Quest for the right Drug
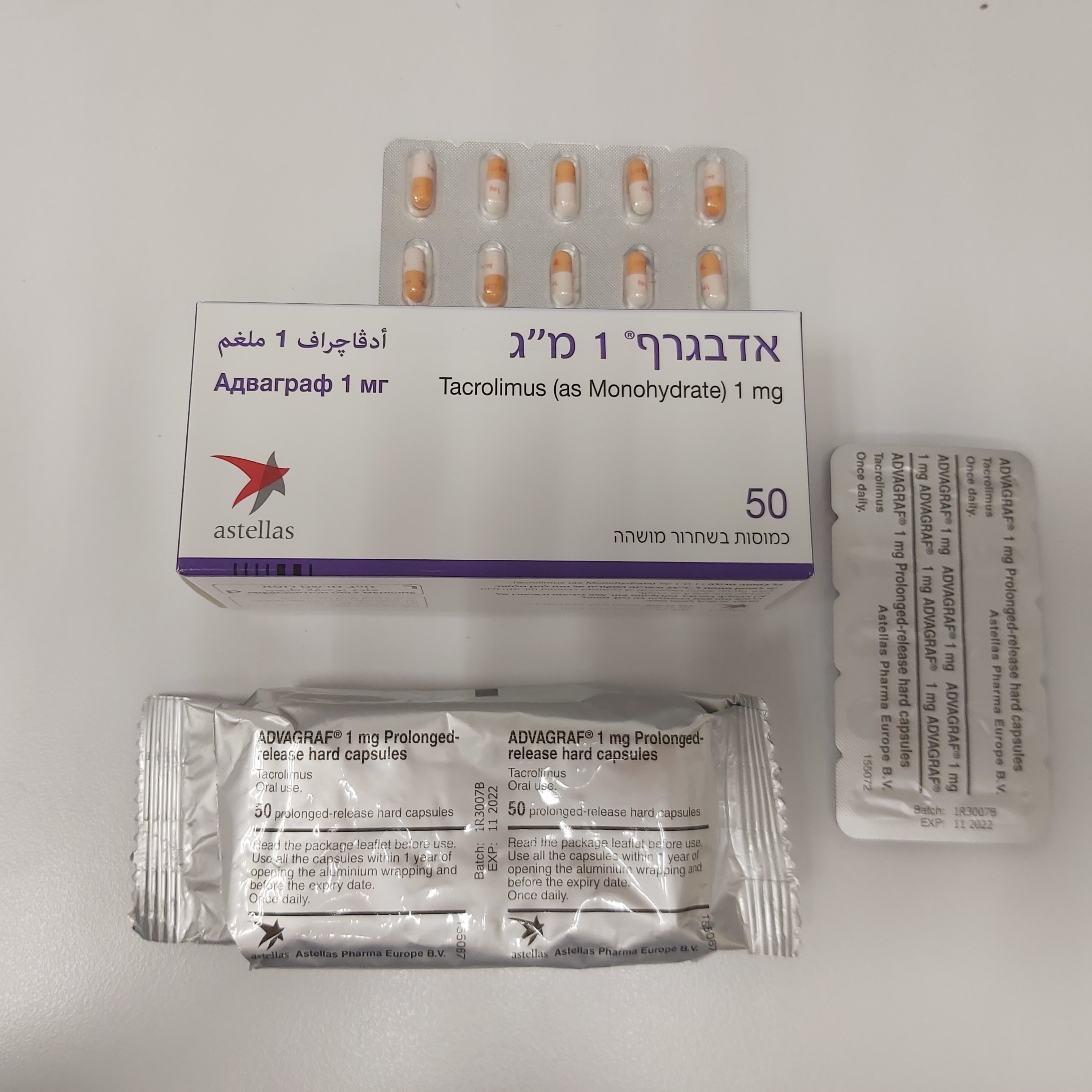
אדבגרף 1 מ"ג ADVAGRAF 1 MG (TACROLIMUS AS MONOHYDRATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
קפסולות בשחרור ממושך : CAPSULES PROLONGED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Immunosuppressants, calcineurin inhibitors, ATC code: L04AD02 Mechanism of action At the molecular level, the effects of tacrolimus appear to be mediated by binding to a cytosolic protein (FKBP12) which is responsible for the intracellular accumulation of the compound. The FKBP12- tacrolimus complex specifically and competitively binds to and inhibits calcineurin, leading to a calcium- dependent inhibition of T-cell signal transduction pathways, thereby preventing transcription of a discrete set of cytokine genes. Tacrolimus is a highly potent immunosuppressive agent and has proven activity in both in vitro and in vivo experiments. In particular, tacrolimus inhibits the formation of cytotoxic lymphocytes, which are mainly responsible for graft rejection. Tacrolimus suppresses T-cell activation and T-helper-cell dependent B-cell proliferation, as well as the formation of lymphokines (such as interleukins-2, -3, and γ-interferon) and the expression of the interleukin-2 receptor. Results from clinical trials performed with once-daily tacrolimus Advagraf Liver transplantation The efficacy and safety of Advagraf and Prograf, both in combination with corticosteroids, was compared in 471 de novo liver transplant recipients. The event rate of biopsy confirmed acute rejection within the first 24 weeks after transplantation was 32.6% in the Advagraf group (N=237) and 29.3% in the Prograf group (N=234). The treatment difference (Advagraf – Prograf) was 3.3% (95% confidence interval [-5.7%, 12.3%]). The 12-month patient survival rates were 89.2% for Advagraf and 90.8% for Prograf; in the Advagraf arm 25 patients died (14 female, 11 male) and in the Prograf arm 24 patients died (5 female, 19 male). 12-month graft survival was 85.3% for Advagraf and 85.6% for Prograf. Kidney transplantation The efficacy and safety of Advagraf and Prograf, both in combination with mycophenolate mofetil (MMF) and corticosteroids, was compared in 667 de novo kidney transplant recipients. The event rate for biopsy-confirmed acute rejection within the first 24 weeks after transplantation was 18.6% in the Advagraf group (N=331) and 14.9% in the Prograf group (N=336). The treatment difference (Advagraf- Prograf) was 3.8% (95% confidence interval [-2.1%, 9.6%]). The 12-month patient survival rates were 96.9% for Advagraf and 97.5% for Prograf; in the Advagraf arm 10 patients died (3 female, 7 male) and in the Prograf arm 8 patients died (3 female, 5 male). 