Quest for the right Drug
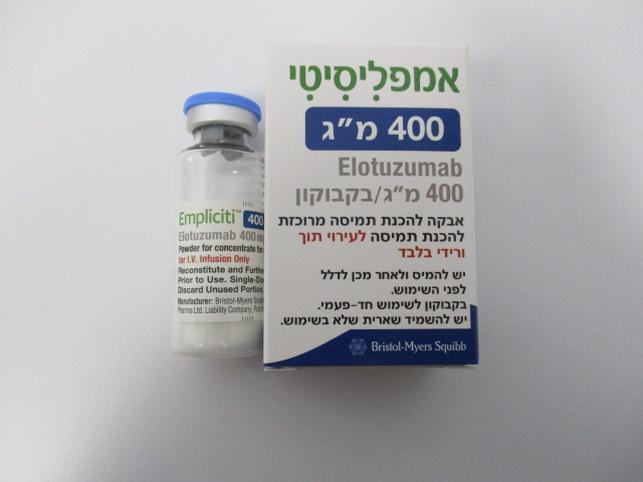
אמפליסיטי 400 מ"ג EMPLICITI 400 MG (ELOTUZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
אבקה להכנת תמיסה מרוכזת לעירוי : POWDER FOR CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antineoplastic agents, monoclonal antibodies and antibody drug conjugates, other monoclonal antibodies and antibody drug conjugates. ATC code: L01FX08. Mechanism of action Elotuzumab is an immunostimulatory humanised, IgG1 monoclonal antibody that specifically targets the signaling lymphocyte activation molecule family member 7 (SLAMF7) protein. SLAMF7 is highly expressed on multiple myeloma cells independent of cytogenetic abnormalities. SLAMF7 is also expressed on natural killer cells (NK), normal plasma cells, and other immune cells including some T cell subsets, monocytes, B cells, macrophages, and pDCs (plasmacytoid dendritic cells), but is not detected on normal solid tissues or haematopoietic stem cells. Elotuzumab directly activates natural killer cells through both the SLAMF7 pathway and Fc receptors enhancing anti-myeloma activity in vitro. Elotuzumab also targets SLAMF7 on myeloma cells and through interactions with Fc receptors on specific immune cells, promotes the killing of myeloma cells through NK cell-mediated antibody-dependent cellular cytotoxicity (ADCC) and macrophage-mediated antibody-dependant cellular phagocytosis (ADCP). In nonclinical models, elotuzumab has demonstrated synergistic activity when combined with lenalidomide, pomalidomide or bortezomib. Clinical efficacy and safety Empliciti in combination with lenalidomide and dexamethasone (CA204004) CA204004 is a randomised, open-label study was conducted to evaluate the efficacy and safety of Empliciti in combination with lenalidomide and dexamethasone (E-Ld) in patients with multiple myeloma who have received one to three prior therapies. All patients had documented progression following their most recent therapy. Patients who were refractory to lenalidomide were excluded and 6% of patients had prior lenalidomide treatment. Patients had to recover after transplant for a minimum of 12 weeks from autologous stem cell transplant (SCT), and 16 weeks from allogeneic SCT. Patients with cardiac amyloidosis or plasma cell leukemia were excluded from this study. Eligible patients were randomised in a 1:1 ratio to receive either Empliciti in combination with lenalidomide and dexamethasone or lenalidomide and dexamethasone (Ld). Treatment was administered in 4-week cycles until disease progression or unacceptable toxicity. Elotuzumab 10 mg/kg bw was administered intravenously each week for the first 2 cycles and every 2 weeks thereafter. Prior to Empliciti infusion, dexamethasone was administered as a divided dose: an oral dose of 28 mg and an intravenous dose of 8 mg. In the control group and on weeks without Empliciti, dexamethasone 40 mg was administered as a single oral dose weekly. Lenalidomide 25 mg was taken orally once daily for the first 3 weeks of each cycle. Assessment of tumour response was conducted every 4 weeks. A total of 646 patients were randomised to receive treatment: 321 to Empliciti in combination with lenalidomide and dexamethasone and 325 to lenalidomide and dexamethasone. Demographics and baseline characteristics were well balanced between treatment arms. The median age was 66 years (range 37 to 91); 57% of patients were older than 65 years; 60% of patients were male; Whites comprised 84% of the study population, Asians 10%, and blacks 4%. The International Staging System (ISS) Stage was I in 43%, II in 32% and III in 21% of patients. The high risk cytogenetic