Quest for the right Drug
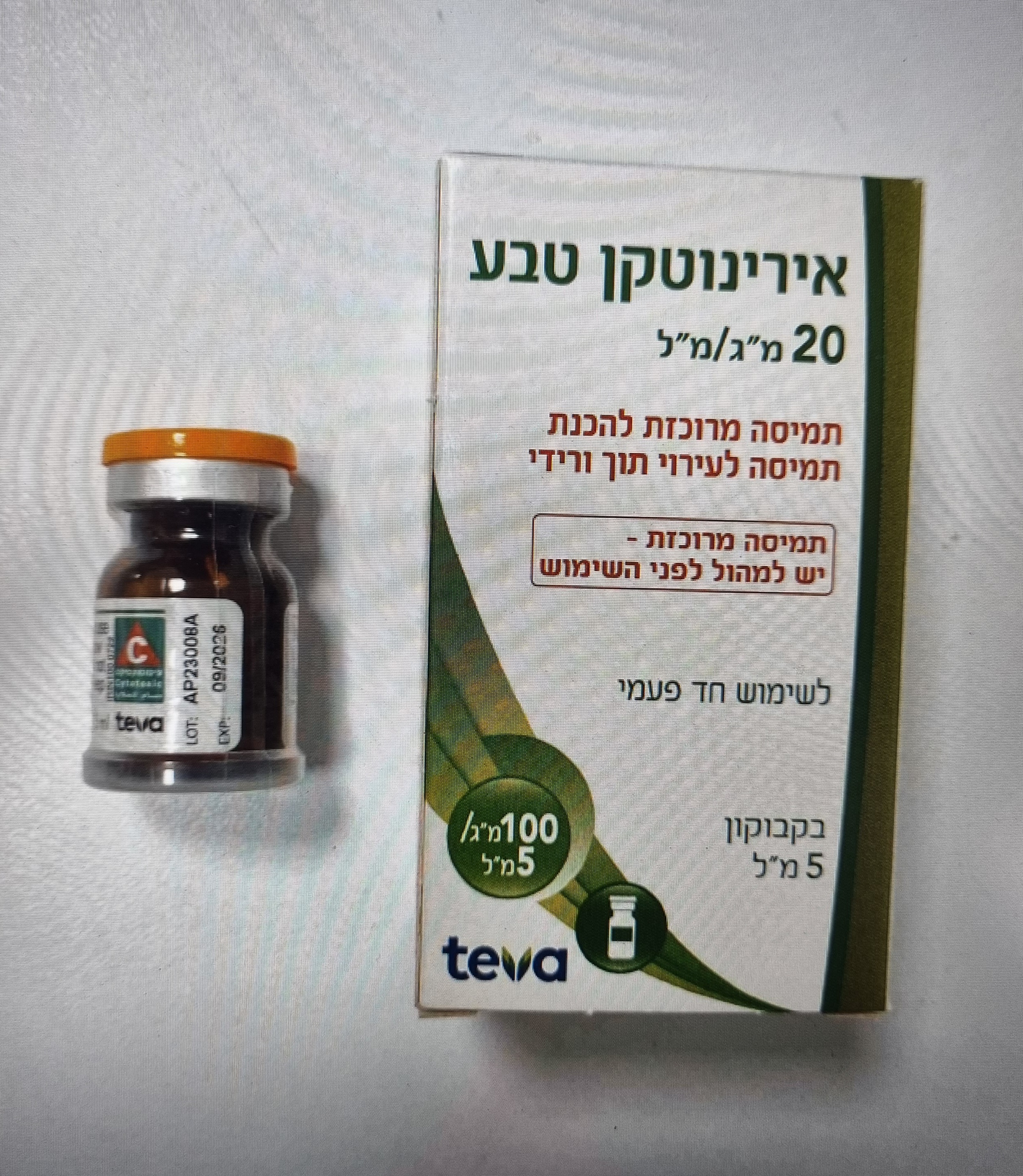
אירינוטקן טבע IRINOTECAN TEVA (IRINOTECAN HYDROCHLORIDE TRIHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use The use of Irinotecan Teva should be confined to units specialised in the administration of cytotoxic chemotherapy and it should only be administered under the supervision of a physician qualified in the use of anticancer chemotherapy. Given the nature and incidence of adverse events, Irinotecan Teva will only be prescribed in the following cases after the expected benefits have been weighted against the possible therapeutic risks: • in patients presenting a risk factor, particularly those with a WHO performance status = 2. • in the few rare instances where patients are deemed unlikely to observe recommendations regarding management of adverse events (need for immediate and prolonged antidiarrheal treatment combined with high fluid intake at onset of delayed diarrhoea). Strict hospital supervision is recommended for such patients. When Irinotecan Teva is used in monotherapy, it is usually prescribed with the every-3-week-dosage schedule. However, the weekly-dosage schedule (see section 5) may be considered in patients who may need a closer follow-up or who are at particular risk of severe neutropenia. Delayed diarrhoea Patients should be made aware of the risk of delayed diarrhoea occurring more than 24 hours after the administration of Irinotecan Teva and at any time before the next cycle. In monotherapy, the median time of onset of the first liquid stool was on day 5 after the infusion of Irinotecan Teva. Patients should quickly inform their physician of its occurrence and start appropriate therapy immediately. Patients with an increased risk of diarrhoea are those who had a previous abdominal/pelvic radiotherapy, those with baseline hyperleucocytosis, those with performance status ≥ 2 and women. If not properly treated, diarrhoea can be life-threatening, especially if the patient is concomitantly neutropenic. As soon as the first liquid stool occurs, the patient should start drinking large volumes of beverages containing electrolytes and an appropriate antidiarrheal therapy must be initiated immediately. This antidiarrheal treatment will be prescribed by the department where Irinotecan Teva has been administered. After discharge from the hospital, the patients should obtain the prescribed medicinal products so that they can treat the diarrhoea as soon as it occurs. In addition, they must inform their physician or the department administering Irinotecan Teva when/if diarrhoea is occurring. The currently recommended antidiarrheal treatment consists of high doses of loperamide (4 mg for the first intake and then 2 mg every 2 hours). This therapy should continue for 12 hours after the last liquid stool and should not be modified. In no instance should loperamide be administered for more than 48 consecutive hours at these doses, because of the risk of paralytic ileus, nor for less than 12 hours. In addition to the antidiarrheal treatment, a prophylactic broad-spectrum antibiotic should be given, when diarrhoea is associated with severe neutropenia (neutrophil count < 500 cells/mm³). In addition to the antibiotic treatment, hospitalisation is recommended for management of the diarrhoea, in the following cases: - Diarrhoea associated with fever, - Severe diarrhoea (requiring intravenous hydration), - Diarrhoea persisting beyond 48 hours following the initiation of high-dose loperamide therapy. Loperamide should not be given prophylactically, even in patients who experienced delayed diarrhoea at previous cycles. In patients who experienced severe diarrhoea, a reduction in dose is recommended for subsequent cycles (see section 4.2). Haematology In clinical studies, the frequency of NCI CTC Grade 3 and 4 neutropenia has been significantly higher in patients who received previous pelvic/abdominal irradiation than in those who had not received such irradiation. Patients with baseline serum total bilirubin levels of 1.0 mg/dL or more have also had a significantly greater likelihood of experiencing first-cycle Grade 3 or 4 neutropenia than those with bilirubin levels that were less than 1.0 mg/dL. Weekly monitoring of complete blood cell counts is