Quest for the right Drug
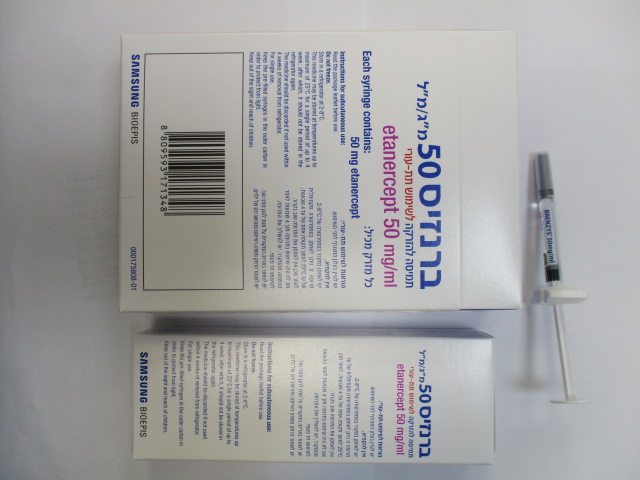
ברנזיס 50 מ"ג/מ"ל BRENZYS 50 MG/ML (ETANERCEPT)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Immunosuppressants, tumour necrosis factor alpha (TNF-α) inhibitors, ATC code: L04AB01 Brenzys is a biosimilar medicinal product, that has been demonstrated to be similar in quality, biological activity, safety and efficacy to the reference medicinal product Enbrel. More detailed information is available on the website of the Ministry of Health http://www.health.gov.il/hozer/dr_127.pdf Tumour necrosis factor (TNF) is a dominant cytokine in the inflammatory process of rheumatoid arthritis. Elevated levels of TNF are also found in the synovium and psoriatic plaques of patients with psoriatic arthritis and in serum and synovial tissue of patients with ankylosing spondylitis. In plaque psoriasis, infiltration by inflammatory cells, including T-cells, leads to increased TNF levels in psoriatic lesions compared with levels in uninvolved skin. Etanercept is a competitive inhibitor of TNF binding to its cell surface receptors, and thereby inhibits the biological activity of TNF. TNF and lymphotoxin are pro-inflammatory cytokines that bind to two distinct cell surface receptors: the 55- kilodalton (p55) and 75-kilodalton (p75) tumour necrosis factor receptors (TNFRs). Both TNFRs exist naturally in membrane-bound and soluble forms. Soluble TNFRs are thought to regulate TNF biological activity. TNF and lymphotoxin exist predominantly as homotrimers, with their biological activity dependent on cross-linking of cell surface TNFRs. Dimeric soluble receptors, such as etanercept, possess a higher affinity for TNF than monomeric receptors and are considerably more potent competitive inhibitors of TNF binding to its cellular receptors. In addition, use of an immunoglobulin Fc region as a fusion element in the construction of a dimeric receptor imparts a longer serum half-life. Mechanism of action Much of the joint pathology in rheumatoid arthritis and ankylosing spondylitis and skin pathology in plaque psoriasis is mediated by pro-inflammatory molecules that are linked in a network controlled by TNF. The mechanism of action of etanercept is thought to be its competitive inhibition of TNF binding to cell surface TNFR, preventing TNF-mediated cellular responses by rendering TNF biologically inactive. Etanercept may also modulate biologic responses controlled by additional downstream molecules (e.g., cytokines, adhesion molecules, or proteinases) that are induced or regulated by TNF. Clinical efficacy and safety This section presents data from four randomised controlled trials in adults with rheumatoid arthritis, one study in adults with psoriatic arthritis, one study in adults with ankylosing spondylitis, one study in adults with non-radiographic axial spondyloarthritis, four studies in adults with plaque psoriasis, three studies in juvenile idiopathic arthritis and one study in paediatric patients with plaque psoriasis. Adult patients with rheumatoid arthritis The efficacy of etanercept was assessed in a randomised, double-blind, placebo-controlled study. The study evaluated 234 adult patients with active rheumatoid arthritis who had failed therapy with at least one but no more than four disease-modifying antirheumatic drugs (DMARDs). Doses of 10 mg or 25 mg etanercept or placebo were administered subcutaneously twice a week for 6 consecutive months. The results of this controlled trial were expressed in percentage improvement in rheumatoid arthritis using American College of Rheumatology (ACR) response criteria. ACR 20 and 50 responses were higher in patients treated with etanercept at 3 and 6 months than in patients treated with placebo (ACR 20: etanercept 62% and 59%, placebo 23% and 11% at 3 and 6 months, respectively: ACR 50: etanercept 41% and 40%, placebo 8% and 5% at months 3 and 6, respectively; p < 0.01 etanercept vs. placebo at all timepoints for both ACR 20 and ACR 50 responses). Approximately 15% of subjects who received etanercept achieved an ACR 70 response at month 3 and month 6 compared to fewer than 5% of subjects in the placebo arm. Among patients receiving etanercept, the clinical responses generally appeared within 1 to 2 weeks after initiation of therapy and nearly always occurred by 3 months. A dose response was seen; results with 10 mg were intermediate between placebo and 25 mg. Etanercept was significantly better than placebo in all components of the ACR criteria, as well as other measures of rheumatoid arthritis disease