Quest for the right Drug
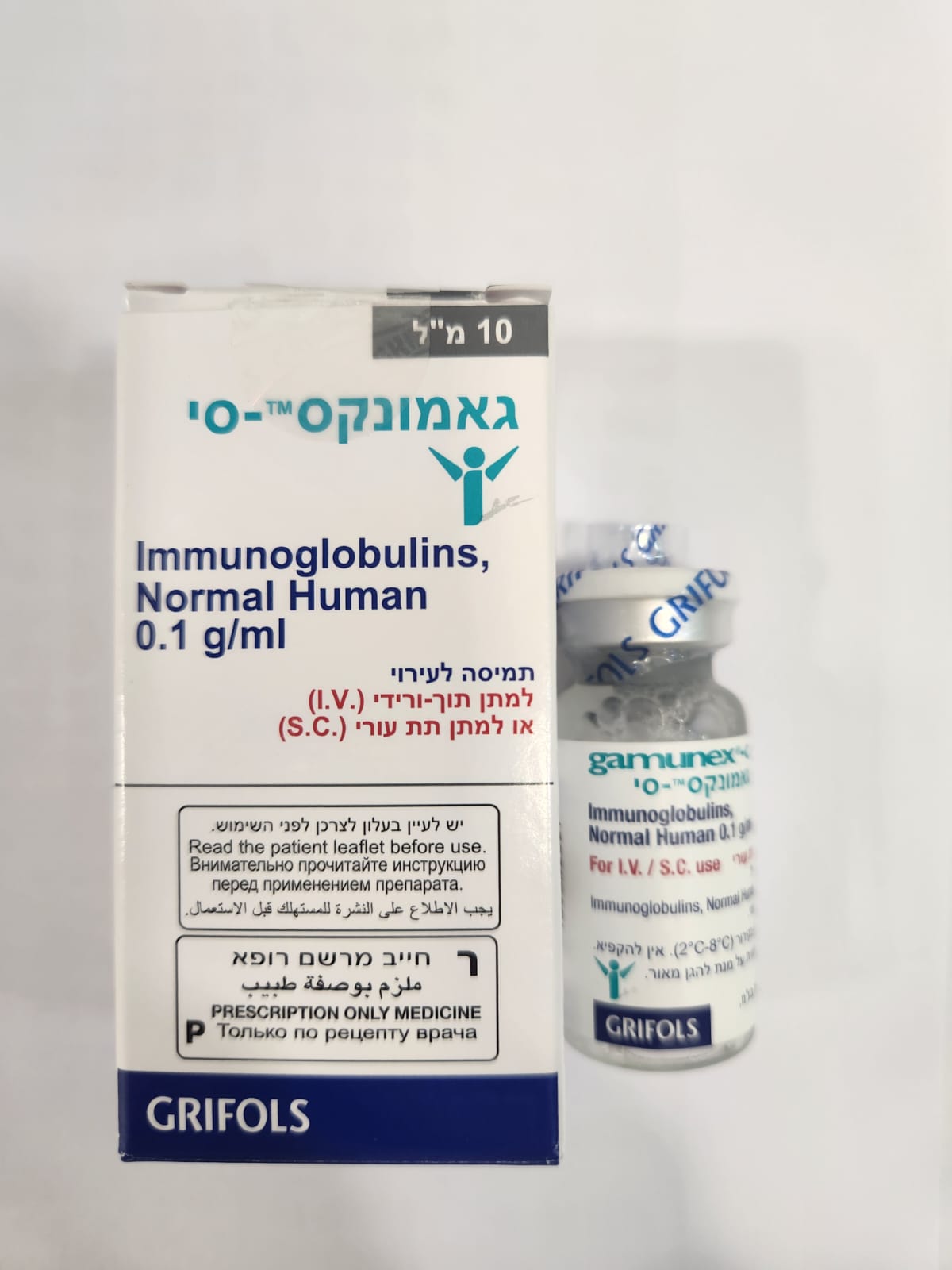
גאמונקס ® - סי GAMUNEX ® - C (IMMUNOGLOBULINS, NORMAL HUMAN)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי, תת-עורי : I.V, S.C
צורת מינון:
תמיסה לאינפוזיה : SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
5 WARNINGS AND PRECAUTIONS 5.1 Hypersensitivity Severe hypersensitivity reactions may occur with IGIV products, including GAMUNEX-C. In case of hypersensitivity, discontinue GAMUNEX-C infusion immediately and institute appropriate treatment. Have medications such as epinephrine available for immediate treatment of acute hypersensitivity reaction. GAMUNEX-C contains trace amounts of IgA (average 46 micrograms/mL). Patients with known antibodies to IgA may have a greater risk of developing potentially severe hypersensitivity and anaphylactic reactions. It is contraindicated in IgA deficient patients with antibodies against IgA and history of hypersensitivity reaction. (see Contraindications [4]) 5.2 Renal Failure Acute renal dysfunction/failure, acute tubular necrosis, proximal tubular nephropathy, osmotic nephrosis and death may occur upon use of IGIV products, especially those containing sucrose.7,8 GAMUNEX-C does not contain sucrose. Ensure that patients are not volume depleted prior to the initiation of the infusion of GAMUNEX-C. Periodic monitoring of renal function and urine output is particularly important in patients judged to have a potential increased risk for developing acute renal failure. Assess renal function, including measurement of blood urea nitrogen (BUN)/serum creatinine, prior to the initial infusion of GAMUNEX-C and again at appropriate intervals thereafter. If renal function deteriorates, consider discontinuation of GAMUNEX-C. For patients judged to be at risk for developing renal dysfunction, including patients with any degree of pre-existing renal insufficiency, diabetes mellitus, age greater than 65, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs, administer GAMUNEX-C at the minimum infusion rate practicable [less than 8 mg/kg/min (0.08 mL/kg/min)]. (see Dosage and Administration [2.5]) 5.3 Hyperproteinemia, Increased Serum Viscosity, and Hyponatremia Hyperproteinemia, increased serum viscosity and hyponatremia may occur in patients receiving IGIV treatment, including GAMUNEX-C. It is clinically critical to distinguish true hyponatremia from a pseudohyponatremia that is associated with concomitant decreased calculated serum osmolality or elevated osmolar gap, because treatment aimed at decreasing serum free water in patients with pseudohyponatremia may lead to volume depletion, a further increase in serum viscosity and a possible predisposition to thrombosis.9 5.4 Thrombosis Thrombosis may occur following treatment with immune globulin products, including GAMUNEX-C.10-12 Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors. Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies. For patients at risk of thrombosis, administer GAMUNEX-C at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity. (see Boxed Warning, Dosage and Administration [2.5]) 5.5 Aseptic Meningitis Syndrome (AMS) AMS may occur infrequently with IGIV treatment, including GAMUNEX-C. Discontinuation of IGIV treatment has resulted in remission of AMS within several days without sequelae. The syndrome usually begins within several hours to two days following IGIV treatment. AMS is characterized by the following symptoms and signs: severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, nausea and vomiting. Cerebrospinal fluid (CSF) studies are frequently positive with pleocytosis up to several thousand cells per cu mm, predominantly from the granulocytic series, and with elevated protein levels up to several hundred mg/dL, but negative culture results. Conduct a thorough neurological examination on patients exhibiting such symptoms and signs including CSF studies, to rule out other causes of meningitis. AMS may occur more frequently in association with high doses (2 g/kg) and/or rapid infusion of IGIV. 5.6 Hemolysis GAMUNEX-C may contain blood group antibodies which may act as hemolysins and induce in vivo coating of red blood cells (RBCs) with immunoglobulin, causing a positive direct antiglobulin reaction and, hemolysis.13-16 Delayed hemolytic anemia can develop subsequent to IGIV therapy due to enhanced RBC sequestration, and acute hemolysis consistent with intravascular hemolysis, has been reported. (see Adverse Reactions [6]) The following risk factors may be related to the development of hemolysis: high doses (e.g., ≥2 grams/kg, single administration or divided over several days) and non-O blood group.17 Underlying inflammatory state in an individual patient may increase the risk of hemolysis, but its role is uncertain.18 Closely monitor patients for clinical signs and symptoms of hemolysis (see Warnings and Precautions [5.11]), particularly patients with risk factors noted above and those with pre-existing anemia and/or cardiovascular or pulmonary compromise. Consider appropriate laboratory testing in higher risk patients, including measurement of hemoglobin or hematocrit prior to infusion and within approximately 36 hours and again 7 to 10 days post infusion. If clinical signs and symptoms of hemolysis or a significant drop in hemoglobin or hematocrit have been observed, perform additional confirmatory laboratory testing. If transfusion is indicated for patients who develop hemolysis with clinically compromising anemia after receiving IGIV, perform adequate cross-matching to avoid exacerbating on-going hemolysis. 5.7 Transfusion-related Acute Lung Injury (TRALI) Noncardiogenic pulmonary edema may occur in patients following treatment with IGIV products, including GAMUNEX-C.19 TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever. Symptoms typically occur within 1 to 6 hours after treatment. Monitor patients for pulmonary adverse reactions. If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil and anti-HLA antibodies in both the product and patient serum. TRALI may be managed using oxygen therapy with adequate ventilatory support. 5.8 Volume Overload The high dose regimen (1g/kg x 1-2 days) is not recommended for individuals with expanded fluid volumes or where fluid volume may be a concern. 5.9 Transmission of Infectious Agents Because GAMUNEX-C is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. No cases of transmission of viral diseases, vCJD or CJD have ever been identified for GAMUNEX-C. ALL infections suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider. 5.10 Hematoma Formation Do not administer GAMUNEX-C subcutaneously in patients with ITP because of the risk of hematoma formation. 