Quest for the right Drug
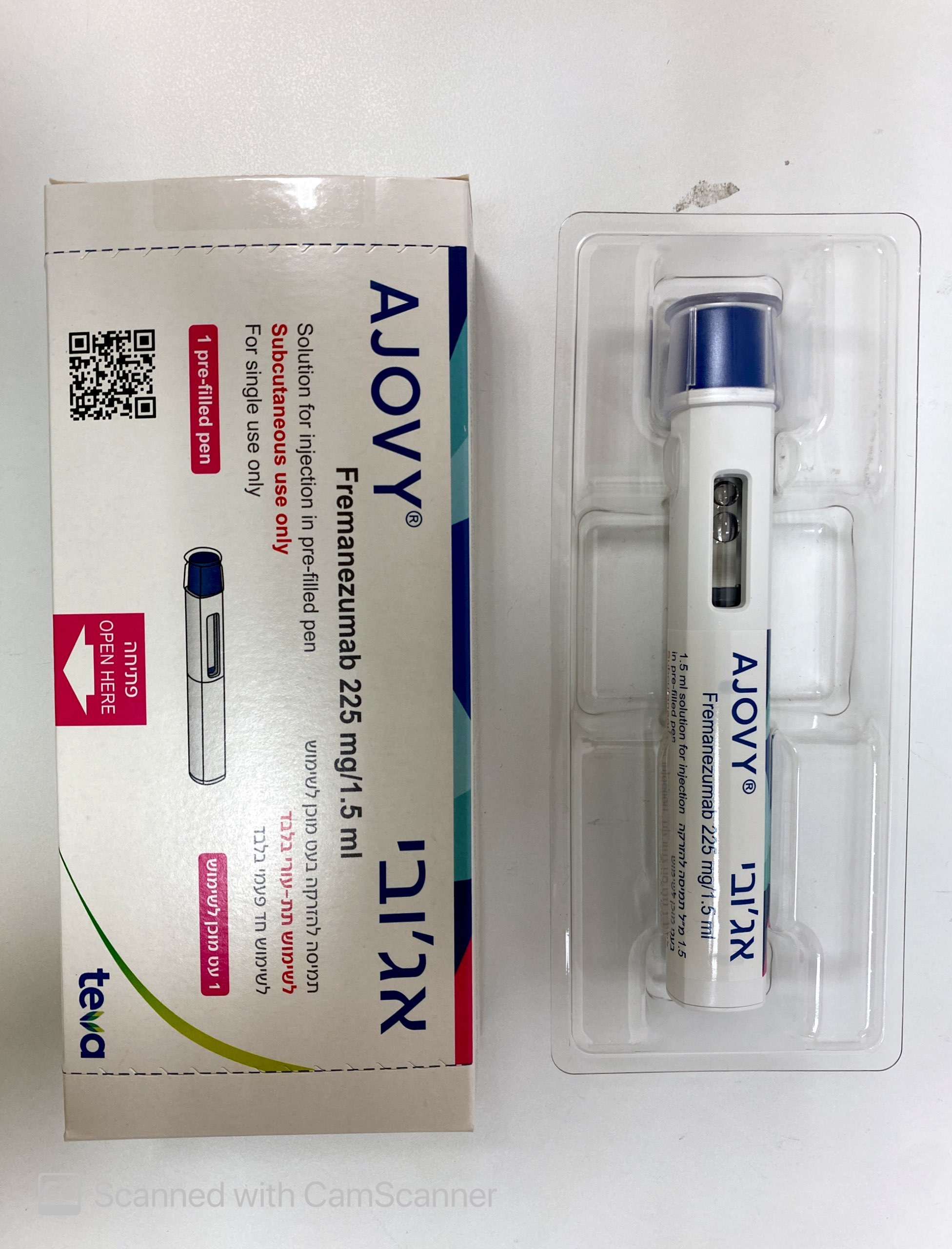
אג'ובי AJOVY (FREMANEZUMAB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Calcitonin gene-related peptide (CGRP) antagonists ATC code: N02CD03 Mechanism of action Fremanezumab is a humanised IgG2Δa/kappa monoclonal antibody derived from a murine precursor. Fremanezumab selectively binds the calcitonin gene-related peptide (CGRP) ligand and blocks both CGRP isoforms (α-and β-CGRP) from binding to the CGRP receptor. While the precise mechanism of action by which fremanezumab prevents migraine attacks is unknown, it is believed that prevention of migraine is obtained by its effect modulating the trigeminal system. CGRP levels have been shown to increase significantly during migraine and return to normal with headache relief. Fremanezumab is highly specific for CGRP and does not bind to closely related family members (e.g., amylin, calcitonin, intermedin and adrenomedullin). Clinical efficacy and safety The efficacy of fremanezumab was assessed in two randomised, 12-week, double-blind, placebo- controlled phase III studies in adult patients with episodic (Study 1) and chronic migraine (Study 2). The patients enrolled had at least a 12-month history of migraine (with and without aura) according to the International Classification of Headache Disorders (ICHD-III) diagnostic criteria. Elderly patients (>70 years), patients using opioids or barbiturates on more than 4 days per month, and patients with pre-existing myocardial infarction, cerebrovascular accident, and thromboembolic events were excluded. Episodic migraine study (Study 1) The efficacy of fremanezumab was evaluated in episodic migraine in a randomised, multicentre, 12-week, placebo-controlled, double-blind study (Study 1). Adults with a history of episodic migraine (less than 15 headache days per month) were included in the study. A total of 875 patients (742 females, 133 males) were randomised into one of three arms: 675 mg fremanezumab every three months (quarterly, n=291), 225 mg fremanezumab once a month (monthly, n=290), or monthly administration of placebo (n=294) administered via subcutaneous injection. Demographics and baseline disease characteristics were balanced and comparable between the study arms. Patients had a median age of 42 years (range: 18 to 70 years), 85% were female, and 80% were white. The mean migraine frequency at baseline was approximately 9 migraine days per month. Patients were allowed to use acute headache treatments during the study. A sub-set of patients (21%) was also allowed to use one commonly used concomitant, preventive medicinal product (beta-blockers, calcium channel blocker/benzocycloheptene, antidepressants, anticonvulsants). Overall, 19% of the patients had previously used topiramate. A total of 791 patients completed the 12-week double-blind treatment period. The primary efficacy endpoint was the mean change from baseline in the monthly average number of migraine days during the 12-week treatment period. Key secondary endpoints were the achievement of at least 50% reduction from baseline in monthly migraine days (50% responder rate), mean change from baseline in the patient reported MIDAS score, and change from baseline in monthly average number of days of acute headache medicinal product use. Both monthly and quarterly dosing regimens of fremanezumab demonstrated statistically