12-month graft survival was 91.5% for Advagraf and 92.8% for Prograf. The efficacy and safety of Prograf, ciclosporin and Advagraf, all in combination with basiliximab antibody induction, MMF and corticosteroids, was compared in 638 de novo kidney transplant recipients. The incidence of efficacy failure at 12 months (defined as death, graft loss, biopsy-confirmed acute rejection, or lost to follow-up) was 14.0% in the Advagraf group (N=214), 15.1% in the Prograf group (N=212) and 17.0% in the ciclosporin group (N=212). The treatment difference was -3.0% (Advagraf- ciclosporin) (95.2% confidence interval [-9.9%, 4.0%]) for Advagraf vs. ciclosporin and -1.9% (Prograf- ciclosporin) (95.2% confidence interval [-8.9%, 5.2%]) for Prograf vs. ciclosporin. The 12-month patient survival rates were 98.6% for Advagraf, 95.7% for Prograf and 97.6% for ciclosporin; in the Advagraf arm 3 patients died (all male), in the Prograf arm 10 patients died (3 female, 7 male) and in the ciclosporin arm 6 patients died (3 female, 3 male). 12-month graft survival was 96.7% for Advagraf, 92.9% for Prograf and 95.7% for ciclosporin. Clinical efficacy and safety of Prograf capsules bid in primary organ transplantation In prospective studies oral Prograf was investigated as primary immunosuppressant in approximately 175 patients following lung, 475 patients following pancreas and 630 patients following intestinal transplantation. Overall, the safety profile of oral Prograf in these published studies appeared to be similar to what was reported in the large studies, where Prograf was used as primary treatment in liver, kidney and heart transplantation. Efficacy results of the largest studies in each indication are summarised below. Lung transplantation The interim analysis of a recent multicentre study using oral Prograf discussed 110 patients who underwent 1:1 randomisation to either tacrolimus or ciclosporin. Tacrolimus was started as continuous intravenous infusion at a dose of 0.01 to 0.03 mg/kg/day and oral tacrolimus was administered at a dose of 0.05 to 0.3 mg/kg/day. A lower incidence of acute rejection episodes for tacrolimus- versus ciclosporin-treated patients (11.5% versus 22.6%) and a lower incidence of chronic rejection, the bronchiolitis obliterans syndrome (2.86% versus 8.57%), was reported within the first year after transplantation. The 1-year patient survival rate was 80.8% in the tacrolimus and 83% in the ciclosporin group. Another randomised study included 66 patients on tacrolimus versus 67 patients on ciclosporin. Tacrolimus was started as continuous intravenous infusion at a dose of 0.025 mg/kg/day and oral tacrolimus was administered at a dose of 0.15 mg/kg/day with subsequent dose adjustments to target trough levels of 10 to 20 ng/ml. The 1-year patient survival was 83% in the tacrolimus and 71% in the ciclosporin group, the 2-year survival rates were 76% and 66%, respectively. Acute rejection episodes per 100 patient-days were numerically fewer in the tacrolimus (0.85 episodes) than in the ciclosporin group (1.09 episodes). Obliterative bronchiolitis developed in 21.7% of patients in the tacrolimus group compared with 38.0% of patients in the ciclosporin group (p=0.025). Significantly more ciclosporin- treated patients (n=13) required a switch to tacrolimus than tacrolimus-treated patients to ciclosporin (n=2) (p=0.02) (Keenan et al., Ann Thoracic Surg 1995;60:580). In an additional two-centre study, 26 patients were randomised to the tacrolimus versus 24 patients to the ciclosporin group. Tacrolimus was started as continuous intravenous infusion at a dose of 0.05 mg/kg/day and oral tacrolimus was administered at