resistance substitutions were present in the HIV-1 virus of the subject at baseline, atazanavir resistance developed through substitutions associated with resistance to other PIs and could include the development of the I50L substitution. The I50L substitution has been detected in treatment-experienced subjects experiencing virologic failure after long-term treatment. Protease cleavage site changes also emerged on atazanavir treatment but their presence did not correlate with the level of atazanavir resistance. Clinical Studies of Pediatric Subjects in AI424-397 (PRINCE I) and AI424-451 (PRINCE II): Treatment- emergent atazanavir with ritonavir resistance-associated amino acid substitution M36I in the protease was detected in the virus of one subject among treatment failures in AI424-397. In addition, three known resistance-associated substitutions for other PIs arose in the viruses from one subject each (L19I/R, H69K/R, and I72I/V). Reduced susceptibility to atazanavir, ritonavir, or atazanavir with ritonavir was not seen with these viruses. In AI424-451, atazanavir with ritonavir resistance-associated substitutions G16E, V82A/I/T, I84V, and/or L90M arose in the viruses of two subjects. The virus population harboring the M46M/V, V82V/I, I84I/V, and L90L/M substitutions acquired phenotypic resistance to ritonavir (ritonavir phenotypic fold-change of 3.5, with a ritonavircutoff of 2.5- fold change). However, these substitutions did not result in phenotypic resistance to atazanavir (atazanavirphenotypic fold-change of <1.8, with an atazanavircutoff of 2.2-fold change). Secondary PI resistance-associated amino acid substitutions also arose in the viruses of one subject each, including V11V/I, D30D/G, E35E/D, K45K/R, L63P/S, and I72I/T. Q61D and Q61E/G emerged in the viruses of two subjects who failed treatment with atazanavir with ritonavir. Viruses from nine subjects in the two studies developed NRTI resistance- associated substitutions: K65K/R (n=1), M184V (n=7), and T215I (n=1). Cross-Resistance Cross-resistance among PIs has been observed. Baseline phenotypic and genotypic analyses of clinical isolates from atazanavir clinical trials of PI-experienced subjects showed that isolates crossresistant to multiple PIs were cross-resistant to atazanavir. Greater than 90% of the isolates with substitutions that included I84V or G48V were resistant to atazanavir. Greater than 60% of isolates containing L90M, G73S/T/C, A71V/T, I54V, M46I/L, or a change at V82 were resistant to atazanavir, and 38% of isolates containing a D30N substitution in addition to other changes were resistant to atazanavir. Isolates resistant to atazanavir were also cross-resistant to other PIs with >90% of the isolates resistant to indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir, and 80% resistant to amprenavir. In treatment-experienced subjects, PI-resistant viral isolates that developed the I50L substitution in addition to other PI resistance- associated substitution were also cross-resistant to other PIs. Baseline Genotype/Phenotype and Virologic Outcome Analyses Genotypic and/or phenotypic analysis of baseline virus may aid in determining atazanavir susceptibility before initiation of atazanavir with ritonavir therapy. An association between virologic response at 48 weeks and the number and type of primary PI resistance-associated substitutions detected in baseline HIV- 1 isolates from antiretroviral-experienced subjects receiving atazanavir with ritonavironce daily or lopinavir / ritonavir (fixed-dose product) twice daily in Study AI424-045 is shown in Table 23. Overall, both the number and type of baseline PI substitutions affected response rates in treatment- experienced subjects. In the atazanavir with ritonavir group, subjects had lower response rates when 3 or more baseline PI substitutions, including a substitution at position 36, 71, 77, 82, or 90, were present compared to subjects with 1-2 PI substitutions, including one of these substitutions. Table 23: HIV RNA Response by Number and Type of Baseline PI Substitution, Antiretroviral- Experienced Subjects in Study AI424- 045, As-Treated Analysis Virologic Response = HIV RNA <400 copies/mLb Number and Type of Baseline PI atazanavir with ritonavir opinavir/ritonavirc (n=113) Substitutionsa (n=110) 3 or more primary PI substitutions includingd: D30N 75% (6/8) 50% (3/6) M36I/V 19% (3/16) 33% (6/18) M46I/L/T 24% (4/17) 23% (5/22) I54V/L/T/M/A 31% (5/16) 31% (5/16) A71V/T/I/G 34% (10/29) 39% (12/31) G73S/A/C/T 14% (1/7) 38% (3/8) V77I 47% (7/15) 44% (7/16) V82A/F/T/S/I 29% (6/21) 27% (7/26) I84V/A 11% (1/9) 33% (2/6) N88D 63% (5/8) 67% (4/6) L90M 10% (2/21) 44% (11/25) Number of baseline primary PI substitutionsa All patients, as-treated 58% (64/110) 59% (67/113) 0-2 PI substitutions 75% (50/67) 75% (50/67) 3-4 PI substitutions 41% (14/34) 43% (12/28) 5 or more PI substitutions 0% (0/9) 28% (5/18) a Primary substitutions include any change at D30, V32, M36, M46, I47, G48, I50, I54, A71, G73, V77, V82, I84, N88, and L90. b Results should be interpreted with caution because the subgroups were small. c Administered as a fixed-dose product. d There were insufficient data (n<3) for PI substitutions V32I, I47V, G48V, I50V, and F53L. The response rates of antiretroviral-experienced subjects in Study AI424-045 were analyzed by baseline phenotype (shift in susceptibility in cell culture relative to reference, Table 24). The analyses are based on a select population with 62% of subjects receiving an NNRTI-based regimen before study entry compared to 35% receiving a PI-based regimen. Additional data are needed to determine clinically relevant break points for atazanavir. Table 24: Baseline Phenotype by Outcome, Antiretroviral-Experienced Subjects in Study AI424-045, As-Treated Analysis Virologic Response = HIV-1 RNA <400 copies/mLb Atazanavir with ritonavir lopinavir/ritonavirc Baseline Phenotypea (n=111) (n=111) 0-2 71% (55/78) 70% (56/80) >2-5 53% (8/15) 44% (4/9) >5-10 13% (1/8) 33% (3/9) >10 10% (1/10) 23% (3/13) a Fold change susceptibility in cell culture relative to the wild-type reference. b Results should be interpreted with caution because the subgroups were small. C Administered as a fixed-dose product.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול בנשאי HIV, ובהתקיים אחד מתנאים אלה:1. נשא נגיף ה-HIV פיתח תסמונת הכשל החיסוני הנרכש;2. נשא נגיף ה-HIV הינו אסימפטומטי – עבור נשא העונה על אחד מהבאים:א. נשאי HBVב. נשים הרות או מניקותג. חולים בשחפת פעילהד. נשאים שבני זוגם אינם נשאים ה. נשא נגיף ה-HIV הינו אסימפטומטי עם ערך CD4 קטן מ-500 או ערך עומס נגיפי גדול מ-100,000 עותקי RNA בסמ""ק. ב. מתן התרופה ייעשה לפי מרשם של מנהל מרפאה לטיפול באיידס, במוסד רפואי שהמנהל הכיר בו כמרכז AIDS.ג. משטר הטיפול בתרופה יהיה כפוף להנחיות המנהל, כפי שיעודכנו מזמן לזמן על פי המידע העדכני בתחום הטיפול במחלה.
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/01/2009
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
