Quest for the right Drug
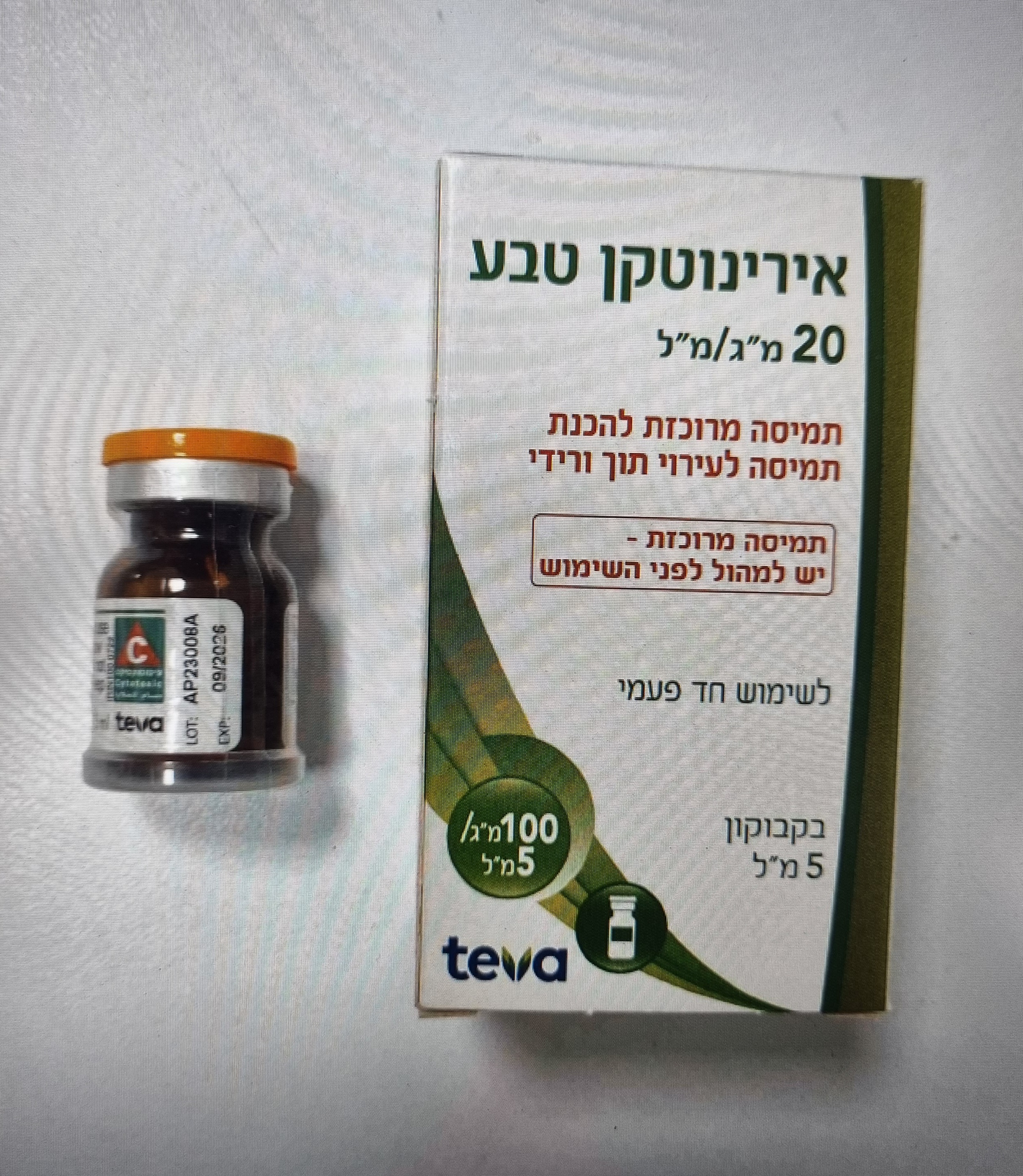
אירינוטקן טבע IRINOTECAN TEVA (IRINOTECAN HYDROCHLORIDE TRIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
4.8 Undesirable effects CLINICAL STUDIES Adverse reaction data have been extensively collected from studies in metastatic colorectal cancer; the frequencies are presented below. The adverse reactions for other indications are expected to be similar to those for colorectal cancer. The most common (≥1/10), dose-limiting adverse reactions of irinotecan are delayed diarrhea (occurring more than 24 hours after administration) and blood disorders including neutropenia, anaemia and thrombocytopenia. Neutropenia is a dose-limiting toxic effect. Neutropenia was reversible and not cumulative; the median day to nadir was 8 days whatever the use in monotherapy or in combination therapy. Very commonly severe transient acute cholinergic syndrome was observed. The main symptoms were defined as early diarrhoea and various other symptoms such as abdominal pain, sweating, myosis and increased salivation occurring during or within the first 24 hours after the infusion of irinotecan. These symptoms disappear after atropine administration (see section 4.4). MONOTHERAPY The following adverse reactions considered to be possibly or probably related to the administration of irinotecan have been reported from 765 patients at the recommended dose of 350 mg/m² in monotherapy. Within each frequency grouping, adverse reactions are presented in order of decreasing seriousness. Frequencies are defined as: Very Common (≥ 1/10), Common (≥ 1/100 to < 1/10), Uncommon (≥ 1/1,000 to < 1/100), Rare (≥ 1/10,000 to < 1/1,000), Very Rare (< 1/10,000). Adverse Reactions Reported with Irinotecan in Monotherapy (350 mg/m2 every 3 weeks schedule) MedDRA System Organ Class Frequency Category Preferred Term Infections and infestations Common Infection Very common Neutropenia Very common Anaemia Blood and lymphatic system disorders Common Thrombocytopenia Common Febrile neutropenia Metabolism and nutrition disorders Very common Decreased appetite Nervous system disorders Very common Cholinergic syndrome Very common Diarrhea Very common Vomiting Gastrointestinal disorders Very common Nausea Very common Abdominal pain Common Constipation Skin and subcutaneous tissue disorders Very common Alopecia (reversible) Very common Mucosal inflammation General disorders and administration site Very common Pyrexia conditions Very common Asthenia Common Blood creatinine increased Common Transaminases (ALT and AST) Investigations increased Common Blood bilirubin increased Common Blood alkaline phosphatase increased Description of selected adverse reactions (monotherapy) Severe diarrhoea was observed in 20 % of patients who follow recommendations for the management of diarrhoea. Of the evaluable cycles, 14 % have severe diarrhoea. The median time of onset of the first liquid stool was on day 5 after the infusion of irinotecan. Nausea and vomiting were severe in approximately 10 % of patients treated with antiemetics. Constipation has been observed in less than 10% of patients. Neutropenia was observed in 78.7 % of patients and was severe (neutrophil