recommended during Irinotecan Teva treatment. Patients should be aware of the risk of neutropenia and the significance of fever. Febrile neutropenia (temperature > 38°C and neutrophil count ≤ 1,000 cells/mm³) should be urgently treated in the hospital with broad-spectrum intravenous antibiotics. In patients who experienced severe haematological events, a dose reduction is recommended for subsequent administration (see section 4.2). There is an increased risk of infections and haematological toxicity in patients with severe diarrhoea. In patients with severe diarrhoea, complete blood cell counts should be performed Patients with reduced UGT1A1 activity Patients that are UGT1A1 poor metabolisers, such as patients with Gilbert’s syndrome (e.g. homozygous for UGT1A1*28 or *6 variants) are at increased risk for severe neutropenia and diarrhoea following irinotecan treatment. This risk increases with the irinotecan dose level. Although a precise dose reduction in starting dose has not been established, a reduced irinotecan starting dose should be considered for patients that are UGT1A1 poor metabolisers, especially patients who are administered doses > 180 mg/m2 or frail patients. Consideration should be given to applicable clinical guidelines for dose recommendations in this patient population. Subsequent doses may be increased based on individual patient tolerance to treatment. UGT1A1 genotyping can be used to identify patients at increased risk of severe neutropenia and diarrhoea, however the clinical utility of pre-treatment genotyping is uncertain, since UGT1A1 polymorphism does not account for all the toxicity seen from irinotecan therapy (see section 5.2). Liver impairment Liver function tests should be performed at baseline and before each cycle. Weekly monitoring of complete blood counts should be conducted in patients with bilirubin ranging from 1.5 to 3 times the ULN, due to decrease of the clearance of irinotecan (see section 5.2) and thus increasing the risk of hematotoxicity in this population. For patients with a bilirubin > 3 times the ULN (see section 4.3). Nausea and vomiting A prophylactic treatment with antiemetics is recommended before each treatment with Irinotecan Teva. Nausea and vomiting have been frequently reported. Patients with vomiting associated with delayed diarrhoea should be hospitalised as soon as possible for treatment. Acute cholinergic syndrome If acute cholinergic syndrome appears (defined as early diarrhoea and various other signs and symptoms such as sweating, abdominal cramping, myosis and salivation), atropine sulphate (0.25 mg subcutaneously) should be administered unless clinically contraindicated (see section 4.8). These symptoms may be observed during or shortly after infusion of irinotecan, are thought to be related to the anticholinesterase activity of the irinotecan parent compound, and are expected to occur more frequently with higher irinotecan doses. Caution should be exercised in patients with asthma. In patients who experienced an acute and severe cholinergic syndrome, the use of prophylactic atropine sulphate is recommended with subsequent doses of irinotecan. Respiratory disorders Interstitial lung disease presenting as lung infiltration is uncommon during irinotecan therapy. Interstitial lung disease can be fatal. Risk factors possibly associated with the development of interstitial lung disease include the use of pneumotoxic medicinal products, radiation therapy and colony stimulating factors. Patients with risk factors should be closely monitored for respiratory symptoms before and during irinotecan therapy. Extravasation While irinotecan is not a known vesicant, care should be taken to avoid extravasation and the infusion site should be monitored for signs of inflammation. Should extravasation occur, flushing the site and application of ice is recommended. Elderly Due to the greater frequency of decreased biological functions, in particular hepatic function, in elderly patients, dose selection with irinotecan should be cautious in this population (see section 4.2). Chronic inflammatory bowel disease and/or bowel obstruction Patients must not be treated with irinotecan until resolution of the bowel obstruction (see section 4.3). Renal function Increases in serum creatinine