categories of del17p and t(4;14) were present in 32% and 9% of patients, respectively. The median number of prior therapies was 2. Thirty-five percent (35%) of patients were refractory (progression during or within 60 days of last therapy) and 65% were relapsed (progression after 60 days of last therapy). Prior therapies included: stem cell transplant (55%), bortezomib (70%) melphalan (65%), thalidomide (48%), and lenalidomide (6%). The primary endpoints of this study, progression-free survival (PFS), as assessed by hazard ratio, and overall response rate (ORR) were determined based on assessments made by a blinded Independent Review Committee (IRC). Efficacy results are presented in Table 8 and Figure 1. The median number of treatment cycles was 19 for the Empliciti arm and 14 for the comparator arm. Overall survival (OS) was a secondary endpoint with the pre-planned final OS analysis to occur after at least 427 deaths. Table 8: CA204004 Efficacy results E-Ld Ld N = 321 N = 325 PFS (ITT) Hazard Ratio [97.61% CI] 0.68 [0.55, 0.85] Stratified log-rank test p-valuea 0.0001 1-Year PFS rate (%) [95% CI] 68 [63, 73] 56 [50, 61] 2-Year PFS rate (%) [95% CI] 39 [34, 45] 26 [21, 31] 3-Year PFS rateb (%) [95% CI] 23 [18, 28] 15 [10, 20] Median PFS in months [95% CI] 18.5 [16.5, 21.4] 14.3 [12.0, 16.0] Response Overall Response (ORR)c n (%) [95% CI] 252 (78.5) [73.6, 82.9] 213 (65.5) [60.1, 70.7] p-valued 0.0002 Complete Response (CR + sCR)e n (%) 14 (4.4)f 24 (7.4) Very Good Partial Response (VGPR) n (%) 91 (28.3) 67 (20.6) Partial Response (RR/PR) n (%) 147 (45.8) 122 (37.5) Combined Responses (CR+sCR+VGPR) n (%) 105 (32.7) 91 (28.0) Overall Survivalg Hazard Ratio [95.4% CI] 0.82 [0.68, 1.00] Stratified log-rank test p-value 0.0408h Median OS in months [95% CI] 48.30 [40.34, 51.94] 39.62 [33.25, 45.27] a p-value based on the log-rank test stratified by B2 microglobulins (<3.5 mg/L versus ≥ 3.5 mg/L), number of prior lines of therapy (1 versus 2 or 3), and prior immunomodulatory therapy (no versus prior thalidomide only versus other). b A pre-specified analysis for 3-year PFS rate was performed based on a minimum follow-up time of 33 months. c European Group for Blood and Marrow Transplantation (EBMT) criteria. d p-value based on the Cochran-Mantel-Haenszel chi-square test stratified by B2 microglobulins (<3.5 mg/L versus ≥ 3.5 mg/L), number of prior lines of therapy (1 versus 2 or 3), and prior immunomodulatory therapy (no versus prior thalidomide only versus other). e Complete response (CR) + stringent complete response (sCR). f Complete response rates in Empliciti group may be underestimated due to interference of elotuzumab monoclonal antibody with immunofixation assay and serum protein electrophoresis assay. g A pre-specified final analysis for OS was performed based on at least 427 deaths with a minimum follow-up time of 70.6 months. h The final OS analysis met the protocol-specified boundary for statistical significance (p ≤ 0.046). CI: confidence interval Figure 1: CA204004 Progression free survival Number of subjects at risk E-Ld 321 282 240 206 164 133 87 43 12 1 Ld 325 262 204 168 130 97 53 24 7 Improvements observed in PFS were consistent across subsets regardless of age (< 65 versus ≥ 65), risk status, presence or absence of cytogenetic categories del17p or t(4;14), ISS stage, number of prior therapies, prior immunomodulatory exposure, prior bortezomib exposure, relapsed or refractory status or renal function as shown in Table 9. Table 9: CA204004 Efficacy results for subsets E-Ld Ld N = 321 N = 325 Subset description Median PFS (months) Median PFS (months) HR [95% CI] [95% CI] [95% CI] Age < 65 