activity not included in the ACR response criteria, such as morning stiffness. A Health Assessment Questionnaire (HAQ), which included disability, vitality, mental health, general health status, and arthritis-associated health status subdomains, was administered every 3 months during the trial. All subdomains of the HAQ were improved in patients treated with etanercept compared to controls at 3 and 6 months. After discontinuation of etanercept, symptoms of arthritis generally returned within a month. Reintroduction of treatment with etanercept after discontinuation of up to 24 months resulted in the same magnitudes of responses as patients who received etanercept without interruption of therapy based on results of open-label studies. Continued durable responses have been seen for up to 10 years in open-label extension treatment trials when patients received etanercept without interruption. The efficacy of etanercept was compared to methotrexate in a randomised, active-controlled study with blinded radiographic evaluations as a primary endpoint in 632 adult patients with active rheumatoid arthritis (< 3 years duration) who had never received treatment with methotrexate. Doses of 10 mg or 25 mg etanercept were administered subcutaneously (SC) twice a week for up to 24 months. Methotrexate doses were escalated from 7.5 mg/week to a maximum of 20 mg/week over the first 8 weeks of the trial and continued for up to 24 months. Clinical improvement, including onset of action within 2 weeks with etanercept 25 mg, was similar to that seen in the previous trials and was maintained for up to 24 months. At baseline, patients had a moderate degree of disability, with mean HAQ scores of 1.4 to 1.5. Treatment with etanercept 25 mg resulted in substantial improvement at 12 months, with about 44% of patients achieving a normal HAQ score (less than 0.5). This benefit was maintained in Year 2 of this study. In this study, structural joint damage was assessed radiographically and expressed as change in Total Sharp Score (TSS) and its components, the erosion score and Joint Space Narrowing (JSN) score. Radiographs of hands/wrists and feet were read at baseline and 6, 12, and 24 months. The 10 mg etanercept dose had consistently less effect on structural damage than the 25 mg dose. Etanercept 25 mg was significantly superior to methotrexate for erosion scores at both 12 and 24 months. The differences in TSS and JSN were not statistically significant between methotrexate and etanercept 25 mg. The results are shown in the figure below. Radiographic progression: Comparison of etanercept vs. methotrexate in patients with RA of < 3 years duration 2.5 12 Months 2.5 24 Months Change from Baseline 2.2 2.0 2.0 1.5 1.3 1.5 1.3 1.2 1.0 0.9 0.9 0.8 1.0 0.6* 0.6 0.5 0.4* 0.4 0.4 0.5 0.0 0.0 TSS Erosions JSN TSS Erosions JSN MTX Etanercept 25 mg *p < 0.05 In another active-controlled, double-blind, randomised study, clinical efficacy, safety, and radiographic progression in RA patients treated with etanercept alone (25 mg twice weekly), methotrexate alone (7.5 to 20 mg weekly, median dose 20 mg), and the combination of etanercept and methotrexate initiated concurrently were compared in 682 adult patients with active rheumatoid arthritis of 6 months to 20 years duration (median 5 years) who had a less than satisfactory response to at least 1 disease-modifying antirheumatic drug (DMARD) other than methotrexate. Patients in the etanercept in combination with methotrexate therapy group had significantly higher ACR 20, ACR 50, ACR 70 responses and improvement for DAS and HAQ scores at both 24 and 52 weeks than patients in either of the single therapy groups (results shown in table below). Significant advantages for etanercept in combination with methotrexate compared with etanercept monotherapy and methotrexate monotherapy were also observed after 24 months. Clinical Efficacy results at 12 months: Comparison of etanercept vs. methotrexate vs. etanercept in combination with methotrexate in patients with RA of 6 months to 20 years duration Etanercept + Methotrexate Etanercept Endpoint Methotrexate (n = 228) (n = 223) (n = 231) ACR ACR 20 58.8% 65.5% 74.5%†, Φ Responsesa ACR 50 36.4% 43.0% 63.2%†, Φ ACR 70 16.7% 22.0% 39.8%†, Φ DAS (Scoreb) Baseline 5.5 5.7 5.5 (Scoreb) Week 52 3.0 3.0 2.3†, Φ c Remission 14% 18% 37%†, Φ HAQ Baseline 1.7 1.7 1.8 Week 52 1.1 1.0 0.8†, Φ a Patients who did not complete 12 months in the study were considered to be non-responders. b Values for Disease Activity Score (DAS) are means. c Remission is defined as DAS <1.6. Pairwise comparison p-values: † = p < 0.05 for comparisons of etanercept + methotrexate vs. methotrexate and Φ = p < 0.05 for comparisons of etanercept + methotrexate vs. etanercept. Radiographic progression at 12 months was significantly less in the etanercept group than in the methotrexate group, while the combination was significantly better than either monotherapy at slowing radiographic progression (see figure below). Radiographic progression: Comparison of etanercept vs. methotrexate vs. etanercept in combination with methotrexate in patients with RA of 6 months to 20 years duration (12 month results) Methotrexate 3.0 2.80 Etanercept 2.5 Etanercept + Methotrexate Change from Baseline 2.0 1.68 1.5 1.12 1.0 0.52* 0.5 0.21* 0.32 0.0 -0.5 -0.30† -0.23†, Φ †, Φ -0.54 -1.0 TSS Erosions JSN Pairwise comparison p-values: * = p < 0.05 for comparisons of etanercept vs.methotrexate, † = p < 0.05 for comparisons of etanercept + methotrexate vs. methotrexate and Φ = p < 0.05 for comparisons of etanercept + methotrexate vs. etanercept. Significant advantages for etanercept in combination with methotrexate compared with etanercept monotherapy and methotrexate monotherapy were also observed after 24 months. Similarly, the significant advantages for etanercept monotherapy compared with methotrexate monotherapy were also observed after 24 months. In an analysis in which all patients who dropped out of the study for any reason were considered to have progressed, the percentage of patients without progression (TSS change ≤ 0.5) at 24 months was higher in the etanercept in combination with methotrexate group compared with the etanercept alone and methotrexate alone groups (62%, 50%, and 36%, respectively; p < 0.05). The difference between etanercept alone and methotrexate alone was also significant (p < 0.05). Among patients who completed a full 24 months of therapy in the study, the non-progression rates were 78%, 70%, and 61%, respectively. The safety and efficacy of 50 mg etanercept (two 25 mg SC injections) administered once weekly were evaluated in a double-blind, placebo-controlled study of 420 patients with active RA. In this study, 53 patients received placebo, 214 patients received 50 mg etanercept once weekly and 153 patients received 25 mg etanercept twice weekly. The safety and efficacy profiles of the two etanercept treatment regimens were comparable at week 8 in their effect on signs and symptoms of RA; data at week 16 did not show comparability (non-inferiority) between the two regimens. A single 50 mg/ml injection of etanercept was found to be bioequivalent to two simultaneous injections of 25 mg/ml. Adult patients with psoriatic arthritis The efficacy of etanercept was assessed in a randomised, double-blind, placebo-controlled study in 205 patients with psoriatic arthritis. Patients were between 18 and 70 years of age and had active psoriatic arthritis (≥ 3 swollen joints and ≥ 3 tender joints) in at least one of the following forms: (1) distal interphalangeal (DIP) involvement; (2) polyarticular arthritis (absence of rheumatoid nodules and presence of psoriasis); (3) arthritis mutilans; (4) asymmetric psoriatic arthritis; or (5) spondylitis- like ankylosis. Patients also had plaque psoriasis with a qualifying target lesion ≥ 2 cm in diameter. Patients had previously been treated with NSAIDs (86%), DMARDs (80%), and corticosteroids (24%). Patients currently on methotrexate therapy (stable for ≥ 2 months) could continue at a stable dose of ≤ 25 mg/week methotrexate. Doses of 25 mg of etanercept (based on dose-finding studies in patients with rheumatoid arthritis) or placebo were administered SC twice a week for 6 months. At the end of the double-blind study, patients could enter a long-term open-label extension study for a total duration of up to 2 years. Clinical responses were expressed as percentages of patients achieving the ACR 20, 50, and 70 response and percentages with improvement in Psoriatic Arthritis Response Criteria (PsARC). Results are summarised in the table below. Responses of patients with psoriatic arthritis in a placebo-controlled trial Percent of Patients Psoriatic Arthritis Response Placebo Etanercepta n = 104 n = 101 ACR 20 Month 3 15 59b Month 6 13 50b ACR 50 Month 3 4 38b Month 6 4 37b ACR 70 Month 3 0 11b Month 6 1 9c PsARC Month 3 31 72b Month 6 23 70b a 25 mg etanercept SC twice weekly b p < 0.001, etanercept vs. placebo c p < 0.01, etanercept vs. placebo Among patients with psoriatic arthritis who received etanercept, the clinical responses were apparent at