5.11 Monitoring: Laboratory Tests • Periodic monitoring of renal function and urine output is particularly important in patients judged to be at increased risk of developing acute renal failure. Assess renal function, including measurement of BUN and serum creatinine, before the initial infusion of GAMUNEX-C and at appropriate intervals thereafter. • Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies, because of the potentially increased risk of thrombosis. • If signs and/or symptoms of hemolysis are present after an infusion of GAMUNEX-C, perform appropriate laboratory testing for confirmation. • If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil antibodies and anti-HLA antibodies in both the product and patient’s serum. 5.12 Interference with Laboratory Tests After infusion of IgG, the transitory rise of the various passively transferred antibodies in the patient’s blood may yield positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to erythrocyte antigens (e.g., A, B, and D) may cause a positive direct or indirect antiglobulin (Coombs) test. 6 ADVERSE REACTIONS PI: Intravenous: The most common adverse reactions observed at a rate ≥ 5% in subjects with intravenous treatment in the clinical trials were cough increased, rhinitis, pharyngitis, headache, asthma, nausea, fever, diarrhea, and sinusitis. PI: Subcutaneous: The most common adverse reactions observed at a rate ≥5% of subjects with subcutaneous treatment in the clinical trials were local infusion site reactions, fatigue, headache, upper respiratory tract infection, arthralgia, diarrhea, nausea, sinusitis, bronchitis, depression, allergic dermatitis, erythema, migraine, myalgia, viral infection, and pyrexia. ITP: The most common adverse reactions observed at a rate ≥ 5% in subjects in the clinical trials were headache, ecchymosis, vomiting, fever, nausea, rash, abdominal pain, back pain and dyspepsia. CIDP: The most common adverse reactions observed at a rate ≥ 5% in subjects in the clinical trial were headache, pyrexia, hypertension, chills, rash, nausea, arthralgia, and asthenia. 6.1 Clinical Trials Experience Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of one drug cannot be directly compared to rates in other clinical trials of another drug and may not reflect the rates observed in clinical practice. PI: Intravenous Administration The most serious adverse event observed in clinical study subjects receiving GAMUNEX-C IV for PI was an exacerbation of autoimmune pure red cell aplasia in one subject. In four different clinical trials to study PI, out of 157 subjects treated with GAMUNEX-C, 4 subjects discontinued due to the following adverse events: Coombs negative hypochromic anemia, autoimmune pure red cell aplasia, arthralgia/hyperhidrosis/fatigue/myalgia/nausea and migraine. In a study of 87 subjects, 9 subjects in each treatment group were pretreated with non-steroidal medication prior to infusion, such as diphenhydramine and acetaminophen. Table 2 lists the adverse reactions reported by at least 5% of subjects during the 9-month treatment. Table 2: Adverse Reactions Occurring in ≥ 5% of Subjects GAMUNEX®-C GAMIMUNE® N, 10% No. of subjects: 87 No. of subjects: 85 No. of subjects with adverse No. of subjects with adverse reaction (percentage of all reaction (percentage of all Adverse Reactions subjects) subjects) Cough increased 27 (31.0%) 25 (29.4%) Rhinitis 21 (24.1%) 24 (28.2%) Headache 13 (14.9%) 17 (20.0%) Pharyngitis 14 (16.1%) 16 (18.8%) Asthma 13 (14.9%) 10 (11.8%) Fever 6 (6.9%) 10 (11.8%) Nausea 10 (11.5%) 9 (10.6%) Diarrhea 6 (6.9%) 9 (10.6%) Sinusitis 5 (5.7%) 6 (7.1%) *An adverse reaction is an adverse event that meets any of the following 3 criteria: (a) that began during or within 72 hours of the end of product infusion, (b) that