Quest for the right Drug
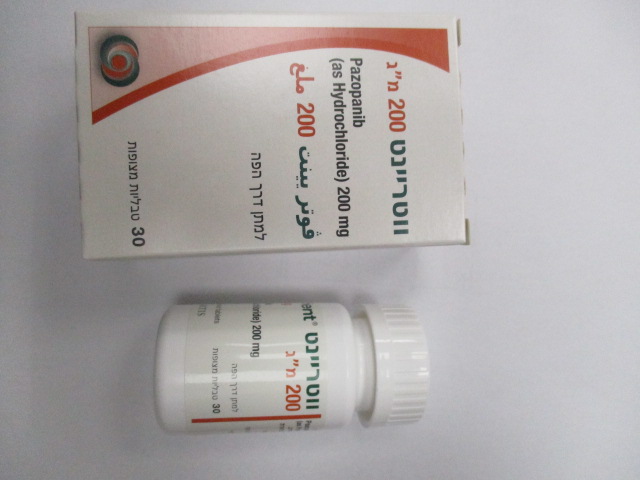
ווטריינט 200 מ"ג VOTRIENT 200 MG (PAZOPANIB AS HYDROCHLORIDE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Hepatic effects Cases of hepatic failure (including fatalities) have been reported during use of pazopanib. Administration of pazopanib to patients with mild or moderate hepatic impairment should be undertaken with caution and close monitoring. 800 mg pazopanib once daily is the recommended dose in patients with mild abnormalities in serum liver tests (either normal bilirubin and any degree of ALT elevation or elevation of bilirubin up to 1.5 x ULN regardless of the ALT value). A reduced pazopanib dose of 200 mg once daily is recommended in patients with moderate hepatic impairment (elevation of bilirubin >1.5 to 3 x ULN regardless of the ALT value) (see sections 4.2 and 5.2). Pazopanib is not recommended in patients with severe hepatic impairment (total bilirubin >3 x ULN regardless of the ALT value) (see sections 4.2 and 5.2). Exposure at a 200 mg dose is markedly reduced, though highly variable, in these patients, with values considered insufficient to obtain a clinically relevant effect. In clinical studies with pazopanib, increase in serum transaminases (ALT, aspartate aminotransferase [AST]) and bilirubin were observed (see section 4.8). In the majority of the cases, isolated increases in ALT and AST have been reported, without concomitant elevations of alkaline phosphatase or bilirubin. Patients over 60 years of age may be at greater risk for mild (>3 x ULN) to severe (>8 x ULN) elevation of ALT. Patients who carry the HLA-B*57:01 allele have an increased risk of pazopanib- associated ALT elevations. Liver function should be monitored in all subjects receiving pazopanib, regardless of genotype or age (see section 5.1). Serum liver tests should be performed before initiation of treatment with pazopanib, at weeks 3, 5, 7 and 9, then at months 3 and 4, with additional tests as clinically indicated. Periodic testing should then continue after month 4. See Table 1 for dose modification guidance for patients with baseline values of total bilirubin ≤1.5 x ULN and AST and ALT ≤2 x ULN: Table 1 Dose modifications for drug-induced hepatotoxicity Liver test values Dose modification Transaminase elevation Continue on pazopanib with weekly monitoring of liver function until between 3 and 8 x ULN transaminases return to Grade 1 or baseline. Transaminase elevation of Interrupt pazopanib until transaminases return to Grade 1 or baseline. >8 x ULN If the potential benefit of reinitiating pazopanib treatment is considered to outweigh the risk for hepatotoxicity, then reintroduce pazopanib at a reduced dose of 400 mg daily and perform serum liver tests weekly for 8 weeks. Following reintroduction of pazopanib, if transaminase elevations >3 x ULN recur, then pazopanib should be permanently discontinued. Transaminase elevations Permanently discontinue pazopanib. >3 x ULN concurrently with Patients should be monitored until return to Grade 1 or baseline. Pazopanib bilirubin elevations >2 x ULN is a UGT1A1 inhibitor. Mild, indirect (unconjugated) hyperbilirubinaemia may occur in patients with Gilbert’s syndrome. Patients with only a mild indirect hyperbilirubinaemia, known or suspected Gilbert’s syndrome, and elevation in ALT >3 x ULN should be managed as per the recommendations outlined for isolated ALT elevations. Concomitant use of pazopanib and simvastatin increases the risk of ALT elevations (see section 4.5) and should be undertaken with caution and close monitoring. Hypertension In clinical studies with pazopanib, events of hypertension including newly diagnosed symptomatic episodes of elevated blood pressure (hypertensive crisis) have occurred. Blood pressure should be well controlled prior to initiating pazopanib. Patients should be monitored for hypertension early after starting treatment (no VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 longer than one week after starting pazopanib) and frequently thereafter to ensure blood pressure control. Elevated blood pressure levels (systolic blood pressure ≥150 mm Hg or diastolic blood pressure ≥100 mm Hg) occurred early in the course of treatment (approximately 40% of cases occurred by day 9 and approximately 90% of cases occurred in the first 18 weeks). Blood pressure should be monitored and managed promptly using a combination of anti-hypertensive therapy and dose modification of pazopanib (interruption and re-initiation at a reduced dose based on clinical judgement) (see sections 4.2 and 4.8). Pazopanib should be discontinued if there is evidence of hypertensive crisis or if hypertension is severe and persists despite anti-hypertensive therapy and pazopanib dose reduction. Posterior reversible encephalopathy syndrome (PRES)/Reversible