Quest for the right Drug
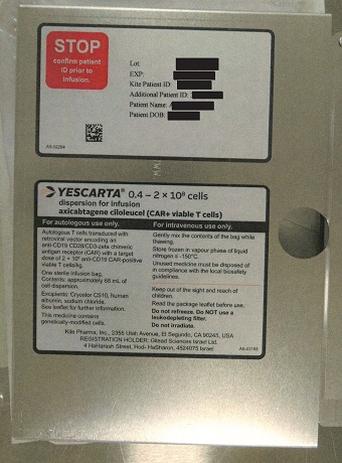
יסקרטה YESCARTA (AXICABTAGENE CILOLEUCEL)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אין פרטים : DISPERSION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects Summary of the safety profile The safety data described in this section are from a total of 397 adult patients treated with Yescarta in three multi-centre pivotal clinical studies (ZUMA-1, ZUMA-5 and ZUMA-7 and post-marketing experience. Adverse reactions are adverse events from pivotal clinical studies and post-marketing experience medically assessed as reasonably attributed to axicabtagene ciloleucel(. Relapsed or refractory DLBCL, PMBCL and DLBCL arising from follicular lymphoma after two or more lines of systemic therapy Safety data from ZUMA-1 reflects exposure to Yescarta in a Phase 1/2 study in which 108 patients received CAR-positive T cells based on a recommended dose which was weight-based. The data described are from the 54-month follow-up analysis where the median actual duration of follow up was 23.5 months (range: 0.3 to 68.2 months). The most significant and frequently occurring adverse reactions were CRS (93%), encephalopathy (60%), and infections (40%). Serious adverse reactions occurred in 51% of patients. The most common (≥ 5%) serious adverse reactions included encephalopathy (22%), unspecified pathogen infections (15%), bacterial infection (6%), viral infection (6%), febrile neutropenia (5%), and fever (5%). The most common (≥5%) Grade 3 or higher non-haematological adverse reactions included encephalopathy (31%), unspecified pathogen infections (19%), CRS (11%), bacterial infection (9%), delirium (6%), hypertension (6%), hypotension (6%), transaminases increased (6%), and viral infection (6%). The most common Grade 3 or higher haematological adverse reactions included lymphopenia (99%), leukopenia (96%), neutropenia (94%), anaemia (65%), and thrombocytopenia (56%). DLBCL and HGBL that relapses within 12 months from completion of, or is refractory to, first-line chemoimmunotherapy Safety data from ZUMA-7 reflects exposure to Yescarta in a Phase 3 study in which 170 patients received CAR-positive T cells based on a recommended dose which was weight-based. The data described are from an analysis where the median actual duration of follow-up was 23.2 months (range: 1.5 to 41.3 months). The most significant and frequently occurring adverse reactions were CRS (92%), encephalopathy (49%), and infections (45%). Serious adverse reactions occurred in 54% of patients. The most common (≥ 5%) serious adverse reactions included CRS (17%), encephalopathy (16%), unspecified pathogen infections (8%), fever (6%) and viral infection (5%). The most common (≥ 5%) Grade 3 or higher non-haematological adverse reactions included encephalopathy (19%), unspecified pathogen infections (8%), CRS (6%), and bacterial infection (5%). The most common Grade 3 or higher haematological adverse reactions included lymphopenia (99%), leukopenia (95%), neutropenia (94%), anaemia (41%), and thrombocytopenia (26%). Follicular lymphoma The safety of Yescarta was evaluated in ZUMA-5, a study that included 146 patients with r/r iNHL (of which 124 patients had r/r FL) who received CD19-positive CAR T cells. Patients with a history of CNS disorders or autoimmune disease requiring systemic immunosuppression were ineligible. The median age was 61 years (range: 34 to 79 years), 43% were female, 93% were white, 3% were black, and 1% were Asian. The most common non-laboratory adverse reactions (incidence ≥ 20%) included fever, CRS, hypotension, encephalopathy, fatigue, headache, infections with pathogen unspecified, tachycardia, febrile neutropenia, musculoskeletal pain, nausea, tremor, chills, diarrhoea, constipation, decreased appetite, cough, vomiting, hypoxia, arrhythmia, and