was considered at least possibly related by either the investigator or the applicant, and/or (c) whose causality assessment by the investigator was missing or indeterminate. Table 3 lists the frequency of adverse reactions (as defined for Table 2), which were reported by at least 5% of subjects. Table 3: Adverse Reactions Frequency GAMUNEX®-C GAMIMUNE® N, 10% No. of infusions: 825 No. of infusions: 865 Number (percentage of all Number (percentage of all Adverse Reactions infusions) infusions) Cough increased 40 (4.8%) 47 (5.4%) Rhinitis 34 (4.1%) 44 (5.1%) Headache 17 (2.1%) 24 (2.8%) Pharyngitis 20 (2.4%) 24 (2.8%) Fever 8 (1.0%) 20 (2.3%) Asthma 17 (2.1%) 12 (1.4%) Diarrhea 10 (1.2%) 10 (1.2%) Nausea 10 (1.2%) 10 (1.2%) Sinusitis 6 (0.7%) 7 (0.8%) The mean number of adverse reactions per infusion that occurred during or within 72 hours of the end of product infusion was 0.33 for the GAMUNEX-C and 0.39 for the GAMIMUNE® N, 10% [Immune Globulin Intravenous (Human), 10%] treatment group. In all three trials in primary humoral immunodeficiencies, the maximum infusion rate was 0.08 mL/kg/min (8 mg/kg/min). The infusion rate was reduced for 11 of 222 exposed subjects (7 GAMUNEX-C, 4 GAMIMUNE N, 10%) at 17 occasions. In most instances, mild to moderate hives/urticaria, itching, pain or reaction at infusion site, anxiety or headache was the main reason. There was one case of severe chills. There were no anaphylactic or anaphylactoid reactions to GAMUNEX-C or GAMIMUNE N, 10% in clinical trials. In the IV efficacy and safety study, serum samples were drawn to monitor the virus safety at baseline and one week after the first infusion of IGIV (for parvovirus B19), eight weeks after first and fifth infusion of IGIV (for hepatitis C, hepatitis B, and HIV-1), 16 weeks after the first and fifth infusion of IGIV (for hepatitis C) and at any time of premature discontinuation of the study (for hepatitis C, hepatitis B, HIV-1, and parvovirus B19). Viral markers of hepatitis C, hepatitis B, HIV-1, and parvovirus B19 were monitored by nucleic acid testing (NAT, Polymerase Chain Reaction [PCR]) and serological testing. There were no treatment-related emergent findings of virus transmission for either GAMUNEX-C or GAMIMUNE N, 10%. PI: Subcutaneous Administration (PK and Safety Study Adverse reactions were divided into 2 types: 1( Local infusion site reactions, and 2) Non-infusion site adverse reactions. Table 4 lists those adverse reactions (as defined for Table 2) occurring in ≥ 2% of infusions during the SC phase of the pharmacokinetic (PK) crossover and safety trial. [see Clinical Pharmacology (12.3)] Table 4: Most Frequent Adverse Reactions (≥ 2% of infusions) by Infusion in the SC Phase Adverse Reactions Number (Rate*) Non-infusion Site Adverse Reactions Headache 25 (0.03) Abdominal Pain 1 (<0.01) Local Infusion Site Reactions†, ‡ Mild 389 (0.54) Moderate 29 (0.04) Severe 9 (0.01) * Rate is calculated by the total number of events divided by the number of infusions received (725) † All local infusion site reactions were a priori considered drug-related. ‡ At each level of summation (Preferred Term), local infusion site reactions are counted only once if they occur at the same infusion visit. Mild – usually transient in nature and generally not interfering with normal activities. Moderate – sufficiently discomforting to interfere with normal activities. Severe – prevents normal activities. Table 5 lists the adverse reactions occurring in ≥ 5% of subjects