posterior leukoencephalopathy syndrome (RPLS) PRES/RPLS has been reported in association with pazopanib. PRES/RPLS can present with headache, hypertension, seizure, lethargy, confusion, blindness and other visual and neurological disturbances, and can be fatal. Patients developing PRES/RPLS should permanently discontinue treatment with pazopanib. Interstitial lung disease (ILD)/Pneumonitis ILD, which can be fatal, has been reported in association with pazopanib (see section 4.8). Patients should be monitored for pulmonary symptoms indicative of ILD/pneumonitis and pazopanib should be discontinued in patients developing ILD or pneumonitis. Cardiac dysfunction/Heart failure The risks and benefits of pazopanib should be considered before beginning therapy in patients who have pre- existing cardiac dysfunction. The safety and pharmacokinetics of pazopanib in patients with moderate to severe heart failure or those with a below normal left ventricular ejection fraction (LVEF) have not been studied. In clinical studies with pazopanib, events of cardiac dysfunction such as congestive heart failure and decreased LVEF have occurred (see section 4.8). In a randomised study comparing pazopanib and sunitinib in RCC (VEG108844), subjects had baseline and follow up LVEF measurements. Myocardial dysfunction occurred in 13% (47/362) of subjects in the pazopanib arm compared to 11% (42/369) of subjects in the sunitinib arm. Congestive heart failure was observed in 0.5% of subjects in each treatment arm. Congestive heart failure was reported in 3 out of 240 subjects (1%) in the Phase III VEG110727 STS study. Decreases in LVEF in subjects who had post-baseline and follow-up LVEF measurement were detected in 11% (15/140) in the pazopanib arm, compared with 3% (1/39) in the placebo arm. Risk factors Thirteen of the 15 subjects in the pazopanib arm of the STS Phase III study had concurrent hypertension which may have exacerbated cardiac dysfunction in patients at risk by increasing cardiac after-load. 99% of patients (243/246) enrolled in the STS Phase III study, including the 15 subjects, received anthracycline. Prior anthracycline therapy may be a risk factor for cardiac dysfunction. Outcome Four of the 15 subjects had full recovery (within 5% of baseline) and 5 had partial recovery (within the normal range, but >5% below baseline). One subject did not recover and follow-up data were not available for the other 5 subjects. Management Interruption of pazopanib and/or dose reduction should be combined with treatment of hypertension (if present, refer to hypertension warning section above) in patients with significant reductions in LVEF, as clinically indicated. Patients should be carefully monitored for clinical signs or symptoms of congestive heart failure. Baseline and periodic evaluation of LVEF is recommended in patients at risk of cardiac dysfunction. VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 QT prolongation and torsade de pointes In clinical studies with pazopanib, events of QT prolongation and torsade de pointes have occurred (see section 4.8). Pazopanib should be used with caution in patients with a history of QT interval prolongation, in patients taking antiarrhythmics or other medicinal products that may prolong QT interval and in patients with relevant pre-existing cardiac disease. When using pazopanib, baseline and periodic monitoring of electrocardiograms and maintenance of electrolytes (e.g. calcium, magnesium, potassium) within normal range is recommended. Arterial thrombotic events In clinical studies with pazopanib, myocardial infarction, myocardial ischaemia, ischaemic stroke and transient ischaemic attack were observed (see section 4.8). Fatal events have been observed. Pazopanib should be used with caution in patients who are at increased risk of thrombotic events or who have had a history of thrombotic events. Pazopanib has not been studied in patients who have had an event within the previous 6 months. A treatment decision should be made based on the assessment of individual patient’s benefit/risk. Venous thromboembolic events In clinical studies with pazopanib, venous thromboembolic events including venous thrombosis and fatal pulmonary embolus have occurred. While observed in both RCC and STS studies, the incidence was higher in the STS population (5%) than in the RCC population (2%). Thrombotic microangiopathy (TMA) TMA has been reported in clinical studies of pazopanib as monotherapy, in combination with bevacizumab, and in combination with topotecan (see section 4.8). Patients developing TMA should permanently discontinue treatment with pazopanib. Reversal of effects of TMA has been observed after treatment was discontinued. Pazopanib is not indicated for use in combination with other agents. Haemorrhagic events In clinical studies with pazopanib