years 19.4 [15.9, 23.1] 15.7 [11.2, 18.5] 0.74 [0.55, 1.00] ≥ 65 years 18.5 [15.7, 22.2] 12.9 [10.9, 14.9] 0.64 [0.50, 0.82] Risk factors High risk 14.8 [9.1, 19.6] 7.2 [5.6, 11.2] 0.63 [0.41, 0.95] Standard risk 19.4 [16.5, 22.7] 16.4 [13.9, 18.5] 0.75 [0.59, 0.94] Cytogenetic category Presence of del17p 19.6 [15.8, NE] 14.9 [10.6, 17.5] 0.65 [0.45, 0.93] Absence of del17p 18.5 [15.8, 22.1] 13.9 [11.1, 16.4] 0.68 [0.54, 0.86] Presence of t(4;14) 15.8 [8.4, 18.4] 5.5 [3.1, 10.3] 0.55 [0.32, 0.98] Absence of t(4;14) 19.6 [17.0, 23.0] 14.9 [12.4, 17.1] 0.68 [0.55, 0.84] ISS Stage I 22.2 [17.8, 31.3] 16.4 [14.5, 18.6] 0.61 [0.45, 0.83] II 15.9 [9.5, 23.1] 12.9 [11.1, 18.5] 0.83 [0.60, 1.16] III 14.0 [9.3, 17.3] 7.4 [5.6, 11.7] 0.70 [0.48, 1.04] Prior therapies Lines of prior therapy = 1 18.5 [15.8, 20.7] 14.5 [10.9, 17.5] 0.71 [0.54, 0.94] Lines of prior therapy = 2 or 3 18.5 [15.9, 23.9] 14.0 [11.1, 15.7] 0.65 [0.50, 0.85] Prior thalidomide exposure 18.4 [14.1, 23.1] 12.3 [9.3, 14.9] 0.61 [0.46, 0.80] No prior immunomodulatory 18.9 [15.8, 22.2] 17.5 [13.0, 20.0] 0.78 [0.59, 1.04] exposure Prior bortezomib exposure 17.8 [15.8, 20.3] 12.3 [10.2, 14.9] 0.67 [0.53, 0.84] No prior bortezomib exposure 21.4 [16.6, NE] 17.5 [13.1, 21.3] 0.70 [0.48, 1.00] Response to therapy Relapsed 19.4 [16.6, 22.2] 16.6 [13.0, 18.9] 0.75 [0.59, 0.96] Refractory 16.6 [14.5, 23.3] 10.4 [6.6, 13.3] 0.55 [0.40, 0.76] Renal function Baseline CrCl < 60 mL/min 18.5 [14.8, 23.3] 11.7 [7.5, 17.4] 0.56 [0.39, 0.80] Baseline CrCl ≥ 60 mL/min 18.5 [15.9, 22.2] 14.9 [12.1, 16.7] 0.72 [0.57, 0.90] The 1-, 2-, 3-, 4- and 5-year rates of overall survival for Empliciti in combination with lenalidomide and dexamethasone treatment were 91%, 73%, 60%, 50% and 40% respectively, compared with 83%, 69%, 53%, 43% and 33% respectively, for lenalidomide and dexamethasone treatment (See Figure 2). The pre-planned final OS analysis was performed after 212 deaths in the E-Ld arm and 225 deaths in the Ld arm. The minimum follow-up was 70.6 months. A statistically significant advantage in OS was observed in patients in the E-Ld arm compared to patients in the Ld arm. The median OS in the E-Ld arm was 48.30 months compared with 39.62 months in the Ld arm. Patients in the E-Ld arm had an 18% reduction in the risk of death compared with those in the Ld arm (HR = 0.82; 95.4% CI: 0.68, 1.00; p-value = 0.0408). See Table 8 and Figure 2. Figure 2: CA204004 Overall survival Number of subjects at risk E-Ld 321 303 283 250 224 197 181 163 149 129 115 105 57 15 2 Ld 325 287 255 228 208 184 159 142 128 116 98 86 47 9 Empliciti in combination with pomalidomide and dexamethasone (CA204125) CA204125 is a randomised, open-label study conducted to evaluate the efficacy and safety of Empliciti in combination with pomalidomide and dexamethasone (E-Pd) in patients with refractory or relapsed and refractory multiple myeloma who have received at least two prior therapies including lenalidomide and a proteasome inhibitor (PI) and had disease progression on or within 60 days of their last therapy. Patients were refractory if they had progressed on or within 60 days of treatment with lenalidomide and a PI and on or within 60 days of their last treatment, or relapsed and refractory if they had achieved at least a partial response to previous treatment with lenalidomide and a PI but progressed within 6 months and had developed progressive disease on or within 60 days after completing their last treatment. Patients with Grade 2 or higher peripheral neuropathy were excluded from the clinical trials with E-Pd. A total of 117 patients were randomised in a 1:1 ratio to receive treatment: 