dizziness. Serious adverse reactions occurred in 48% of patients. Serious adverse reactions in > 2% of patients included febrile neutropenia, encephalopathy, fever, CRS, infections with pathogen unspecified, pneumonia, hypoxia, and hypotension. The most common (≥ 10%) Grade 3 or higher reactions included febrile neutropenia, encephalopathy, and infections with pathogen unspecified. Fatal adverse reactions occurred in 1% of patients and included CRS and fungal infection. Fifty-one percent (75/146) of patients received tocilizumab after infusion of Yescarta. In addition, safety data is presented below from a subset of 119 patients with r/r FL only from the 24- month follow-up analysis where the median actual duration of follow-up was 25.9 months (range: 0.3 to 44.3 months). For this 24-month analysis, the most significant and frequently occurring adverse reactions were CRS (77%), infections (59%), and encephalopathy (47%). Serious adverse reactions occurred in 45% of patients. The most common (≥ 5%) serious adverse reactions included encephalopathy (16%), unspecified pathogen infections (12%), CRS (12%), and bacterial infection (5%). The most common (≥ 5%) Grade 3 or higher non-haematological adverse reactions included encephalopathy (14%), unspecified pathogen infections (11%), CRS (6%), and bacterial infection (5%). The most common Grade 3 or higher haematological adverse reactions included lymphopenia (99%), leukopenia (94%), neutropenia (92%), thrombocytopenia (34%), and anaemia (33%). Tabulated list of adverse reactions Adverse reactions described in this section were identified in patients exposed to Yescarta in ZUMA-1 (n = 108), ZUMA-5 (n = 119), and ZUMA-7 (n = 170) and from post-marketing reports. These reactions are presented by system organ class and by frequency. Frequencies are defined as: very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1 000 to < 1/100). Within each frequency grouping, adverse reactions are presented in the order of decreasing seriousness. Table 3: Adverse drug reactions identified with Yescarta* System Organ Class (SOC) Frequency Adverse reactions Infections and infestations Very common Unspecified pathogen infections Viral infection Bacterial infection Common Fungal infection Neoplasms benign, malignant and unspecified (including cysts and polyps) Rare Secondary malignancy of T-cell origin Blood and lymphatic system disorders Very common Febrile neutropenia# Neutropenia# Lymphopenia# Leukopenia# Anaemia# Thrombocytopenia# Common Coagulopathya Immune system disorders Very common Cytokine Release Syndrome Immunoglobulins decreasedb Common Hypersensitivity Uncommon Haemophagocytic Lymphohistiocytosis* Metabolism and nutrition disorders Very common Hyponatraemia# Hypophosphataemia# Hyperuricemia#** Hyperglycaemia# Decreased appetitec Common Hypokalaemia# Hypocalcaemia# Hypoalbuminaemia# Dehydrationd Weight decreased Psychiatric disorders Very common Deliriume Insomnia Common Anxiety Affective disorderf Nervous system disorders Very common Encephalopathyg Tremorh Headachei Dizzinessj Common Ataxiak Seizures, including status epilepticus Hemiparesis Facial paralysisl Neuropathy peripheralm Myoclonus Uncommon Quadriplegia Spinal cord oedema Myelitis Dyscalculia Eye disorders Common Visual impairmentn Cardiac disorders Very common Tachycardiao Arrhythmiap System Organ Class (SOC) Frequency Adverse reactions Common Cardiac arrest Cardiac failureq Vascular disorders Very common Hypotensionr Hypertension Common Thrombosiss Respiratory, thoracic and mediastinal disorders Very common Cought Common Respiratory failureu Hypoxiav Pleural effusion Pulmonary oedema Dyspnoeaw Nasal inflammationx Gastrointestinal disorders Very common Vomiting Diarrhoeay Constipation Abdominal painz Nausea Common Dysphagia*** Dry mouthaa