and the frequency of adverse reactions (as defined for Table 2) per infusion. Table 5: Most Frequent Adverse Reactions (≥ 5% of subjects) by Subject and Infusion in the SC phase No. of Adverse No. of Subjects Reactions Adverse Reaction n=32 (%) (Rate*) Local Infusion Site Reaction†,‡ 24 (75.0%) 427 (0.59) Fatigue 5 (15.6%) 6 (0.01) Headache 4 (12.5%) 25 (0.03) Upper respiratory tract infection 4 (12.5%) 5 (0.01) Arthralgia 3 (9.4%) 6 (0.01) Diarrhea 3 (9.4%) 6 (0.01) Nausea 3 (9.4%) 4 (0.01) Sinusitis 3 (9.4%) 4 (0.01) Bronchitis 2 (6.3%) 2 (<0.01) Depression 2 (6.3%) 2 (<0.01) Dermatitis allergic 2 (6.3%) 2 (<0.01) Erythema 2 (6.3%) 2 (<0.01) Migraine 2 (6.3%) 2 (<0.01) Myalgia 2 (6.3%) 2 (<0.01) Pyrexia 2 (6.3%) 2 (<0.01) Viral infection 2 (6.3%) 2 (<0.01) * Rate is calculated by the total number of events divided by the number of infusions received (725) † All local infusion site reactions were a priori considered drug-related ‡ At each level of summation (Preferred Term), infusion site reactions are counted only once if they occur at the same infusion visit. There were no serious bacterial infections in the SC phase of the PK and safety trial. Local Infusion Site Reactions Local infusion site reactions with SC GAMUNEX-C consisted of erythema, pain and swelling. The majority of local infusion site reactions resolved within 3 days. The number of subjects experiencing an infusion site reaction and the number of infusion site reactions decreased over time as subjects received continued weekly SC infusions. At the beginning of the SC phase (week 1), a rate of approximately 1 infusion site reaction per infusion was reported, whereas at the end of the study (week 24) this rate was reduced to 0.5 infusion site reactions per infusion, a reduction of 50%. ITP In two different clinical trials to study ITP, out of 76 subjects treated with GAMUNEX-C, 2 subjects discontinued due to the following adverse reactions: Hives and Headache/Fever/Vomiting. One subject, a 10-year-old boy, died suddenly from myocarditis 50 days after his second infusion of GAMUNEX-C. The death was judged to be unrelated to GAMUNEX-C. No pre-medication with corticosteroids was permitted by the protocol. Twelve ITP subjects treated in each treatment group were pretreated with medication prior to infusion. Generally, diphenhydramine and/or acetaminophen were used. More than 90% of the observed drug-related adverse events were of mild to moderate severity and of transient nature. The infusion rate was reduced for 4 of the 97 exposed subjects (1 GAMUNEX-C, 3 GAMIMUNE N, 10%) on 4 occasions. Mild to moderate headache, nausea, and fever were the reported reasons. Table 6 lists the adverse reactions (as defined for Table 2) reported by at least 5% of subjects during the 3-month efficacy and safety study. Table 6: Adverse Reactions Occurring in ≥ 5% of Subjects GAMUNEX®-C GAMIMUNE® N, 10% No. of subjects: 48 No. of subjects: 49 Number Number Adverse Reaction (percentage of all subjects) (percentage of all subjects) Headache 25 (52.1%) 26 (53.1%) Vomiting 6 (12.5%) 8 (16.3%) Ecchymosis 7 (14.6%) 2 (4.1%) Fever 6 (12.5%) 6 (12.2%) Nausea 6 (12.5%) 5 (10.2%) Rash 4 (8.3%) 0 Abdominal pain 3 (6.3%) 3 (6.1%) Back pain 3 (6.3%) 2 (4.1%) Dyspepsia 3 (6.3%) 0 Asthenia 2 (4.2%) 3 (6.1%) Dizziness 2 (4.2%) 3 (6.1%) Serum samples were drawn to monitor the virus safety of the ITP subjects at baseline, nine days after the first infusion (for parvovirus B19), and 3 months after the first infusion of