Quest for the right Drug
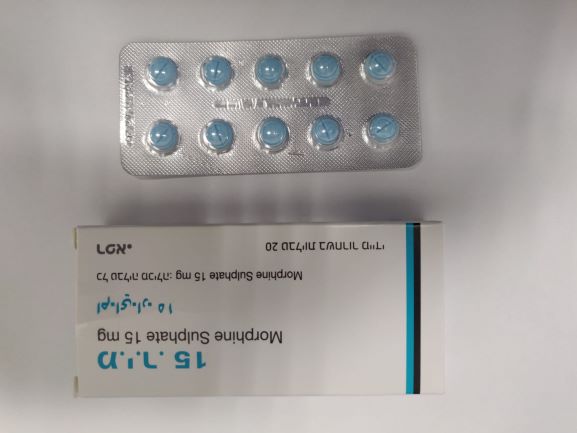
מ.י.ר. 15 M.I.R. 15 (MORPHINE SULFATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליה : TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use M.I.R. tablets should be administered in caution in patients with: • Impaired respiratory function • Respiratory depression (see below) • Severe cor pulmonale • Sleep apnoea • CNS depressant co-administration (see below and section 4.5) • Opioid Use Disorder • Acute alcoholism • Delirium tremens • Head Injury, intracranial lesions or increased intracranial pressure, reduced level of consciousness of uncertain origin • Hypotension with hypovolaemia • Hypothyroidism • Adrenocortical insufficiency • Convulsive disorders • Biliary tract disorders • Pancreatitis • Prostatic hypertrophy • Inflammatory bowel disorders • Severely impaired renal function • Severely impaired hepatic function • Constipation As with all narcotics a reduction in dosage may be advisable in the elderly. M.I.R. tablets should not be used where there is a possibility of paralytic ileus occurring. Should paralytic ileus be suspected or occur during use, M.I.R. tablets should be discontinued immediately. Respiratory Depression The major risk of opioid excess is respiratory depression. Sleep-related breathing disorders Opioids can cause sleep-related breathing disorders including central sleep apnoea (CSA) and sleep-related hypoxemia. Opioid use may increase the risk of CSA in a dose-dependent fashion. Opioids may also cause worsening of pre-existing sleep apnoea (see section 4.8). In patients who present with CSA, consider decreasing the total opioid dosage. Severe cutaneous adverse reactions (SCARs) Acute generalized exanthematous pustulosis (AGEP), which can be life-threatening or fatal, has been reported in association with morphine treatment. Most of these reactions occurred within the first 10 days of treatment. Patients should be informed about the signs and symptoms of AGEP and advised to seek medical care if they experience such symptoms. If signs and symptoms suggestive of these skin reactions appear, morphine should be withdrawn and an alternative treatment considered. Morphine may lower the seizure threshold in patients with a history of epilepsy. Risk from concomitant use of sedative medicines such as benzodiazepines or related drugs Concomitant use of M.I.R. tablets and sedative medicines, such as benzodiazepines or related drugs, may result in sedation, respiratory depression, coma and death. Because of these risks, concomitant prescribing with these sedative medicines should be reserved for patients for whom alternative treatment options are not possible. If a decision is made to prescribe M.I.R. tablets concomitantly with sedative medicines, the lowest effective dose should be used, and the duration of treatment should be as short as possible (see also general dose recommendation in section 4.2). The patients should be followed closely for signs and symptoms of respiratory depression and sedation. In this respect, it is strongly recommended to inform patients and their caregivers to be aware of these symptoms (see section 4.5). Acute chest syndrome (ACS) in patients with sickle cell disease (SCD) Due to a possible association between ACS and morphine use in SCD patients treated with morphine during a vaso- occlusive crisis, close monitoring for ACS symptoms is warranted. M.I.R. 15 and M.I.R. 30 tablets contain Lactose. Patients with rare hereditary problems of galactose intolerance, total lactase deficiency or glucose-galactose malabsorption should not take this medicine. M.I.R. 30 tablets contain azorubine, which may cause allergic reactions. Patients about to undergo additional pain-relieving procedures (e.g. surgery, plexus blockade) should not receive M.I.R. tablets for 4 hours prior to the intervention. If further treatment with M.I.R. tablets is indicated then the dosage should be adjusted to new post-operative requirements. M.I.R. tablets should be used with caution pre- operatively and within the first 24 hours post-operatively. M.I.R. tablets should also be used with caution following abdominal surgery as morphine impairs intestinal motility and should not be used until the physician is assured of normal bowel function. Opioid Use Disorder (abuse and dependence) Tolerance and physical and/or psychological dependence may develop upon repeated administration of opioids such as M.I.R tablets. Repeated use of M.I.R tablets can lead to Opioid Use Disorder (OUD). A higher dose and longer duration of opioid treatment, can increase the risk of developing OUD. Abuse or intentional misuse of M.I.R tablets may result in overdose and/or death. The risk of developing OUD is increased in patients with a personal or a family history (parents or siblings) of substance use disorders (including alcohol use disorder), in current tobacco users or in patients with a personal history of other mental health disorders (e.g. major depression, anxiety and personality disorders). Before initiating treatment with M.I.R tablets and during the treatment, treatment goals and a discontinuation plan should be agreed with the patient (see section 4.2). Before and during treatment the patient should also be informed about the risks and signs of OUD. If these signs occur, patients should be advised to contact their physician. Patients will require monitoring for signs of drug-seeking behavior (e.g. too early requests for refills). This includes the review of concomitant opioids and psycho-active drugs (like benzodiazepines). For patients