or blood urea nitrogen have been observed. There have been cases of acute renal failure. These events have generally been attributed to complications of infection or to dehydration related to nausea, vomiting, or diarrhoea. Rare instances of renal dysfunction due to tumour lysis syndrome have also been reported. Irradiation therapy Patients who have previously received pelvic/abdominal irradiation are at increased risk of myelosuppression following the administration of irinotecan. Physicians should use caution in treating patients with extensive prior irradiation (e.g.,>25% of bone marrow irradiated and within 6 weeks prior to start of treatment with irinotecan). Dosing adjustment may apply to this population (see section 4.2). Cardiac disorders Myocardial ischaemic events have been observed following irinotecan therapy predominately in patients with underlying cardiac disease, other known risk factors for cardiac disease, or previous cytotoxic chemotherapy (see section 4.8). Consequently, patients with known risk factors should be closely monitored, and action should be taken to try to minimize all modifiable risk factors (e.g., smoking, hypertension, and hyperlipidaemia). Vascular disorders Irinotecan has been rarely associated with thromboembolic events (pulmonary embolism, venous thrombosis, and arterial thromboembolism) in patients presenting with multiple risk factors in addition to the underlying neoplasm. Others Concomitant administration of irinotecan with a strong inhibitor (e.g., ketoconazole) or inducer (e.g., rifampicin, carbamazepine, phenobarbital, phenytoin, apalutamide) of CYP3A4 may alter the metabolism of irinotecan and should be avoided (see section 4.5). Infrequent cases of renal insufficiency, hypotension or circulatory failure have been observed in patients who experienced episodes of dehydration associated with diarrhoea and/or vomiting, or sepsis. Contraception in women of childbearing potential / men: Due to the potential for genotoxicity, advise female patients of reproductive potential to use highly effective contraception during treatment and for 6 months after the last dose of irinotecan. Due to the potential for genotoxicity, advise male patients with female partners of reproductive potential to use effective contraception during treatment and for 3 months after the last dose of irinotecan (see section 4.6). Breast-feeding Due to the potential for adverse reactions in nursing infants, breast-feeding should be discontinued for the duration of Irinotecan Teva therapy (see sections 4.3 and 4.6). Sorbitol This medicine contains sorbitol (see section 2). Sorbitol is a source of fructose. Patients with hereditary fructose intolerance (HFI) must not be given this medicine unless strictly necessary. Babies and young children (below 2 years of age) may not yet be diagnosed with hereditary fructose intolerance (HFI). Medicines (containing sorbitol/fructose) given intravenously may be life-threatening and should be contraindicated in this population unless there is an overwhelming clinical need and no alternatives are available. A detailed history with regard to HFI symptoms has to be taken of each patient prior to being given this medicinal product. Sodium This medicine contains less than 1mmol sodium (23 mg) per dose that is to say essentially ‘sodium free’.
Effects on Driving
4.7 Effects on ability to drive and use machines Irinotecan has moderate influence on the ability to drive and use machines. Patients should be warned about the potential for dizziness or visual disturbances which may occur within 24 hours following the administration of Irinotecan Teva, and advised not to drive or operate machinery if these symptoms occur.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול במקרים האלה: א. סרטן מעי גס מתקדם (גם כטיפול ראשון). ב. סרטן החלחולת לטיפול בחזרה מקומית של המחלה. ג. סרטן לבלב גרורתי כקו טיפול ראשון.2. מתן התרופה האמורה ייעשה לפי מרשם של רופא מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| סרטן מעי גס מתקדם (גם כטיפול ראשון). | 16/12/1997 | |||
| סרטן לבלב גרורתי כקו טיפול ראשון. | 16/12/1997 | |||
| סרטן החלחולת לטיפול בחזרה מקומית של המחלה. | 16/12/1997 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
16/12/1997
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