60 to elotuzumab in combination with pomalidomide and dexamethasone (E-Pd) and 57 to pomalidomide and dexamethasone (Pd). Treatment was administered in 4-week cycles (28-day cycle) until disease progression or unacceptable toxicity. Elotuzumab 10 mg/kg bw was administered intravenously each week for the first 2 cycles and 20 mg/kg bw every 4 weeks thereafter. Dexamethasone was administered on day 1, 8, 15 and 22 of each cycle. On weeks with Empliciti infusion, dexamethasone was administered before Empliciti as a divided dose: subjects 75 years an oral dose of 28 mg and an intravenous dose of 8 mg, and in subjects > 75 years an oral dose of 8 mg and an intravenous dose of 8 mg. On weeks without an Empliciti infusion and in the control group, dexamethasone was administered in subjects 75 years as an oral dose of 40 mg and in subjects > 75 years as an oral dose of 20 mg dexamethasone. Assessment of tumour response was conducted every 4 weeks. Demographics and baseline characteristics were balanced between treatment arms. The median age was 67 years (range 36 to 81); 62% of patients were older than 65 years; 57% of patients were male; whites comprised 77% of the study population, Asians 21%, and blacks 1%. The International Staging System (ISS) Stage was I in 50%, II in 38% and III in 12% of patients. The chromosomal abnormalities as determined by the FISH of del(17p), t(4;14) and t(14;16) were present in 5%, 11% and 7% of patients, respectively. Eleven (9.4%) patients had high-risk myeloma. The median number of prior therapies was 3. Eighty-seven percent (87%) of the patients were refractory to lenalidomide, 80% refractory to a PI and 70% were refractory to both lenalidomide and a PI. Prior therapies included stem cell transplant (55%), bortezomib (100%), lenalidomide (99%), cyclophosphamide (66%), melphalan (63%), carfilzomib (21%), ixazomib (6%), and daratumumab (3%). The median number of treatment cycles was 9 for the E-Pd arm and 5 for the Pd arm. The primary endpoint was investigator assessed PFS by modified International Myeloma Working Group (IMWG) criteria. The median PFS per ITT was 10.25 months (95% CI: 5.59, non-estimable (NE)) in the E-Pd arm and 4.67 months (95% CI: 2.83, 7.16) in the Pd arm. PFS and ORR were also assessed by the IRC. PFS results per the investigator and IRC are summarised in Table 10 (minimum follow-up of 9.1 months). Kaplan-Meier curve for PFS per the investigator is provided in Figure 3. Table 10: CA204125 Progression-Free Survival and Overall Response Investigator Assessed IRC Assessedf E-Pd Pd E-Pd Pd N = 60 N = 57 N = 60 N = 57 PFS (ITT) Hazard Ratio [95% CI] 0.54 [0.34, 0.86] 0.51 [0.32, 0.82] Stratified log-rank test p-valuea 0.0078 0.0043 Median PFS in months [95% CI] 10.25 4.67 10.25 4.70 [5.59, NE] [2.83, 7.16] [6.54, NE] [2.83, 7.62] Response Overall Response (ORR)b n (%) [95% CI] 32 (53.3) 15 (26.3) 35 (58.3) 14 (24.6) [40.0, 66.3] [15.5, 39.7] [44.9, 70.9] [14.1, 37.8] p-valuec 0.0029 0.0002 Complete Response (CR + sCR)d n (%) 5 (8.3)e 1 (1.8) 0 (0.0)e 0 (0.0) Very Good Partial Response (VGPR) n (%) 7 (11.7) 4 (7.0) 9 (15.0) 5 (8.8) Partial Response (RR/PR) n (%) 20 (33.3) 10 (17.5) 26 (43.3) 9 (15.8) Combined Responses (CR+sCR+VGPR) n (%) 12 (20.0) 5 (8.8) 9 (15.0) 5 (8.8) a p-value based on the log-rank test stratified by stage of disease at study entry (International Staging System I-II vs III) and number of prior lines of therapy (2-3 vs ≥ 4) at randomization. b modified International Myeloma Working Group (IMWG) criteria. c p-value based on the Cochran-Mantel-Haenszel chi-square test stratified by stage of disease at study entry (International Staging System