the time of the first visit (4 weeks) and were maintained through 6 months of therapy. Etanercept was significantly better than placebo in all measures of disease activity (p < 0.001), and responses were similar with and without concomitant methotrexate therapy. Quality of life in psoriatic arthritis patients was assessed at every timepoint using the disability index of the HAQ. The disability index score was significantly improved at all timepoints in psoriatic arthritis patients treated with etanercept, relative to placebo (p < 0.001). Radiographic changes were assessed in the psoriatic arthritis study. Radiographs of hands and wrists were obtained at baseline and months 6, 12, and 24. The modified TSS at 12 months is presented in the table below. In an analysis in which all patients who dropped out of the study for any reason were considered to have progressed, the percentage of patients without progression (TSS change ≤ 0.5) at 12 months was higher in the etanercept group compared with the placebo group (73% vs. 47%, respectively, p ≤ 0.001). The effect of etanercept on radiographic progression was maintained in patients who continued on treatment during the second year. The slowing of peripheral joint damage was observed in patients with polyarticular symmetrical joint involvement. Mean (SE) annualized change from baseline in total sharp score Placebo Etanercept Time (n = 104) (n = 101) Month 12 1.00 (0.29) -0.03 (0.09)a SE = standard error a p = 0.0001 Etanercept treatment resulted in improvement in physical function during the double-blind period, and this benefit was maintained during the longer-term exposure of up to 2 years. There is insufficient evidence of the efficacy of etanercept in patients with ankylosing spondylitis-like and arthritis mutilans psoriatic arthropathies due to the small number of patients studied. No study has been performed in patients with psoriatic arthritis using the 50 mg once-weekly dosing regimen. Evidence of efficacy for the once-weekly dosing regimen in this patient population has been based on data from the study in patients with ankylosing spondylitis. Adult patients with ankylosing spondylitis The efficacy of etanercept in ankylosing spondylitis was assessed in 3 randomised, double-blind studies comparing twice-weekly administration of 25 mg etanercept with placebo. A total of 401 patients were enrolled, from which 203 were treated with etanercept. The largest of these trials (n = 277) enrolled patients who were between 18 and 70 years of age and had active ankylosing spondylitis defined as visual analog scale (VAS) scores of ≥ 30 for average of duration and intensity of morning stiffness plus VAS scores of ≥ 30 for at least 2 of the following 3 parameters: patient global assessment; average of VAS values for nocturnal back pain and total back pain; average of 10 questions on the Bath Ankylosing Spondylitis Functional Index (BASFI). Patients receiving DMARDs, NSAIDS, or corticosteroids could continue them on stable doses. Patients with complete ankylosis of the spine were not included in the study. Doses of 25 mg of etanercept (based on dose- finding studies in patients with rheumatoid arthritis) or placebo were administered subcutaneously twice a week for 6 months in 138 patients. The primary measure of efficacy (ASAS 20) was a ≥ 20% improvement in at least 3 of the 4 Assessment in Ankylosing Spondylitis (ASAS) domains (patient global assessments, back pain, BASFI, and inflammation) and absence of deterioration in the remaining domain. ASAS 50 and 70 responses used the same criteria with a 50% improvement or a 70% improvement, respectively. Compared to placebo, treatment with etanercept resulted in significant improvements in the ASAS 20, ASAS 50 and ASAS 70 as early as 2 weeks after the initiation of therapy. Responses of patients with ankylosing spondylitis in a placebo-controlled trial Percent of Patients Placebo Etanercept Ankylosing Spondylitis Response n = 139 n = 138 ASAS 20 2 weeks 22 46a 3 months 27 60a 6 months 23 58a ASAS 50 2 weeks 7 24a 3 months 13 45a 6 months 10 42a ASAS 70 2 weeks 2 12b 3 months 7 29b 6 months 5 28b a p < 0.001, etanercept vs. placebo b p = 0.002, etanercept vs. placebo Among patients with ankylosing spondylitis who received etanercept, the clinical responses were apparent at the time of the first visit (2 weeks) and were maintained through 6 months of therapy. Responses were similar in patients who were or were not receiving concomitant therapies at baseline. Similar results were obtained in the 2 smaller ankylosing