count < 500 cells/mm3) in 22.6 % of patients. Of the evaluable cycles, 18 % had a neutrophil count below 1,000 cells/mm³ including 7.6 % with a neutrophil count < 500 cells/mm³. Total recovery was usually reached by day 22. Febrile neutropenia was reported in 6.2 % of patients and in 1.7 % of cycles. Infections occurred in about 10.3 % of patients (2.5 % of cycles) and were associated with severe neutropenia in about 5.3 % of patients (1.1 % of cycles), and resulted in death in 2 cases. Anaemia was reported in about 58.7 % of patients (8% with haemoglobin < 8 g/dl and 0.9% with haemoglobin < 6.5 g/dl). Thrombocytopenia (< 100,000 cells/mm³) was observed in 7.4% of patients and 1.8 % of cycles with 0.9% with platelet count ≤ 50,000 cells/mm3 and 0.2% of cycles. Nearly all the patients showed a recovery by day 22. Acute cholinergic syndrome Severe transient acute cholinergic syndrome was observed in 9% of patients treated in monotherapy. Asthenia was severe in less than 10% of patients treated in monotherapy. The causal relationship to irinotecan has not been clearly established. Pyrexia in the absence of infection and without concomitant severe neutropenia, occurred in 12 % of patients treated in monotherapy. Laboratory tests Transient and mild to moderate increases in serum levels of either transaminases, alkaline phosphatase or bilirubin were observed in 9.2 %, 8.1 % and 1.8 % of the patients, respectively, in the absence of progressive liver metastasis. Transient and mild to moderate increases of serum levels of creatinine have been observed in 7.3 % of the patients. COMBINATION THERAPY Adverse reactions detailed in this section refer to irinotecan. Irinotecan has been studied in combination with 5FU and FA for metastatic colorectal cancer. Safety data of adverse reactions from clinical studies demonstrate very commonly observed NCI Grade 3 or 4 possibly or probably-related adverse events in the blood and the lymphatic system disorders, gastrointestinal disorders, and skin and subcutaneous tissue disorders MedDRA System Organ Classes. The following adverse reactions considered to be possibly or probably related to the administration of irinotecan have been reported from 145 patients treated by irinotecan in combination therapy with 5FU/FA in every 2 weeks schedule at the recommended dose of 180 mg/m². Adverse Reactions Reported with Irinotecan in Combination Therapy (180 mg/m2 every 2 weeks schedule) MedDRA System Organ Class Frequency Category Preferred Term Infections and infestations Common Infection Very common Thrombocytopenia Blood and lymphatic system Very common Neutropenia disorders Very common Anaemia Common Febrile neutropenia Metabolism and nutrition Very common Decreased appetite disorders Nervous system disorders Very common Cholinergic syndrome Very common Diarrhea Very common Vomiting Gastrointestinal disorders Very common Nausea Common Abdominal pain Common Constipation Skin and subcutaneous tissue Very common Alopecia (reversible) disorders Very common Mucosal inflammation General disorders and Very common Asthenia administration site conditions Common Pyrexia Transaminases (ALT and AST) Very common increased Investigations Very