a dose of 0.1 to 0.3 mg/kg/day with subsequent dose adjustments to target trough levels of 12 to 15 ng/ml. The 1-year survival rates were 73.1% in the tacrolimus versus 79.2% in the ciclosporin group. Freedom from acute rejection was higher in the tacrolimus group at 6 months (57.7% versus 45.8%) and at 1 year after lung transplantation (50% versus 33.3%). The three studies demonstrated similar survival rates. The incidences of acute rejection were numerically lower with tacrolimus in all three studies and one of the studies reported a significantly lower incidence of bronchiolitis obliterans syndrome with tacrolimus. Pancreas transplantation A multicentre study using oral Prograf included 205 patients undergoing simultaneous pancreas-kidney transplantation who were randomised to tacrolimus (n=103) or to ciclosporin (n=102). The initial oral per protocol dose of tacrolimus was 0.2 mg/kg/day with subsequent dose adjustments to target trough levels of 8 to 15 ng/ml by Day 5 and 5 to 10 ng/ml after Month 6. Pancreas survival at 1 year was significantly superior with tacrolimus: 91.3% versus 74.5% with ciclosporin (p < 0.0005), whereas renal graft survival was similar in both groups. In total 34 patients switched treatment from ciclosporin to tacrolimus, whereas only 6 tacrolimus patients required alternative therapy. Intestinal transplantation Published clinical experience from a single centre on the use of oral Prograf for primary treatment following intestinal transplantation showed that the actuarial survival rate of 155 patients (65 intestine alone, 75 liver and intestine, and 25 multivisceral) receiving tacrolimus and prednisone was 75% at 1 year, 54% at 5 years, and 42% at 10 years. In the early years the initial oral dose of tacrolimus was 0.3 mg/kg/day. Results continuously improved with increasing experience over the course of 11 years. A variety of innovations, such as techniques for early detection of Epstein-Barr (EBV) and CMV infections, bone marrow augmentation, the adjunct use of the interleukin-2 antagonist daclizumab, lower initial tacrolimus doses with target trough levels of 10 to 15 ng/ml, and most recently allograft irradiation were considered to have contributed to improved results in this indication over time.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption In man tacrolimus has been shown to be able to be absorbed throughout the gastrointestinal tract. Available tacrolimus is generally rapidly absorbed. Advagraf is a prolonged-release formulation of tacrolimus resulting in an extended oral absorption profile with an average time to maximum blood concentration (Cmax) of approximately 2 hours (tmax). Absorption is variable and the mean oral bioavailability of tacrolimus (investigated with the Prograf formulation) is in the range of 20% - 25% (individual range in adult patients 6% - 43%). The oral bioavailability of Advagraf was reduced when it was administered after a meal. Both the rate and extent of absorption of Advagraf were reduced when administered with food. Bile flow does not influence the absorption of tacrolimus and therefore treatment with Advagraf may commence orally. A strong correlation exists between