significant and clinically meaningful improvement from baseline compared to placebo for key endpoints (see Table 2). The effect also occurred from as early as the first month and sustained over the treatment period (see Figure 1). Figure 1: Mean Change from Baseline in the Monthly Average Number of Migraine Days for Study 1 Placebo AJOVY Quarterly AJOVY Monthly 0.0 -0.5 LS Mean (+/- SE) Change from Baseline -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 -4.5 Visit: Baseline Week 1 Week 2 Week 3 Month 1 Month 2 Month 3 AJOVY Monthly <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 0.0002 AJOVY Quarterly <0.0001 <0.0001 0.0003 <0.0001 0.0009 0.0013 Mean at baseline (monthly average number of migraine days): Placebo: 9.1, AJOVY Quarterly: 9.2, AJOVY Monthly: 8.9. Table 2: Key Efficacy Outcomes in Study 1 in Episodic Migraine Efficacy Endpoint Placebo Fremanezumab Fremanezumab (n=290) 675 mg quarterly 225 mg monthly (n=288) (n=287) MMD Mean changea (95% -2.2 (-2.68, -1.71) -3.4 (-3.94, -2.96) -3.7 (-4.15, -3.18) CI) - -1.2 (-1.74, -0.69) -1.4 (-1.96, -0.90) TD (95% CI)b 9.1 (2.65) 9.2 (2.62) 8.9 (2.63) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 MHD Mean changea (95% -1.5 (-1.88, -1.06) -3.0 (-3.39, -2.55) -2.9 (-3.34, -2.51) CI) - -1.5 (-1.95, -1.02) -1.5 (-1.92, -0.99) TD (95% CI)b 6.9 (3.13) 7.2 (3.14) 6.8 (2.90) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 50% Responder Rate MMD Percentage [%] 27.9% 44.4% 47.7% P-value (vs. placebo) - p<0.0001 p<0.0001 75% Responder Rate MMD Percentage [%] 9.7% 18.4% 18.5% P-value (vs. placebo) - p=0.0025 p=0.0023 MIDAS total Mean changea (95% -17.5 (-20.62, -14.47) -23.0 (-26.10, -19.82) -24.6 (-27.68, -21.45) CI) 37.3 (27.75) 41.7 (33.09) 38 (33.30) Baseline (SD) P-value (vs. placebo)a - p=0.0023 p<0.0001 MAHMD Mean changea (95% -1.6 (-2.04, -1.20) -2.9 (-3.34, -2.48) -3.0 (-3.41, -2.56) CI) - -1.3 (-1.73, -0.78) -1.3 (-1.81, -0.86) TD (95% CI)b 7.7 (3.60) 7.7 (3.70) 7.7 (3.37) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 CI = confidence interval; MAHMD = monthly acute headache medication days; MHD = monthly headache days of at least moderate severity; MIDAS = Migraine Disability Assessment; MMD = monthly migraine days; SD = standard deviation; TD = treatment difference a For all endpoints mean change and CIs are based on the ANCOVA model that included treatment, gender, region, and baseline preventive medication use (yes/no) as fixed effects and corresponding baseline value and years since onset of migraine as covariates. b Treatment difference is based on the MMRM analysis with treatment, gender, region, and baseline preventive medication use (yes/no), month, and treatment month as fixed effects and corresponding baseline value and years since onset of migraine as covariates. In patients on one other concomitant, migraine preventive medicinal product, the treatment difference for the reduction of monthly migraine days (MMD) observed between fremanezumab 675 mg quarterly and placebo was -1.8 days (95% CI: -2.95, -0.55) and between fremanezumab 225 mg monthly and placebo -2.0 days (95% CI: -3.21, -0.86). In patients who had previously used topiramate the treatment difference for the reduction of monthly migraine days (MMD) observed between fremanezumab 675 mg quarterly and placebo was -2.3 days (95% CI: -3.64, -1.00) and between fremanezumab 225 mg monthly and