Quest for the right Drug
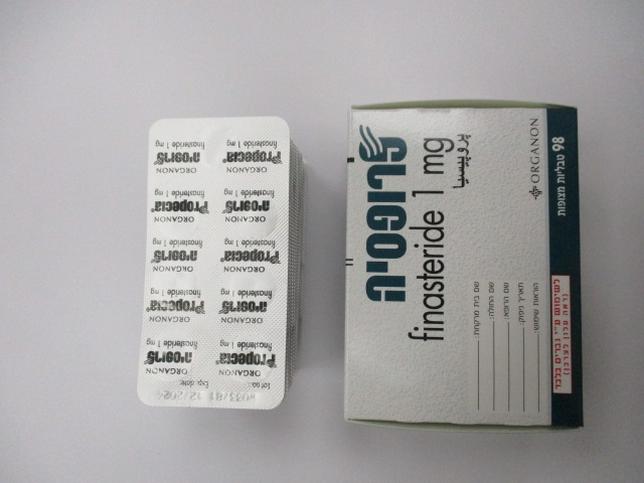
פרופסיה PROPECIA (FINASTERIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: 5α-reductase inhibitor. ATC code D11AX10 Mechanism of action Finasteride is a competitive and specific inhibitor of type II 5-reductase. Finasteride has no affinity for the androgen receptor and has no androgenic, anti-androgenic, oestrogenic, anti-oestrogenic, or progestational effects. Inhibition of this enzyme blocks the peripheral conversion of testosterone to the androgen DHT, resulting in significant decreases in serum and tissue DHT concentrations. Finasteride produces a rapid reduction in serum DHT concentration, reaching significant suppression within 24 hours of dosing. Hair follicles contain type II 5-reductase. In men with male pattern hair loss, the balding scalp contains miniaturised hair follicles and increased amounts of DHT. Administration of finasteride decreases scalp and serum DHT concentrations in these men. Men with a genetic deficiency of type II 5-reductase do not suffer from male pattern hair loss. Finasteride inhibits a process responsible for miniaturisation of the scalp hair follicles, which can lead to reversal of the balding process. Clinical efficacy and safety Studies in men Clinical studies were conducted in 1879 men aged 18 to 41 with mild to moderate, but not complete, vertex hair loss and/or frontal/mid-area hair loss. In the two studies in men with vertex hair loss (n=1553), 290 men completed 5 years of treatment with Propecia vs. 16 patients on placebo. In these two studies, efficacy was assessed by the following methods: (i) hair count in a representative 5.1cm2 area of scalp, (ii) patient self assessment questionnaire, (iii) investigator assessment using a seven point scale, and (iv) photographic assessment of standardised paired photographs by a blinded expert panel of dermatologists using a seven point scale. In these 5- year studies men treated with ‘Propecia’ improved compared to both baseline and placebo beginning as early as 3 months, as determined by both the patient and investigator assessments of efficacy. With regard to hair count, the primary endpoint in these studies, increases compared to baseline were demonstrated starting at 6 months (the earliest time point assessed) through to the end of the study. In men treated with ‘Propecia’ these increases were greatest at 2 years and gradually declined thereafter to the end of 5 years; whereas hair loss in the placebo group progressively worsened compared to baseline over the entire 5 year period. In ‘Propecia’ treated patients, a mean increase from baseline of 88 hairs [p <0.01; 95% CI (77.9, 97.80; n=433] in the representative 5.1 cm2 area was observed at 2 years and an increase from baseline of 38 hairs [p <0.01; 95% CI (20.8, 55.6); n=219] was observed at 5 years, compared with a decrease from baseline of 50 hairs [p <0.01; 95% CI (-80.5, -20.6);n=47] at 2 years and a decrease from baseline of 239 hairs [p <0.01; 95% CI (-304.4, -173.4); n=15] at 5 years in patients who received placebo. Standardised photographic assessment of efficacy demonstrated that 48% of men treated with finasteride for 5 years were rated as improved, and an additional 42% were rated as unchanged. This is in comparison to 25% of men treated with placebo for 5 years who were rated as improved or unchanged. These data demonstrate that treatment with ‘Propecia’ for 5 years resulted in a stabilisation of the hair loss that occurred in men treated with placebo. An additional 48-week, placebo-controlled study designed to assess the effect of ‘Propecia’ on the phases of the hair-growth cycle (growing phase [anagen] and resting phase [telogen]) in vertex baldness enrolled 212 men with androgenetic alopecia. At baseline and 48 weeks, total, anagen and telogen hair counts were obtained in a 1-cm2 target area of the scalp. Treatment with ‘Propecia’ led to improvements in anagen hair counts, while men in the placebo group lost anagen hair. At 48 weeks, men treated with ‘Propecia’ showed net increases in total and anagen hair counts of 17 hairs and 27 hairs, respectively, compared to placebo. This increase in anagen hair count, compared to total hair count, led to a net improvement in the anagen-to-telogen ratio of 47% at 48 weeks for men treated with ‘Propecia’, compared to placebo. These data provide direct evidence that treatment with ‘Propecia’ promotes the conversion of hair follicles into the actively growing phase. Studies in women Lack of efficacy was demonstrated in post-menopausal women with androgenetic alopecia who were treated with ‘Propecia’ in a 12 month, placebo-controlled study (n=137). These women did not show any improvement in hair count, patient self- assessment, investigator assessment, or ratings based on standardised photographs, compared with the placebo group.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption Relative to an intravenous reference dose, the oral bioavailability of finasteride is approximately 80%. The bioavailability is not affected by food. Maximum finasteride plasma concentrations are reached approximately two hours after dosing and the absorption is complete after six to eight hours. Distribution Protein binding is approximately 93%. The volume of distribution of finasteride is approximately 76 litres. At steady state following dosing with 1 mg/day, maximum finasteride plasma concentration averaged 9.2 ng/ml and was reached 1 to 2 hours post-dose; AUC (0-24 hr) was 53 ng•hr/ml. Finasteride has been recovered in the cerebrospinal fluid (CSF), but the drug does not appear to concentrate preferentially to the CSF. A small amount of finasteride has also been detected in the seminal fluid of subjects receiving the drug. Biotransformation Finasteride is metabolised primarily via the cytochrome P450 3A4 enzyme subfamily. Following an oral dose of 14C-finasteride in man, two metabolites of the drug were identified that possess only a small fraction of the 5-reductase inhibitory activity of finasteride. Elimination Following an oral dose of 14C-finasteride in man, 39% of the dose was excreted in the urine in the form of metabolites (virtually no unchanged drug was excreted in the urine) and 57% of total dose was excreted in the faeces. Plasma clearance is approximately 165 ml/min. The elimination rate of finasteride decreases somewhat with age. Mean terminal half- life is approximately 5-6 hours in men 18-60 years of age and 8 hours in men more than 70 years of age. These findings are of no clinical significance and hence, a reduction in dosage in the elderly is not warranted. Renal impairment No adjustment in dosage is necessary in non-dialysed patients with renal impairment.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| לטיפול בהגדלה שפירה של הערמונית. | אורולוגיה | DUTASTERIDE, FINASTERIDE | BPH |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
12.01.21 - עלון לצרכן אנגלית 12.01.21 - עלון לצרכן עברית 12.01.21 - עלון לצרכן ערבית 09.03.24 - עלון לצרכן עברית 03.04.24 - עלון לצרכן אנגלית 03.04.24 - עלון לצרכן ערבית 24.06.12 - החמרה לעלון 26.05.13 - החמרה לעלון 07.04.14 - החמרה לעלון 19.08.20 - החמרה לעלון 20.03.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
פרופסיה