AUC and whole blood trough levels at steady-state for Advagraf. Monitoring of whole blood trough levels therefore provides a good estimate of systemic exposure. Distribution In man, the disposition of tacrolimus after intravenous infusion may be described as biphasic. In the systemic circulation, tacrolimus binds strongly to erythrocytes resulting in an approximate 20:1 distribution ratio of whole blood/plasma concentrations. In plasma, tacrolimus is highly bound (> 98.8%) to plasma proteins, mainly to serum albumin and α-1-acid glycoprotein. Tacrolimus is extensively distributed in the body. The steady-state volume of distribution based on plasma concentrations is approximately 1300 l (healthy subjects). Corresponding data based on whole blood averaged 47.6 l. Metabolism Tacrolimus is widely metabolised in the liver, primarily by the cytochrome P450-3A4 (CYP3A4) and the cytochrome P450-3A5 (CYP3A5). Tacrolimus is also considerably metabolised in the intestinal wall. There are several metabolites identified. Only one of these has been shown in vitro to have immunosuppressive activity similar to that of tacrolimus. The other metabolites have only weak or no immunosuppressive activity. In systemic circulation only one of the inactive metabolites is present at low concentrations. Therefore, metabolites do not contribute to the pharmacological activity of tacrolimus. Excretion Tacrolimus is a low-clearance substance. In healthy subjects, the average total body clearance estimated from whole blood concentrations was 2.25 l/h. In adult liver, kidney and heart transplant patients, values of 4.1 l/h, 6.7 l/h and 3.9 l/h, respectively, have been observed. Factors such as low haematocrit and protein levels, which result in an increase in the unbound fraction of tacrolimus, or corticosteroid-induced increased metabolism, are considered to be responsible for the higher clearance rates observed following transplantation. The half-life of tacrolimus is long and variable. In healthy subjects, the mean half-life in whole blood is approximately 43 hours. Following intravenous and oral administration of 14C-labelled tacrolimus, most of the radioactivity was eliminated in the faeces. Approximately 2% of the radioactivity was eliminated in the urine. Less than 1% of unchanged tacrolimus was detected in the urine and faeces, indicating that tacrolimus is almost completely metabolised prior to elimination: bile being the principal route of elimination.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול במקרים האלה: א. מושתלי כליה ב. מושתלי כבד. ג. מושתלי לב. ד. מושתלי ריאה. 2. מתן התרופה ייעשה לפי מרשם של רופא מומחה באימונולוגיה קלינית או רופא מומחה העוסק בתחום ההשתלות
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
09/03/1999
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
153 08 34073 00
מחיר
0 ₪
מידע נוסף
עלון מידע לצרכן
26.04.22 - עלון לצרכן אנגלית 26.04.22 - עלון לצרכן עברית 24.05.20 - עלון לצרכן ערבית 05.12.22 - עלון לצרכן אנגלית 05.12.22 - עלון לצרכן עברית 05.12.22 - עלון לצרכן ערבית 25.08.15 - החמרה לעלון 05.08.18 - החמרה לעלון 06.09.20 - החמרה לעלון 26.04.22 - החמרה לעלון 05.12.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אדבגרף 1 מ"ג