I-II vs III) and number of prior lines of therapy (2-3 vs ≥ 4) at randomization. d Complete response (CR) + stringent complete response (sCR). e Complete response rates in Empliciti group may be underestimated due to interference of elotuzumab monoclonal antibody with immunofixation assay and serum protein electrophoresis assay. f IRC assessment was performed post-hoc. NE: non-estimable Figure 3: CA204125 Progression free survival per investigator E-Pd Pd Probability progression free (%) HR (95% CI): 0.54 (0.34, 0.86) p-value: 0.0078 Progression free survival (Months) Number of subjects at risk E-Pd 60 48 43 37 32 25 7 1 1 1 1 Pd 57 42 31 22 16 10 6 2 1 PFS ITT assessment per investigator was evaluated in several subgroups including age (< 65 versus ≥ 65), race, ISS stage, prior therapies, transplant, risk category, ECOG status, creatinine clearance, and cytogenic abnormalities. Regardless of the subgroup evaluated, PFS was generally consistent with that observed in the ITT population for the treatment groups. However, results should be taken with caution as assessment of consistency of effect within the different subgroups was hampered by the very limited number of patients included in the different subgroups. Overall survival (OS) was a key secondary study endpoint. A pre-planned final OS analysis was performed after at least 78 deaths occurred. The minimum follow-up was 45.0 months. The OS results at final analysis reached statistical significance. A significantly longer OS was observed in patients in the E-Pd arm compared to patients in the Pd arm (HR = 0.59; 95% CI: 0.37, 0.93; p-value 0.0217), representing a 41% reduction in the risk of death. Efficacy results are presented in Table 11 and Figure 4. Table 11: CA204125 Overall Survival Results E-Pd Pd N = 60 N = 57 ** Overall Survival (OS) Hazard Ratio [95% CI] 0.59 [0.37, 0.93] * *** Stratified log-rank test p-value 0.0217 Median OS in months [95% CI] 29.80 [22.87, 45.67] 17.41 [13.83, 27.70] * p-value based on the log-rank test stratified by stage of disease at study entry (International Staging System I-II vs III) and number of prior lines of therapy (2-3 vs ≥ 4) at randomisation. ** A pre-specified final analysis for OS was performed based on at least 78 deaths (minimum follow-up time of 45.0 months). *** The final OS analysis crossed the pre-determined alpha boundary for statistical significance (p 0.20) as well as the stringent 0.05 level. Figure 4: CA204125 Overall Survival Probability alive OS (Months) Number of Subjects at Risk E-Pd 60 57 53 48 43 41 37 36 34 29 27 25 21 21 21 15 7 1 0 Pd 57 49 43 36 34 29 25 22 22 18 17 15 14 12 10 8 3 1 0 ──∆─── E-Pd (events: 37/60), median and 95% CI: 29.80 (22.87, 45.67) - - -- - - Pd (events: 41/57), median and 95% CI: 17.41 (13.83, 27.70) E-Pd vs Pd - hazard ratio and 95% CI: 0.59 (0.37, 0.93) 80% CI: 0.59 (0.44, 0.79), p-value: 0.0217 Adjusted alpha level = 0.2. Symbols represent censored observations. Stratified by stage of disease at study entry (International Staging System I-II vs III) and number of prior lines of therapy (2-3 vs ≥ 4) at randomisation.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetics (PK) of elotuzumab was studied in patients with multiple myeloma. Elotuzumab exhibits nonlinear PK with decrease in clearance with increase in dose from 0.5-20 mg/kg bw. Absorption Elotuzumab is dosed via intravenous route and therefore is immediately and completely bioavailable. Distribution The geometric mean volume of distribution of elotuzumab at the recommended dosing regimen in combination with lenalidomide/dexamethasone or pomalidomide/dexamethasone at steady state is 5.7 L (coefficient