IGIV and at any time of premature discontinuation of the study. Viral markers of hepatitis C, hepatitis B, HIV-1, and parvovirus B19 were monitored by nucleic acid testing (NAT, PCR), and serological testing. There were no treatment-related emergent findings of virus transmission for either GAMUNEX®-C, or GAMIMUNE® N, 10%. CIDP In the CIDP efficacy and safety study, 113 subjects were exposed to GAMUNEX-C and 95 were exposed to Placebo. (see Clinical Studies [14]) As a result of the study design, the drug exposure with GAMUNEX- C was almost twice that of Placebo, with 1096 GAMUNEX-C infusions versus 575 Placebo infusions. Therefore, adverse reactions are reported per infusion (represented as frequency) to correct for differences in drug exposure between the 2 groups. The majority of loading-doses were administered over 2 days. The majority of maintenance-doses were administered over 1 day. Infusions were administered in the mean over 2.7 hours. Table 7 shows the numbers of subjects per treatment group in the CIDP clinical trial, and the reason for discontinuation due to adverse events: Table 7: Reasons for Discontinuation Due to Adverse Events: Number of Subjects Number of Subjects Discontinued due to Adverse Adverse Event Events Urticaria, Dyspnea, GAMUNEX®-C 113 3 (2.7%) Bronchopneumonia Cerebrovascular Accident, Placebo 95 2 (2.1%) Deep Vein Thrombosis The most common adverse reactions with GAMUNEX-C were headache and pyrexia. Table 8 lists adverse reactions (as defined for Table 2) reported by at least 5% of subjects in any treatment group. Table 8: Adverse Reactions Occurring in ≥ 5% of Subjects GAMUNEX®-C Placebo No. of subjects: 113 No. of subjects: 95 MedDRA No. of No. of No. of No. of Preferred term a Incidence Incidence Subjects Adverse b Subjects Adverse Density Density b (%) Reactions (%) Reactions 35 Headache 50 0.046 7 (7.4%) 9 0.016 (31.0%) 15 Pyrexia 27 0.025 0 0 (13.3%) 10 Hypertension 19 0.017 3 (3.2%) 3 0.005 (8.8%) Chills 9 (8.0%) 10 0.009 0 0 Nausea 7 (6.2%) 9 0.008 3 (3.2%) 3 0.005 Rash 7 (6.2%) 10 0.009 1 (1.1%) 1 0.002 Arthralgia 6 (5.3%) 7 0.006 0 0 1 Asthenia 6 (5.3%) 6 0.005 2 0.003 (1.1%) a Reported in ≥5% of subjects in any treatment group. b Calculated by the total number of adverse reactions divided by the number of infusions received (1096 for GAMUNEX-C and 575 for Placebo). The most serious adverse reaction observed in clinical study subjects receiving GAMUNEX-C for CIDP was pulmonary embolism (PE) in one subject with a history of PE. Laboratory Abnormalities During the course of the clinical program, ALT and AST elevations were identified in some subjects. • For ALT, in the IV PI study treatment emergent elevations above the upper limit of normal were transient and observed among 14/80 (18%) of subjects in the GAMUNEX-C group versus 5/88 (6%) of subjects in the GAMIMUNE N, 10% group (p = 0.026). • In the SC PI study treatment emergent laboratory abnormalities during the SC phase occurred in several subjects. Four subjects (4/32, 13%) had elevated Alkaline Phosphatase. One subject (1/32, 3%) had an elevated ALT and three subjects (3/32, 9%) had an elevated AST. No elevations were >1.6 times the upper limit of normal. • In the ITP study which employed a higher dose per infusion, but a maximum of only two infusions, the reverse finding for elevation of ALT was observed among 3/44 (7%) of subjects in the GAMUNEX-C group versus 8/43 (19%) of subjects in the GAMIMUNE N, 10% group (p = 0.118). • In the CIDP study, 