common Blood bilirubin increased Blood alkaline phosphatase Very common increased Description of selected adverse reactions (combination therapy) Severe diarrhoea was observed in 13.1 % of patients who follow recommendations for the management of diarrhoea. Of the evaluable cycles, 3.9 % have a severe diarrhoea. A lower incidence of severe nausea and vomiting was observed (2.1 % and 2.8 % of patients respectively). Constipation relative to irinotecan and/or loperamide has been observed in 3.4 % of patients. Neutropenia was observed in 82.5 % of patients and was severe (neutrophil count < 500 cells/mm3) in 9.8 % of patients. Of the evaluable cycles, 67.3 % had a neutrophil count below 1,000 cells/mm³ including 2.7 % with a neutrophil count < 500 cells/mm³. Total recovery was usually reached within 7-8 days. Febrile neutropenia was reported in 3.4 % of patients and in 0.9 % of cycles. Infections occurred in about 2% of patients (0.5% of cycles) and were associated with severe neutropenia in about 2.1% of patients (0.5% of cycles), and resulted in death in 1 case. Anaemia was reported in 97.2% of patients (2.1% with haemoglobin < 8 g/dl). Thrombocytopenia (< 100,000 cells/mm³) was observed in 32.6 % of patients and 21.8 % of cycles. No severe thrombocytopenia (< 50,000 cells/mm³) has been observed. Acute cholinergic syndrome Severe transient acute cholinergic syndrome was observed in 1.4 % of patients treated in combination therapy. Asthenia was severe in 6.2 % of patients treated in combination therapy. The causal relationship to irinotecan has not been clearly established. Pyrexia in the absence of infection and without concomitant severe neutropenia, occurred in 6.2 % of patients treated in combination therapy. Laboratory tests Transient serum levels (Grades 1 and 2) of either SGPT, SGOT, alkaline phosphatase or bilirubin were observed in 15%, 11%, 11% and 10% of the patients, respectively, in the absence of progressive liver metastasis. Transient Grade 3 were observed in 0%, 0%, 0% and 1% of the patients, respectively. No Grade 4 was observed. Increases of amylase and/or lipase have been very rarely reported. Rare cases of hypokalaemia and hyponatremia mostly related with diarrhea and vomiting have been reported. OTHER ADVERSE EVENTS REPORTED IN CLINICAL STUDIES WITH THE WEEKLY REGIMEN FOR IRINOTECAN The following additional drug-related events have been reported in clinical studies with irinotecan: pain, sepsis, anorectal disorder, GI candida infection, hypomagnesamia, rash, skin signs, gait disturbance, confusion, headache, syncope, flushing, bradycardia, urinary tract infection, breast pain, gamma-glutamyltransferase, extravasation, and tumour lysis syndrome, cardiovascular disorders (angina pectoris, cardiac arrest, myocardial infarction, myocardial ischaemia, peripheral vascular disorder, vascular disorder), and thromboembolic events (arterial thrombosis, cerebral infarction, cerebrovascular accident, deep vein thrombosis, peripheral embolism , pulmonary embolism, thrombophlebitis, thrombosis, and sudden death) (see section 4.4.). POST-MARKETING SURVEILLANCE Frequencies from post-marketing surveillance are not known (cannot be estimated from available