placebo -2.4 days (95% CI: -3.61, -1.13). Chronic migraine study (Study 2) Fremanezumab was evaluated in chronic migraine in a randomised, multicentre, 12-week, placebo- controlled, double-blind study (Study 2). The study population included adults with a history of chronic migraine (15 headache days or higher per month). A total of 1,130 patients (991 females, 139 males) were randomised into one of three arms: 675 mg fremanezumab starting dose followed by 225 mg fremanezumab once a month (monthly, n=379), 675 mg fremanezumab every three months (quarterly, n=376), or monthly administration of placebo (n=375) administered via subcutaneous injection. Demographics and baseline disease characteristics were balanced and comparable between the study arms. Patients had a median age of 41 years (range: 18 to 70 years), 88% were female, and 79% were white. The mean headache frequency at baseline was approximately 21 headache days per month (of which 13 headache days were of at least moderate severity). Patients were allowed to use acute headache treatments during the study. A sub-set of patients (21%) was also allowed to use one commonly used concomitant, preventive medicinal product (beta-blockers, calcium channel blocker/benzocycloheptene, antidepressants, anticonvulsants). Overall, 30% of the patients had previously used topiramate and 15% onabotulinumtoxin A. A total of 1,034 patients completed the 12-week double-blind treatment period. The primary efficacy endpoint was the mean change from baseline in the monthly average number of headache days of at least moderate severity during the 12-week treatment period. Key secondary endpoints were the achievement of at least 50% reduction from baseline in monthly headache days of at least moderate severity (50% responder rate), mean change from baseline in the patient reported HIT-6 score, and change from baseline in monthly average number of days of acute headache medicinal product use. Both monthly and quarterly dosing regimens of fremanezumab demonstrated statistically significant and clinically meaningful improvement from baseline compared to placebo for key endpoints (see Table 3). The effect also occurred from as early as the first month and sustained over the treatment period (see Figure 2). Figure 2: Mean Change from Baseline in the Monthly Average Number of Headache Days of At Least Moderate Severity for Study 2 Placebo AJOVY Quarterly AJOVY Monthly 0.0 -0.5 LS Mean (+/- SE) Change from Baseline -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 -4.5 -5.0 -5.5 Visit: Baseline Week 1 Week 2 Week 3 Month 1 Month 2 Month 3 AJOVY Monthly <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 AJOVY Quarterly <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 0.0007 Mean at baseline (monthly average number of headache days of at least moderate severity): Placebo: 13.3, AJOVY Quarterly: 13.2, AJOVY Monthly: 12.8. Table 3: Key Efficacy Outcomes in Study 2 in Chronic Migraine Efficacy Endpoint Placebo Fremanezumab Fremanezumab (n=371) 675 mg quarterly 225 mg monthly with (n=375) 675 mg starting dose (n=375) MHD Mean changea (95% -2.5 (-3.06, -1.85) -4.3 (-4.87, -3.66) -4.6 (-5.16, -3.97) CI) - -1.8 (-2.45, -1.13) -2.1 (-2.77, -1.46) TD (95% CI)b 13.3 (5.80) 13.2 (5.45) 12.8 (5.79) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 MMD Mean changea (95% -3.2 (-3.86, -2.47) -4.9 (-5.59, -4.20) -5.0 (-5.70, -4.33) CI) - -1.7 (-2.44, -0.92) -1.9 (-2.61, -1.09) TD (95% CI)b 16.3 (5.13) 16.2 (4.87) 16.0 (5.20) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 50% Responder Rate MHD Percentage [%] 18.1% 37.6% 40.8% P-value (vs. placebo) - p<0.0001 p<0.0001 75% Responder Rate MHD Percentage [%] 7.0% 14.7% 15.2% P-value (vs. placebo) - p=0.0008 p=0.0003 HIT-6 total Mean changea (95% -4.5 (-5.38, -3.60) -6.4 (-7.31, -5.52) -6.7 (-7.71, -5.97) CI) 64.1 (4.79) 64.3 (4.75) 64.6 (4.43) Baseline (SD) P-value (vs. placebo)a - p=0.0001 p<0.0001 MAHMD Mean changea (95% -1.9 (-2.48, -1.28) -3.7 (-4.25, -3.06) -4.2 (-4.79, -3.61) CI) - -1.7 (-2.40, -1.09) -2.3 (-2.95, -1.64) TD (95% CI)b 13.0 (6.89) 13.1 (6.79) 13.1 (7.22) Baseline (SD) P-value (vs. placebo)a - p<0.0001 p<0.0001 CI = confidence interval; HIT-6 = Headache Impact Test; MAHMD = monthly acute headache medication days; MHD = monthly headache days of at least moderate severity; MMD = monthly migraine days; SD = standard deviation; TD = treatment difference a For all endpoints mean change and CIs are based on the ANCOVA model that included treatment, gender, region, and baseline preventive medication use (yes/no) as fixed effects and corresponding baseline value and years since onset of migraine as covariates. b Treatment difference is based on the MMRM analysis with treatment, gender, region, and baseline preventive medication use (yes/no), month, and treatment month as fixed effects and corresponding baseline value and years since onset of migraine as covariates. In patients on one other concomitant, migraine preventive medicinal product, the treatment difference for the reduction of monthly headache days (MHD) of at least moderate severity observed between fremanezumab 675 mg quarterly and placebo was -1.3 days (95% CI: -2.66, 0.03) and between fremanezumab 225 mg monthly with 675 mg starting dose and placebo -2.0 days (95% CI: -3.27, -0.67). In patients who had previously used topiramate the treatment difference for the reduction of monthly headache days (MHD) of at least moderate severity observed between fremanezumab 675 mg quarterly and placebo was -2.7 days (95% CI: -3.88, -1.51) and between fremanezumab 225 mg monthly with 675 mg starting dose and placebo -2.9 days (95% CI: -4.10, -1.78). In patients who had previously used onabotulinumtoxin A the treatment difference for the reduction of monthly headache days (MHD) of at least moderate severity observed between fremanezumab 675 mg quarterly and placebo was -1.3 days (95% CI: -3.01, -0.37) and between fremanezumab 225 mg monthly with 675 mg starting dose and placebo -2.0 days (95% CI: -3.84, -0.22). Approximately 52% of the patients in the study had acute headache medication overuse. The observed treatment difference for the reduction of monthly headache days (MHD) of at least moderate severity between fremanezumab 675 mg quarterly and placebo in these patients was -2.2 days (95% CI: -3.14, -1.22) and between fremanezumab 225 mg monthly with 675 mg starting dose and placebo -2.7 days (95% CI: -3.71, -1.78). Long-term study (Study 3) For all episodic and chronic migraine patients, efficacy was sustained for up to 12 additional months in the long-term study (Study 3), in which patients received 225 mg fremanezumab monthly or 675 mg quarterly. 