15/113 (13%) of subjects in the GAMUNEX-C group and 7/95 (7%) in the Placebo group (p=0.168) had a treatment emergent transient elevation of ALT. Elevations of ALT and AST were generally mild (<3 times upper limit of normal), transient, and were not associated with obvious symptoms of liver dysfunction. GAMUNEX-C may contain low levels of anti-Blood Group A and B antibodies primarily of the IgG4 class. Direct antiglobulin tests (DAT or direct Coombs tests), which are carried out in some centers as a safety check prior to red blood cell transfusions, may become positive temporarily. There were 2 cases of hemolytic anemia across these clinical trials. One hemolytic event not associated with positive DAT findings was observed in the IV PI study in a woman with common variable immune deficiency and B12 deficiency (pernicious anemia) at a dose of 450 mg/kg. The other hemolytic event occurred in the CIDP study in a subject with positive DAT at a dose of 1g/kg. 6.2 Postmarketing Experience Because adverse reactions are voluntarily reported post-approval from a population of uncertain size, it is not always possible to reliably estimate their frequencies or establish a causal relationship to product exposure. The following adverse reactions have been identified during post-approval use of IGIV products8,20 including GAMUNEX-C: • Infusion Reactions: Hypersensitivity (e.g., anaphylaxis), tachycardia, malaise, flushing, or other skin reactions, chest discomfort, rigors, and changes in blood pressure • Renal: Acute renal dysfunction/failure, osmotic nephropathy • Respiratory: Apnea, Acute Respiratory Distress Syndrome (ARDS), TRALI, cyanosis, hypoxemia, pulmonary edema, bronchospasm • Cardiovascular: Cardiac arrest, thromboembolism, vascular collapse, hypotension • Neurological: Coma, loss of consciousness, seizures/convulsions, tremor, aseptic meningitis • Integumentary: Stevens-Johnson syndrome, epidermolysis, erythema multiforme, dermatitis (e.g., bullous dermatitis) • Hematologic: Pancytopenia, leukopenia, hemolysis, hemolytic anemia, positive direct antiglobulin (Coombs test) • General/Body as a Whole: Rigors • Gastrointestinal: Hepatic dysfunction Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il. Additionally, you can also report to Padagis via the following address: Padagis.co.il.
Effects on Driving

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול במקרים האלה: א. חסר חיסוני ראשוני (חולים עם פגיעה ראשונית בייצור נוגדנים כגון אגמגלובולינמיה או היפוגמגלובוילינמיה, ITP (Idiopathic thrombocytopenic purpura)); ב. חסר חיסוני ספציפי, מניעה או טיפול בחצבת, הפטיטיס A ויראלית; ג. CIDP – Chronic inflammatory demyelineating polyneuropathy; ד.טיפול בחולי לוקמיה מסוג CLL הסובלים מהיפוגלמגלובולינמיה משנית חמורה וזיהומים חוזרים.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| טיפול בחולי לוקמיה מסוג CLL הסובלים מהיפוגלמגלובולינמיה משנית חמורה וזיהומים חוזרים. | ||||
| CIDP – Chronic inflammatory demyelineating polyneuropathy; | ||||
| חסר חיסוני ספציפי, מניעה או טיפול בחצבת, הפטיטיס A ויראלית | ||||
| חסר חיסוני ראשוני (חולים עם פגיעה ראשונית בייצור נוגדנים כגון אגמגלובולינמיה או היפוגמגלובולינמיה, ITP (Idiopathic thrombocytopenic purpura)); |
שימוש לפי פנקס קופ''ח כללית 1994
Primary immunodeficiency (patients with primary defective antibody synthesis such as agammaglobulinemia or hypogammaglobulinemia, idiopathic thrombocytopenic purpura (ITP)
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה מוגבלת לשימוש בבתי חולים או אשפוז יום
מידע נוסף