data). MedDRA System Organ Class Preferred Term Infections and infestations • Pseudomembranous colitis one of which has been documented bacteriologically (Clostridium difficile) • Sepsis • Fungal infections1 • Viral infections2 Blood and lymphatic system disorders • Thrombocytopenia with antiplatelet antibodies Immune system disorders • Hypersensitivity • Anaphylactic reaction Metabolism and nutrition disorders • Dehydration (due to diarrhoea and vomiting) • Hypovolaemia Nervous system disorders • Speech disorder generally transient in nature, in some cases, the event was attributed to the cholinergic syndrome observed during or shortly after infusion of irinotecan • Paraesthesia • Muscular contractions involuntary • Hypertension (during or after infusion) Cardiac disorders • Cardio circulatory failure3 Vascular disorders • Hypotension3 Respiratory, thoracic and mediastinal • Interstitial lung disease presenting as lung infiltration is disorders uncommon during irinotecan therapy; early effects such as dyspnoea have been reported (see section 4.4) • Dyspnoea (see section 4.4) • Hiccups Gastrointestinal disorders • Intestinal obstruction • Ileus: cases of ileus without preceding colitis have also been reported • Megacolon • Gastrointestinal haemorrhage • Colitis; in some cases, colitis was complicated by ulceration, bleeding, ileus, or infection • Typhlitis • Colitis ischaemic • Colitis ulcerative • Symptomatic or asymptomatic pancreatic enzymes incraesed • Intestinal perforation • Steatohepatitis Hepatobiliary disorders • Hepatic steatosis Skin and subcutaneous tissue • Skin reaction disorders Musculoskeletal and connective • Cramps tissue disorders • Renal impairment and acute renal failure generally in Renal and urinary disorders patients who become infected and/or volume depleted from severe gastrointestinal toxicities3 • Renal insufficiency3 General disorders and administration site conditions • Infusion site reaction Investigations • Amylase increased • Lipase increased • Hypokalaemia • Hyponatraemia mostly related with diarrhea and vomiting • Transaminases increased (i.e., AST and ALT) in the absence of progressive liver metastasis have been very rarely reported 1 e.g. Pneumocystis jirovecii pneumonia, bronchopulmonary aspergillosis, systemic Candida. 2 e.g. Herpes zoster, influenza, hepatitis B reactivation, cytomegalovirus colitis. 3 Infrequent cases of renal insufficiency, hypotension or cardio circulatory failure have been observed in patients who experienced episodes of dehydration associated with diarrhea and/or vomiting, or sepsis. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form: https://sideeffects.health.gov.il

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול במקרים האלה: א. סרטן מעי גס מתקדם (גם כטיפול ראשון). ב. סרטן החלחולת לטיפול בחזרה מקומית של המחלה. ג. סרטן לבלב גרורתי כקו טיפול ראשון.2. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| סרטן מעי גס מתקדם (גם כטיפול ראשון). | 16/12/1997 | |||
| סרטן לבלב גרורתי כקו טיפול ראשון. | 16/12/1997 | |||
| סרטן החלחולת לטיפול בחזרה מקומית של המחלה. | 16/12/1997 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/12/1997
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