79% of patients completed the 12-month treatment period of Study 3. Pooled across the two dosing regimens, a reduction of 6.6 monthly migraine days was observed after 15 months relative to Study 1 and Study 2 baseline. 61% of patients completing Study 3 achieved a 50% response in the last month of the study. No safety signal was observed during the 15-month combined treatment period. Intrinsic and extrinsic factors The efficacy and safety of fremanezumab was demonstrated regardless of age, gender, race, use of concomitant preventive medicinal products (beta-blockers, calcium channel blocker/ benzocycloheptene, antidepressants, anticonvulsants), use of topiramate or onabotulinumtoxin A for migraine in the past, and acute headache medication overuse. There is limited data available on the use of fremanezumab in patients ≥65 years of age (2% of the patients). Difficult to treat migraine The efficacy and safety of fremanezumab in a total of 838 episodic and chronic migraine patients with documented inadequate response to two to four classes of prior migraine preventive medicinal products was assessed in a randomised study (Study 4), which was composed of a 12-week double- blind, placebo-controlled treatment period followed by a 12-week open-label period. The primary efficacy endpoint was the mean change from baseline in the monthly average number of migraine days during the 12-week double-blind treatment period. Key secondary endpoints were the achievement of at least 50% reduction from baseline in monthly migraine days, the mean change from baseline in the monthly average number of headache days of at least moderate severity and change from baseline in monthly average number of days of acute headache medicinal product use. Both monthly and quarterly dosing regimens of fremanezumab demonstrated statistically significant and clinically meaningful improvement from baseline compared to placebo for key endpoints. Therefore, the results of Study 4 are consistent with the main findings of the previous efficacy studies and in addition demonstrate efficacy in difficult to treat migraine, including mean reduction in monthly migraine days (MMD) of -3.7 (95% CI: -4.38, -3.05) with fremanezumab quarterly and -4.1 (95% CI: -4.73, -3.41) with fremanezumab monthly compared to -0.6 (95% CI: -1.25, 0.07) in placebo-treated patients. 34% of the patients treated with fremanezumab quarterly and 34% of the patients treated with fremanezumab monthly achieved at least 50% reduction in MMD, compared to 9% in placebo-treated patients (p<0.0001) during the 12-week treatment period. The effect also occurred from as early as the first month and was sustained over the treatment period (see Figure 3). No safety signal was observed during the 6-month treatment period. Figure 3: Mean Change from Baseline in Monthly Average Number of Migraine Days for Study 4 Placebo AJOVY Quarterly AJOVY Monthly LS Mean (+/- SE) Change from Baseline 0.0 -0.5 -1.0 -1.5 -2.0 -2.5 -3.0 -3.5 -4.0 -4.5 -5.0 -5.5 Visit: Baseline Month 1 Month 2 Month 3 AJOVY Monthly <0.0001 <0.0001 <0.0001 AJOVY Quarterly <0.0001 <0.0001 <0.0001 Mean at baseline (monthly average number of migraine days): Placebo: 14.4, AJOVY Quarterly: 14.1, AJOVY Monthly: 14.1. Paediatric population The European Medicines Agency has deferred the obligation to submit the results of studies with AJOVY in one or more subsets of the paediatric population in prevention of migraine headaches (see section 4.2 for information on paediatric use).