Hepatobiliary disorders Very common Transaminases increasedbb Common Hyperbilirubinaemiacc Skin and subcutaneous tissue disorders Very common Rashdd Musculoskeletal and connective tissue disorders Very common Motor dysfunctionee Musculoskeletal painff Uncommon Rhabdomyolysis Renal and urinary disorders Common Renal impairmentgg General disorders and administration site conditions Very common Feverhh Oedemaii Fatiguejj Chills Common Infusion related reactions Pain Uncommon Multiple organ dysfunction syndrome * Haemophagocytic lymphohistiocytosis has been reported in the setting of CRS. ** Hyperuricemia was identified from a pooled analysis of 227 adult patients treated with Yescarta in ZUMA-1 and ZUMA-5. *** Dysphagia has been reported in the setting of neurologic toxicity and encephalopathy. # Frequency based on Grade 3 or higher laboratory parameter. a. Coagulopathy includes coagulopathy, blood fibrinogen decreased, blood fibrinogen increased, disseminated intravascular coagulation, hypofibrinogenaemia, international normalized ratio increased, prothrombin level decreased, prothrombin time prolonged b. Immunoglobulins decreased includes blood immunoglobulin G decreased, hypogammaglobulinaemia c. Decreased appetite includes decreased appetite, hypophagia d. Dehydration includes dehydration, hypovolaemia e. Delirium includes delirium, agitation, delusion, disorientation, hallucination, restlessness f. Affective disorder includes impulsive behavior, mood altered, depression, Panic attack g. Encephalopathy includes encephalopathy, agraphia, altered state of consciousness, amnesia, aphasia, aphonia, apraxia, cognitive disorder, confusional state, depressed level of consciousness, disturbance in attention, dysarthria, dysgraphia, dyskinesia, dyspraxia, hypersomnia, immune effector cell-associated neurotoxicity syndrome, lethargy, leukoencephalopathy, loss of consciousness, memory impairment, mental impairment, mental status changes, metabolic encephalopathy, neurotoxicity, slow speech, somnolence, speech disorder, stupor, toxic encephalopathy h. Tremor includes tremor, head titubation i. Headache includes headache, head discomfort, tension headache j. Dizziness includes dizziness, dizziness postural, presyncope, syncope, vertigo k. Ataxia includes ataxia, balance disorder, gait disturbance l. Facial paralysis includes facial paralysis, facial paresis m. Neuropathy peripheral includes neuropathy peripheral, allodynia, cervical radiculopathy, hyperaesthesia, hypoaesthesia, lumbar radiculopathy, paraesthesia, peripheral sensory neuropathy, peroneal nerve palsy n. Visual impairment includes visual impairment, hemianopia, vision blurred, visual acuity reduced o. Tachycardia includes tachycardia, postural orthostatic tachycardia syndrome, sinus tachycardia p. Arrhythmia includes arrhythmia, atrial fibrillation, atrial flutter, atrioventricular block, bradycardia, bundle branch block right, electrocardiogram QT prolonged, extrasystoles, heart rate increased, heart rate irregular, sinus bradycardia, supraventricular extrasystoles, supraventricular tachycardia, ventricular arrhythmia, ventricular extrasystoles, ventricular tachycardia q. Cardiac failure includes cardiac failure, acute left ventricular failure, ejection fraction decreased, stress cardiomyopathy r. Hypotension includes hypotension, capillary leak syndrome, diastolic hypotension, hypoperfusion, Orthostatic hypotension s. Thrombosis includes thrombosis, axillary vein thrombosis, brachiocephalic vein thrombosis, deep vein thrombosis, device occlusion, embolism, jugular vein thrombosis, peripheral embolism, peripheral ischaemia, pulmonary embolism, splenic vein thrombosis, thrombosis in device t. Cough includes cough, productive cough, upper-airway cough syndrome u. Respiratory failure includes respiratory