Quest for the right Drug
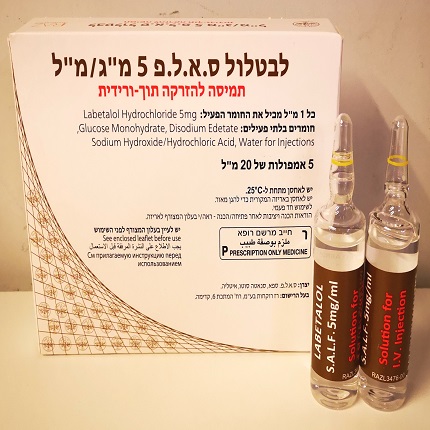
לבטלול ס.א.ל.פ 5 מ"ג/מ"ל LABETALOL S.A.L.F. 5 MG/ML (LABETALOL HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Interactions : אינטראקציות
4.5 Interaction with other medicinal products and other forms of interaction The hypotensive effect of labetalol may be reduced when used in combination with prostaglandin synthetase inhibitors (NSAIDs). Dosage adjustments may therefore be necessary. Additive synergism may occur with other antihypertensive agents. Labetalol fluoresces in alkaline solution at an excitation wavelength of 334 nanometres and a fluorescence wavelength of 412 nanometres , and may therefore interfere with the assays of certain fluorescent substances including catecholamines. The presence of labetalol metabolites in the urine may result in falsely elevated levels or urinary catecholamines, metanephrine, normetanephrine and vanillylmandelic acid, (VMA) when measured by fluorimetric or photometric methods. In screening patients suspected of having a phaeochromocytoma and being treated with labetalol hydrochloride, a specific method such as high performance liquid chromatography with a solid phase extraction should be employed in determining levels of catecholamines. Labetalol has been shown to reduce the uptake of radioisotopes of metaiodobenzylguanidine (MIBG). Care should therefore be taken in interpreting results from MIBG scintigraphy. Concomitant administration of labetalol and adrenaline may result in bradycardia and hypertension (see section 4.4 Special warnings and precautions for use). Care should be taken if labetalol is used concomitantly with either Class I antiarrhythmic agents or calcium antagonists of the verapamil type. Increased risk of myocardial depression in combination with Class I antiarrhythmic (e.g. disopyramide and quinidine) and amiodarone (Class II antiarrhythmics). Risk of marked bradycardia and hypotension in combination with calcium antagonists with negative inotropic effect (e.g., verapamil, diltiazem), especially in patients with an impaired ventricular function and/or conduction disorders. In case of change from a calcium antagonist to a beta-blocker or reverse, new intravenous therapy must not be initiated before at least 48 hours after withdrawal of the former treatment. Concomitant treatment with calcium antagonists which are dihydropyridine derivatives (e.g. nifedipine) may increase the risk of hypotension and may lead to heart failure in patients with latent cardial insufficiency. Digitalis glycosides in combination with beta blockers may increase the atrioventricular conduction time. Labetalol may enhance the digoxin’s effect of reducing ventricular rate. Beta-blockers, especially non-selective beta blockers, may increase the risk of hypoglycaemia in diabetic patients and mask the symptoms of hypoglycaemia, such as tachycardia and tremor, and delay the normalisation of blood sugar after insulin-induced hypoglycemia, especially non-selective beta blockers. Dose adjustments of oral antidiabetics and insulin may be necessary. Care should be taken at general anaesthesia of patients using beta blockers. Beta blockers reduce the risk of arrhythmias during anaesthesia , but may lead to reduction of the reflectoric tachycardia and increase the risk of hypotension during anaesthesia. As anaesthetic, an agent with as low as possible degree of negative inotropic effect should be used. Heart function must be closely monitored and bradycardia due to vagal dominance should be corrected by intravenous administration of atropine 1-2 mg intravenously (withdrawal prior to surgery, see section 4.2 Posology and method of administration). For withdrawal in patients using both beta blockers and clonidine, gradual discontinuation of the beta blocker must be done several days before discontinuation of clonidine. This is to reduce the potential rebound hypertensive crisis which is a consequence of withdrawal of clonidine. Accordingly, when changing from clonidine to a beta-blocker, it is important to discontinue clonidine gradually and start treatment with beta blocker several days after the clonidine has been withdrawn. Concomitant treatment with cholinesterase inhibitors can increase the risk of bradycardia. Concomitant treatment with stimulating adrenergics may increase the risk of increased blood pressure (e.g. phenylpropanolamine and adrenaline), while concomitant treatment with beta stimulating adrenergics results in a mutual reduced effect (antidote effect). Concomitant use of ergotamine derivatives may increase the risk of vasospastic reactions in some patients. Labetalol has been shown to increase the bioavailability of imipramine by more than 50% through the inhibition of its 2-hydroxylation. Labetalol in combination with imipramine may increase the effect of imipramine and concomitant use of tricyclic antidepressants. Concomitant use of tricyclic antidepressants may increase the incidence of tremor. Labetalol may enhance the hypotensive effect of volatile anaesthetics. Enhanced blood pressure reduction may occur in case of concomitant use of e.g. nitrates, antipsychotics (phenothiazine derivatives such as chloropromazine) and other antipsychotics, antidepressants.

שימוש לפי פנקס קופ''ח כללית 1994
Hypertensive crisis
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