of variation (CV): 23%) and 5.6 L (CV: 21%) respectively. Biotransformation The metabolic pathway of elotuzumab has not been characterized. As an IgG monoclonal antibody, elotuzumab is expected to be degraded into small peptides and amino acids via catabolic pathways. Elimination The geometric mean total clearance of elotuzumab at 10 mg/kg bw (in combination with lenalidomide and dexamethasone) at steady state is 0.194 L/day (CV: 62.9%). Upon discontinuation of elotuzumab in combination with lenalidomide and dexamethasone or in combination with pomalidomide and dexamethasone, concentrations of elotuzumab will decrease to approximately 3% (approximately 97% washout as estimated by 5 half-lives) of the population predicted steady-state maximal serum concentration by 3 months. Special populations Based on a population PK analysis using data from 440 patients, the clearance of elotuzumab increased with increasing bw supporting a weight-based dose. Population PK analysis suggested that the following factors had no clinically important effect on the clearance of elotuzumab: age, gender, race, baseline lactate dehydrogenase (LDH), albumin, renal impairment, mild hepatic impairment, and coadministration with lenalidomide/dexamethasone or pomalidomide/dexamethasone. Target-mediated clearance of elotuzumab increased with higher serum M-protein concentrations. Renal impairment An open-label study (CA204007) evaluated the pharmacokinetics of elotuzumab in combination with lenalidomide and dexamethasone in patients with multiple myeloma with varying degrees of renal impairment (classified using the CrCl values). The effect of renal impairment on the pharmacokinetics of elotuzumab was evaluated in patients with normal renal function (CrCl > 90 mL/min; N = 8), severe renal impairment not requiring dialysis (CrCl <30 mL/min; N = 9), or end-stage renal disease requiring dialysis (CrCl < 30 mL/min; N = 9). No clinically important differences in the pharmacokinetics of elotuzumab were found between patients with severe renal impairment (with and without dialysis) and patients with normal renal function (see section 4.2). Hepatic impairment Empliciti is an IgG1 monoclonal antibody, which is principally cleared by catabolism. Thus, hepatic functional impairment is not likely to alter its clearance. The effect of hepatic impairment on the clearance of Empliciti was evaluated by population PK analyses in patients with mild hepatic impairment (TB ≤ ULN and AST > ULN or TB < 1 to 1.5 × ULN and any AST; N = 33). No clinically important differences in the clearance of Empliciti were found between patients with mild hepatic impairment and patients with normal hepatic function. Elotuzumab has not been studied in patients with moderate (TB > 1.5 to 3 × ULN and any AST) or severe hepatic impairment (TB > 3 × ULN and any AST) (see section 4.2).

פרטי מסגרת הכללה בסל
"א. התרופה תינתן לטיפול במיאלומה נפוצה בשילוב עם Lenalidomide ו-Dexamethasone כקו טיפול שני בחולה שמחלתו התקדמה לאחר טיפול קודם במשלב שכלל Thalidomide או Bortezomib ולא כלל Lenalidomide.במסגרת זו יהיה החולה זכאי לטיפול בתרופה אחת בלבד מהתרופות המפורטות להלן - Carfilzomib, Daratumumab, Elotuzumab, Ixazomib. ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה או מומחה בהמטולוגיה."
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| מיאלומה נפוצה בשילוב עם Lenalidomide ו-Dexamethasone כקו טיפול שני - כלל החולים | ||||
| מיאלומה נפוצה בשילוב עם Lenalidomide ו-Dexamethasone כקו טיפול שני כאשר החולה מוגדר בסיכון גבוה. |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
12/01/2017
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
157 14 34685 00
מחיר
0 ₪
מידע נוסף