failure, acute respiratory failure v. Hypoxia includes hypoxia, oxygen saturation decreased w. Dyspnoea includes dyspnoea, dyspnoea exertional x. Nasal inflammation includes rhinitis allergic, Rhinorrhoea y. Diarrhoea includes diarrhoea, colitis, enteritis z. Abdominal pain includes abdominal pain, abdominal discomfort, abdominal pain lower, abdominal pain upper, abdominal tenderness, dyspepsia, epigastric discomfort aa. Dry mouth includes dry mouth, lip dry bb. Transaminases increased includes transaminases increased, alanine aminotransferase increased, aspartate aminotransferase increased, hepatic enzyme increased, hypertransaminasaemia cc. hyperbilirubinaemia increased includes hyperbilirubinemia, blood bilirubin increased dd. Rash includes rash, application site rash, dermatitis, dermatitis allergic, dermatitis bullous, erythema, pruritus, rash erythematous, rash macular, rash maculo-papular, rash pruritic, rash pustular, urticaria ee. Motor dysfunction includes motor dysfunction, muscle contractions involuntary, muscle rigidity, muscle spasms, muscle spasticity, muscle strain, muscle tightness, muscle twitching, muscular weakness ff. Musculoskeletal pain includes musculoskeletal pain, arthralgia, arthritis, back pain, bone pain, flank pain, groin pain, musculoskeletal chest pain, myalgia, neck pain, osteoarthritis, pain in extremity gg. Renal impairment includes acute kidney injury, blood creatinine increased, renal failure hh. Fever includes hyperthermia, pyrexia ii. Oedema includes oedema, face oedema, generalized oedema, localized oedema, oedema genital, oedema peripheral, peripheral swelling, swelling jj. Fatigue includes fatigue, asthenia, decreased activity, malaise Description of selected adverse reactions Cytokine release syndrome In ZUMA-1 and ZUMA-7, CRS occurred in 92% of patients. Eight percent (8%) of patients experienced Grade 3 or higher (severe, life-threatening, and fatal) CRS. The median time to onset was 3 days (range: 1 to 12 days) and the median duration was 7 days (range: 2 to 58 days). Ninety-nine percent (99%) of patients recovered from CRS. No CRS was reported by patients treated with standard of care therapy (SOCT) in ZUMA-7. In ZUMA-5, CRS occurred in 77% of patients. Six percent (6%) of patients experienced Grade 3 or higher (severe, life-threatening, and fatal) CRS. The median time to onset was 4 days (range: 1 to 11 days) and the median duration was 6 days (range: 1 to 27 days). Ninety-nine percent (99%) of patients recovered from CRS. The most common adverse reactions (≥ 20%) that may be associated with CRS included pyrexia (89%), hypotension (50%), tachycardia (47%), chills (30%), and hypoxia (24%). Serious adverse reactions that may be associated with CRS included pyrexia (12%), hypotension (5%), hypoxia (3%), arrhythmia (3%), cardiac failure (2%), fatigue (2%), headache (2%), tachycardia (2%), cardiac arrest (1%), dyspnoea (1%), and tachypnoea (1%). See section 4.4 for monitoring and management guidance. Neurologic adverse reactions In ZUMA-1 and ZUMA-7, neurologic adverse reactions occurred in 63% of patients. Twenty-five percent (25%) of patients experienced Grade 3 or higher (severe or life-threatening) adverse reactions. Neurologic toxicities occurred within the first 7 days of infusion for 75% of patients. The median time to onset was 6 days (range: 1 to 133 days). The median duration was 10 days, with resolution occurring within 3 weeks for 66% of patients following infusion. In ZUMA-5, neurologic adverse reactions occurred in 57% of patients. Sixteen percent (16%) of patients experienced Grade 3 or higher (severe or life-threatening) adverse reactions. Neurologic toxicities occurred within the first 7 days of infusion for 65% of patients. The median time to onset was 7 days (range: 1 to 177 days). The median duration was 