haemorrhagic events have been reported (see section 4.8). Fatal haemorragic events have occurred. Pazopanib has not been studied in patients who had a history of haemoptysis, cerebral haemorrhage or clinically significant gastrointestinal (GI) haemorrhage in the past 6 months. Pazopanib should be used with caution in patients with significant risk of haemorrhage. Aneurysms and artery dissections The use of VEGF pathway inhibitors in patients with or without hypertension may promote the formation of aneurysm and/or artery dissections. Before initiating pazopanib, this risk should be carefully considered in patients with risk factors such as hypertension or history of aneurysm. Gastrointestinal (GI) perforations and fistula In clinical studies with pazopanib, events of GI perforation or fistula have occurred (see section 4.8). Fatal perforation events have occurred. Pazopanib should be used with caution in patients at risk for GI perforation or fistula. Wound healing No formal studies of the effect of pazopanib on wound healing have been conducted. Since vascular endothelial growth factor (VEGF) inhibitors may impair wound healing, treatment with pazopanib should be stopped at least 7 days prior to scheduled surgery. The decision to resume pazopanib after surgery should be based on clinical judgement of adequate wound healing. Pazopanib should be discontinued in patients with VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 wound dehiscence. Hypothyroidism In clinical studies with pazopanib, events of hypothyroidism have occurred (see section 4.8). Baseline laboratory measurement of thyroid function is recommended and patients with hypothyroidism should be treated as per standard medical practice prior to the start of pazopanib treatment. All patients should be observed closely for signs and symptoms of thyroid dysfunction on pazopanib treatment. Laboratory monitoring of thyroid function should be performed periodically and managed as per standard medical practice. Proteinuria In clinical studies with pazopanib, proteinuria has been reported. Baseline and periodic urinanalysis during treatment is recommended and patients should be monitored for worsening proteinuria. Pazopanib should be discontinued if the patient develops nephrotic syndrome. Tumour lysis syndrome (TLS) The occurrence of TLS, including fatal TLS, has been associated with the use of pazopanib (see section 4.8). Patients at increased risk of TLS are those with rapidly growing tumours, a high tumour burden, renal dysfunction, or dehydration. Preventative measures, such as treatment of high uric acid levels and intravenous hydration, should be considered prior to initiation of Votrient. Patients at risk should be closely monitored and treated as clinically indicated. Pneumothorax In clinical studies with pazopanib in advanced soft tissue sarcoma, events of pneumothorax have occurred (see section 4.8). Patients on pazopanib treatment should be observed closely for signs and symptoms of pneumothorax. Infections Cases of serious infections (with or without neutropenia), in some cases with fatal outcome, have been reported. Combination with other systemic anti-cancer therapies Clinical studies of pazopanib in combination with a number of other anti-cancer therapies (including for example pemetrexed, lapatinib or pembrolizumab were terminated early due to concerns over increased toxicity and/or mortality, and a safe and effective combination dose has not been established with these regimens. Pregnancy Pre-clinical studies in animals have shown reproductive toxicity (see section 5.3). If pazopanib is used during pregnancy, or if the patient becomes pregnant whilst receiving pazopanib, the potential hazard to the foetus should be explained to the patient. Women of childbearing potential should be advised to avoid becoming pregnant while receiving treatment with pazopanib (see section 4.6). Interactions Concomitant treatment with strong inhibitors of CYP3A4, P-glycoprotein (P-gp) or breast cancer resistance protein (BCRP) should be avoided due to risk of increased exposure to pazopanib (see section 4.5). Selection of alternative concomitant medicinal products with no or minimal potential to inhibit CYP3A4, P-gp or BCRP should be considered. VOT SPI Jan22 V3 EU SmPC 12-Nov-2021 Concomitant treatment with inducers of CYP3A4 should be avoided due to risk of decreased exposure to pazopanib (see section 4.5). Cases of hyperglycaemia have been observed during concomitant treatment with ketoconazole. Concomitant administration of pazopanib with uridine diphosphate glucuronosyl transferase 1A1 (UGT1A1) substrates (e.g. irinotecan) should be undertaken with caution since pazopanib is an inhibitor of UGT1A1 (see section 4.5). Grapefruit juice should be avoided during treatment with pazopanib (see section 4.5).