with signs and symptoms of OUD, consultation with an addiction specialist should be considered. Drug dependence, tolerance and potential for abuse For all patients, prolonged use of this product may lead to drug dependence (addiction), even at therapeutic doses. The risks are increased in individuals with current or past history of substance misuse disorder (including alcohol misuse) or mental health disorder (e.g. major depression). Additional support and monitoring may be necessary when prescribing for patients at risk of opioid misuse. A comprehensive patient history should be taken to document concomitant medications, including over-the-counter medicines and medicines obtained on-line, and past and present medical and psychiatric conditions. Patients may find that treatment is less effective with chronic use and express a need to increase the dose to obtain the same level of pain control as initially experienced. Patients may also supplement their treatment with additional pain relievers. These could be signs that the patient is developing tolerance. The risks of developing tolerance should be explained to the patient. Overuse or misuse may result in overdose and/or death. It is important that patients only use medicines that are prescribed and do not give this medicine to anyone else. Patients should be closely monitored for signs of misuse, abuse or addiction. The clinical need for analgesic treatment should be reviewed regularly. Hepatobiliary disorders Morphine may cause dysfunction and spasm of the sphincter of Oddi, thus raising intrabiliary pressure and increasing the risk of biliary tract symptoms and pancreatitis. Patients with diseases of the biliary tract should be monitored for worsening of symptoms while administering morphine. Drug withdrawal syndrome Prior to starting treatment with any opioids, a discussion should be held with patients to put in place a withdrawal strategy for ending treatment with morphine. Drug withdrawal syndrome may occur upon abrupt cessation of therapy or dose reduction. When a patient no longer requires therapy, it is advisable to taper the dose gradually to minimise symptoms of withdrawal. Tapering from a high dose may take weeks to months. The opioid drug withdrawal syndrome is characterised by some or all of the following: restlessness, lacrimation, rhinorrhoea, yawning, perspiration, chills, myalgia, mydriasis and palpitations. Other symptoms may also develop including irritability, agitation, anxiety, hyperkinesia, tremor, weakness, insomnia, anorexia, abdominal cramps, nausea, vomiting, diarrhoea, increased blood pressure, increased respiratory rate or heart rate. If women take this drug during pregnancy there is a risk that their newborn infants will experience neonatal withdrawal syndrome. Hyperalgesia Hyperalgesia may be diagnosed if the patient on long-term opioid therapy presents with increased pain. This might be qualitatively and anatomically distinct from pain related to disease progression or to breakthrough pain resulting from development of opioid tolerance. Pain associated with hyperalgesia tends to be more diffuse than the pre- existing pain and less defined in quality. Symptoms of hyperalgesia may resolve with a reduction of opioid dose. Opioid analgesics may cause reversible adrenal insufficiency requiring monitoring and glucocorticoid replacement therapy. Symptoms of adrenal insufficiency may include e.g. nausea, vomiting, loss of appetite, fatigue, weakness, dizziness, or low blood pressure. Some changes that can be seen with long-term use of opioid analgesics include an increase in serum prolactin, and decreases in plasma cortisol, oestrogen and testosterone in association with inappropriately low or normal ACTH, LH or FSH levels. Clinical symptoms include decreased libido, impotence or amenorrhea which may be manifested from these hormonal changes. Plasma concentrations of morphine may be reduced by rifampicin. The analgesic effect of morphine should be monitored and doses of morphine adjusted during and after treatment with rifampicin. Oral P2Y12 inhibitor antiplatelet therapy Within the first day of concomitant P2Y12 inhibitor and morphine treatment, reduced efficacy of P2Y12 inhibitor treatment has been observed (see section 4.5) Abuse of oral dosage forms by parenteral administration can be expected to result in serious adverse events, which may be fatal.
Effects on Driving
4.7 Effects on ability to drive and use machines Treatment with M.I.R. tablets may cause sedation and it is not recommended that patients drive or use machines if they experience drowsiness. This medicine can impair cognitive function and can affect a patient's ability to drive safely. When prescribing this medicine, patients should be told: • The medicine is likely to affect your ability to drive. • Do not drive until you know how the medicine affects you.

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| MORPHINE | ||||
| HYDROMORPHONE | ||||
| For the relief of severe pain in cancer. |
שימוש לפי פנקס קופ''ח כללית 1994
Severe and intractable oncological and postoperative pain
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
15.06.21 - עלון לצרכן אנגלית 15.06.21 - עלון לצרכן עברית 15.06.21 - עלון לצרכן ערבית 21.09.23 - עלון לצרכן עברית 12.01.24 - עלון לצרכן אנגלית 11.01.24 - עלון לצרכן עברית 12.01.24 - עלון לצרכן ערבית 14.05.24 - עלון לצרכן עברית 30.08.24 - עלון לצרכן עברית 01.07.20 - החמרה לעלון 02.02.21 - החמרה לעלון 26.06.13 - החמרה לעלון 21.09.23 - החמרה לעלון 14.05.24 - החמרה לעלון 30.08.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
מ.י.ר. 15