14 days, with resolution occurring within 3 weeks for 60% of patients, following infusion. The most common (≥ 5%) neurologic adverse reactions included encephalopathy (51%), tremor (28%), and delirium (14%). Serious neurologic adverse reactions reported in patients included encephalopathy (18%), tremor (2%), delirium (2%), hemiparesis (1%) and seizure (1%). In ZUMA-7, encephalopathy and tremor were reported in 49% and 25% of patients treated with Yescarta compared to 8% and 1% treated with SOCT, respectively. Other neurologic adverse reactions have been reported less frequently in clinical trials and included dysphagia (3%), myelitis (0.2%), and quadriplegia (0.2%). See section 4.4 for monitoring and management guidance. Febrile neutropenia and infections Febrile neutropenia was observed in 10% of patients after Yescarta infusion. Infections occurred in 48% of patients. Grade 3 or higher (severe, life-threatening, or fatal) infections occurred in 19% of patients. Grade 3 or higher unspecified pathogen, bacterial, and viral infections occurred in 12%, 6%, and 5% of patients respectively. The most common site of unspecified pathogen infection was in the respiratory tract. In ZUMA-7, febrile neutropenia and viral infection were reported in 2% and 16% of patients treated with Yescarta compared to 27% and 5% treated with SOCT, respectively. See section 4.4 for monitoring and management guidance. Prolonged cytopenias Grade 3 or higher neutropenia (including febrile neutropenia), anaemia, and thrombocytopenia occurred in 68%, 31%, and 23% of patients, respectively. Prolonged (still present at Day 30 or with an onset at Day 30 or beyond) Grade 3 or higher neutropenia, thrombocytopenia, and anaemia occurred in 26%, 12%, and 6% of patients, respectively. In ZUMA-1, at the time of the 24-month follow-up analysis, Grade 3 or higher neutropenia, thrombocytopenia, and anaemia present after Day 93 occurred in 11%, 7%, and 3% of patients, respectively. In ZUMA-7, Grade 3 or higher neutropenia and thrombocytopenia were reported in 94% and 26% of patients treated with Yescarta compared to 51% and 63% treated with SOCT, respectively. See section 4.4 for management guidance. Hypogammaglobulinaemia Hypogammaglobulinaemia was reported in 15% of patients treated with Yescarta. Cumulatively, 36 (33%) of 108 patients in ZUMA-1 received intravenous immunoglobulin therapy by the time of the 54-month analysis, 28 (16%) of 170 patients in ZUMA-7 received intravenous immunoglobulin therapy by the time of the 23.2 month analysis and 33 (28%) of 119 subjects in ZUMA-5 received intravenous immunoglobulin therapy at the time of the 24-month follow-up analysis. In ZUMA-7, immunoglobulins decreased was reported in 11% of patients treated with Yescarta compared to 1% of patients treated with SOCT. See section 4.4 for management guidance. Immunogenicity The immunogenicity of Yescarta has been evaluated using an enzyme-linked immunosorbent assay (ELISA) for the detection of binding antibodies against FMC63, the originating antibody of the anti-CD19 CAR. Eleven out of 278 patients (4%) tested positive for anti-FMC63 antibodies prior to being treated with Yescarta in ZUMA-1 and ZUMA-7, and 1 patient (1%) in ZUMA-7 who had a negative test result prior to treatment, had a positive test result after treatment in the screening ELISA. Results of a confirmatory cell-based assay, leveraging a properly folded and expressed extracellular portion of the CAR (ScFv, hinge and linker) demonstrated that all patients treated with Yescarta that had a positive result in the screening ELISA were antibody negative at all time points tested. There is no evidence that the kinetics of initial expansion and persistence of Yescarta, or the safety or effectiveness of Yescarta, was altered in these patients. In ZUMA-5, 13 out of 