Effects on Driving
4.7 Effects on ability to drive and use machines Votrient has no or negligible influence on the ability to drive and use machines. A detrimental effect on such activities cannot be predicted from the pharmacology of pazopanib. The clinical status of the patient and the adverse event profile of pazopanib should be borne in mind when considering the patients ability to perform tasks that require judgement, motor or cognitive skills. Patients should avoid driving or using machines if they feel dizzy, tired or weak.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). 2. קו טיפול מתקדם (שני והלאה) בסרקומה מתקדמת של הרקמות הרכות מסוג סרקומה פיברובלסטית, סרקומה פיברוהיסטיוציטית, ליומיוסרקומה, סרקומה סינוביאלית, MPNST, NOS, סרקומה וסקולארית, malignant glomus tumors ב. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה או מומחה באורולוגיה המטפל באורולוגיה אונקולוגית.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| קו טיפול מתקדם (שני והלאה) בסרקומה מתקדמת של הרקמות הרכות מסוג סרקומה פיברובלסטית, סרקומה פיברוהיסטיוציטית, ליומיוסרקומה, סרקומה סינוביאלית, MPNST, NOS, סרקומה וסקולארית, malignant glomus tumors | 09/01/2013 | אונקולוגיה | Soft tissue sarcoma | |
| לטיפול בסרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). במהלך מחלתו יהיה החולה זכאי לטיפול בשתי תרופות בלבד מהתרופות המפורטות להלן - Sunitinib, Sorafenib, Everolimus, Temsirolimus, Pazopanib | 23/01/2011 | אונקולוגיה | Renal cell carcinoma | |
| סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). | 30/01/2020 | אונקולוגיה | Renal cell carcinoma | |
| סרטן כליה מתקדם או גרורתי (גם כקו טיפול ראשון). במהלך מחלתו יהיה החולה זכאי לטיפול בשלוש תרופות בלבד מהתרופות המפורטות להלן - Sunitinib, Sorafenib, Everolimus, Temsirolimus, Pazopanib, Axitinib, Nivolumab. הטיפול בתכשיר לא יינתן בשילוב עם Nivolumab או עם תרופה ממשפחת מעכבי mTOR. | 12/01/2017 | אונקולוגיה | Renal cell carcinoma |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
23/01/2011
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לרופא
15.03.22 - עלון לרופאעלון מידע לצרכן
08.05.16 - עלון לצרכן 20.04.22 - עלון לצרכן אנגלית 20.04.22 - עלון לצרכן עברית 20.04.22 - עלון לצרכן ערבית 18.07.23 - עלון לצרכן עברית 07.09.23 - עלון לצרכן אנגלית 07.09.23 - עלון לצרכן ערבית 27.09.24 - עלון לצרכן אנגלית 27.09.24 - עלון לצרכן עברית 27.09.24 - עלון לצרכן ערבית 18.11.12 - החמרה לעלון 21.08.13 - החמרה לעלון 26.03.14 - החמרה לעלון 29.03.15 - החמרה לעלון 06.07.15 - החמרה לעלון 02.03.16 - החמרה לעלון 15.03.17 - החמרה לעלון 27.02.20 - החמרה לעלון 20.08.20 - החמרה לעלון 01.11.21 - החמרה לעלון 16.12.21 - החמרה לעלון 15.03.22 - החמרה לעלון 18.07.23 - החמרה לעלון 27.09.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ווטריינט 200 מ"ג