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption After single subcutaneous administrations of 225 mg and 675 mg fremanezumab, median time to maximum concentrations (tmax) in healthy subjects was 5 to 7 days. The absolute bioavailability of fremanezumab after subcutaneous administration of 225 mg and 900 mg in healthy subjects was 55% (±SD of 23%) to 66% (±SD of 26%). Dose proportionality, based on population pharmacokinetics, was observed between 225 mg to 675 mg. Steady state was achieved by approximately 168 days (about 6 months) following 225 mg monthly and 675 mg quarterly dosing regimens. Median accumulation ratio, based on once monthly and once quarterly dosing regimens, is approximately 2.4 and 1.2, respectively. Distribution Assuming the model-derived estimated bioavailability of 66% (±SD of 26%) holds for the patient population, the volume of distribution for a typical patient was 3.6 L (35.1% CV) following subcutaneous administration of 225 mg, 675 mg and 900 mg of fremanezumab. Biotransformation Similar to other monoclonal antibodies, fremanezumab is expected to be degraded by enzymatic proteolysis into small peptides and amino acids. Elimination Assuming the model-derived estimated bioavailability of 66% (±SD of 26%) holds for the patient population, central clearance for a typical patient was 0.09 L/day (23.4% CV) following subcutaneous administration of 225 mg, 675 mg and 900 mg of fremanezumab. The formed small peptides and amino acids may be re-used in the body for de novo synthesis of proteins or are excreted by the kidney. Fremanezumab has an estimated half-life of 30 days. Special populations A population pharmacokinetic analysis looking at age, race, gender, and weight was conducted on data from 2,546 subjects. Approximately twice as much exposure is expected in the lowest body weight quartile (43.5 to 60.5 kg) compared to the highest body weight quartile (84.4 to131.8 kg). However, body weight did not have an observed effect on the clinical efficacy based on the exposure-response analyses in episodic and chronic migraine patients. No dose adjustments are required for fremanezumab. No data on exposure-efficacy relationship in subjects with body weight >132 kg is available. Renal or hepatic impairment Since monoclonal antibodies are not known to be eliminated via renal pathways or metabolised in the liver, renal and hepatic impairment are not expected to impact the pharmacokinetics of fremanezumab. Patients with severe renal impairment (eGFR <30 mL/min/1.73 m2) have not been studied. Population pharmacokinetic analysis of integrated data from the AJOVY clinical studies did not reveal a difference in the pharmacokinetics of fremanezumab in patients with mild to moderate renal impairment or hepatic impairment relative to those with normal renal or hepatic function (see section 4.2).

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
ATC
מידע נוסף
עלון מידע לצרכן
02.11.20 - עלון לצרכן אנגלית 01.03.22 - עלון לצרכן עברית 01.03.22 - עלון לצרכן עברית 02.11.20 - עלון לצרכן ערבית 03.01.23 - עלון לצרכן אנגלית 03.01.23 - עלון לצרכן עברית 03.01.23 - עלון לצרכן ערבית 07.06.23 - עלון לצרכן עברית 07.06.23 - עלון לצרכן עברית 24.08.23 - עלון לצרכן אנגלית 24.08.23 - עלון לצרכן עברית 24.08.23 - עלון לצרכן ערבית 07.12.20 - החמרה לעלון 01.03.22 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אג'ובי