116 patients (11%) tested positive for antibodies in the ELISA screening assay prior to being treated with Yescarta, and 2 subjects who had negative results prior to treatment had positive test results after treatment. Results of a confirmatory cell-based assay demonstrated that all patients treated with Yescarta that had an ELISA positive result were antibody negative, before, during and after treatment. Special population There is limited experience with Yescarta in patients ≥ 75 years of age. Generally, safety and efficacy were similar between patients ≥ 65 years and patients < 65 years of age treated with Yescarta. Outcomes were consistent between patients with Eastern Cooperative Oncology Group (ECOG) of 0 and 1 and by sex. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. מבוגרים החולים בלימפומה מסוג DLBCL (Diffuse large B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 2. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. 3. מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Primary mediastinal B-cell lymphoma, לאחר שני קווי טיפול ומעלה.4. מבוגרים החולים בלימפומה מסוג HGBL (High grade B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel5. מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel.ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה בהמטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Primary mediastinal B-cell lymphoma, לאחר שני קווי טיפול ומעלה | 30/01/2020 | אונקולוגיה | Primary mediastinal B-cell lymphoma | |
| מבוגרים החולים בלימפומה חוזרת או עמידה (רפרקטורית) מסוג Diffuse large B cell lymphoma, לאחר שני קווי טיפול ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 30/01/2020 | אונקולוגיה | Diffuse large b cell lymphoma | |
| מבוגרים החולים בלימפומה פוליקולרית חוזרת או רפרקטורית לאחר שלושה קווי טיפול קודמים ומעלה. במהלך מחלתו יהיה החולה זכאי לטיפול באחת מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | אונקולוגיה | Follicular lymphoma | |
| מבוגרים החולים בלימפומה מסוג HGBL (High grade B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel | 01/02/2023 | אונקולוגיה | HGBL, High grade B cell lymphoma | |
| מבוגרים החולים בלימפומה מסוג DLBCL (Diffuse large B cell lymphoma) שחזרה בתוך 12 חודשים מתום כימואימונותרפיה שניתנה בקו טיפול ראשון, או עמידה לכימואימונותרפיה שניתנה בקו טיפול ראשון. במהלך מחלתו יהיה החולה זכאי לטיפול באחד מאלה – Axicabtagene ciloleucel, Tisagenlecleucel. | 01/02/2023 | אונקולוגיה | DLBCL, Diffuse large B cell lymphoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
30/01/2020
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
ATC
מידע נוסף
עלון מידע לצרכן
11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן אנגלית 11.08.21 - עלון לצרכן עברית 11.08.21 - עלון לצרכן ערבית 05.10.20 - עלון לצרכן אנגלית 05.10.20 - עלון לצרכן עברית 05.10.20 - עלון לצרכן ערבית 14.09.22 - עלון לצרכן אנגלית 14.09.22 - עלון לצרכן עברית 20.09.22 - עלון לצרכן ערבית 29.11.22 - עלון לצרכן אנגלית 29.11.22 - עלון לצרכן עברית 12.12.22 - עלון לצרכן ערבית 21.06.23 - עלון לצרכן אנגלית 11.05.23 - עלון לצרכן אנגלית 11.05.23 - עלון לצרכן עברית 11.05.23 - עלון לצרכן ערבית 12.09.23 - עלון לצרכן אנגלית 12.09.23 - עלון לצרכן עברית 27.09.23 - עלון לצרכן ערבית 12.10.23 - עלון לצרכן אנגלית 12.10.23 - עלון לצרכן אנגלית 12.10.23 - עלון לצרכן עברית 12.10.23 - עלון לצרכן אנגלית 15.10.23 - עלון לצרכן ערבית 01.01.24 - עלון לצרכן אנגלית 31.12.23 - עלון לצרכן עברית 12.01.24 - עלון לצרכן ערבית 28.03.24 - עלון לצרכן אנגלית 28.03.24 - עלון לצרכן עברית 28.03.24 - עלון לצרכן ערבית 13.09.24 - עלון לצרכן אנגלית 13.09.24 - עלון לצרכן עברית 13.09.24 - עלון לצרכן ערבית 05.10.20 - החמרה לעלון 14.09.22 - החמרה לעלון 29.11.22 - החמרה לעלון 11.01.23 - החמרה לעלון 11.05.23 - החמרה לעלון 12.09.23 - החמרה לעלון 06.12.23 - החמרה לעלון 01.01.24 - החמרה לעלון 28.03.24 - החמרה לעלון 13.09.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
יסקרטה