spondylitis trials. In a fourth study, the safety and efficacy of 50 mg etanercept (two 25 mg SC injections) administered once weekly vs. 25 mg etanercept administered twice weekly were evaluated in a double-blind, placebo-controlled study of 356 patients with active ankylosing spondylitis. The safety and efficacy profiles of the 50 mg once-weekly and 25 mg twice-weekly regimens were similar. Adult patients with non-radiographic axial spondyloarthritis The efficacy of etanercept in patients with non-radiographic axial spondyloarthritis (nr-AxSpa) was assessed in a randomised, 12-week double-blind, placebo-controlled study. The study evaluated 215 adult patients (modified intent-to-treat population) with active nr-AxSpa (18 to 49 years of age), defined as those patients meeting the ASAS classification criteria of axial spondyloarthritis but did not meet the modified New York criteria for AS. Patients were also required to have an inadequate response or intolerance to two or more NSAIDs. In the double-blind period, patients received etanercept 50 mg weekly or placebo for 12 weeks. The primary measure of efficacy (ASAS 40) was a 40% improvement in at least three of the four ASAS domains and absence of deterioration in the remaining domain. The double-blind period was followed by an open-label period during which all patients receive etanercept 50 mg weekly for up to an additional 92 weeks. MRIs of the sacroiliac joint and spine were obtained to assess inflammation at baseline and at weeks 12 and 104. Compared to placebo, treatment with etanercept resulted in statistically significant improvement in the ASAS 40, ASAS 20 and ASAS 5/6. Significant improvement was also observed for the ASAS partial remission and BASDAI 50. Week 12 results are shown in the table below. Efficacy response in placebo-controlled nr-AxSpa study: Percent of patients achieving endpoints Double-Blind Clinical Placebo Etanercept Responses at Week 12 n = 106 to 109* n = 103 to 105* ASAS** 40 15.7 32.4b ASAS 20 36.1 52.4c ASAS 5/6 10.4 33.0a ASAS partial remission 11.9 24.8c BASDAI***50 23.9 43.8b *Some patients did not provide complete data for each endpoint **ASAS=Assessments in Spondyloarthritis International Society ***Bath Ankylosing Spondylitis Disease Activity Index a : p < 0.001, b: < 0.01 and c: < 0.05, respectively between etanercept and placebo At week 12, there was a statistically significant improvement in the SPARCC (Spondyloarthritis Research Consortium of Canada) score for the sacroiliac joint (SIJ) as measured by MRI for patients receiving etanercept. Adjusted mean change from baseline was 3.8 for etanercept treated (n = 95) versus 0.8 for placebo treated (n = 105) patients (p < 0.001). At week 104, the mean change from baseline in the SPARCC score measured on MRI for all etanercept-treated subjects was 4.64 for the SIJ (n=153) and 1.40 the spine (n=154). Etanercept showed statistically significantly greater improvement from baseline to week 12 compared to placebo in most health-related quality of life and physical function assessments, including BASFI (Bath Ankylosing Spondylitis Functional Index), EuroQol 5D Overall Health State Score and SF-36 Physical Component Score. Clinical responses among nr-AxSpa patients who received etanercept were apparent at the time of the first visit (2 weeks) and were maintained through 2 years of therapy. Improvements in health-related quality of life and physical function were also maintained through 2 years of therapy. The 2 year data did not reveal any new safety findings. At week 104, 8 subjects had progressed to a score of bilateral Grade 2 on spinal X-ray according to the modified New York Radiological Grade, indicative of axial spondyloarthropathy. Adult patients with plaque psoriasis Etanercept is recommended for use in patients as defined in section 4.1. Patients who “failed to respond to” in the target population is defined by insufficient response (PASI < 50 or PGA less than good), or worsening of the disease while on treatment, and who were adequately dosed for a sufficiently long duration to assess response with at least each of the three major systemic therapies as available. The efficacy of etanercept versus other systemic therapies in patients with moderate to severe psoriasis (responsive to other systemic therapies) has not been evaluated in studies directly comparing etanercept with other systemic therapies. Instead, the safety and efficacy of etanercept were assessed in four randomised, double-blind, placebo-controlled studies. The primary efficacy endpoint in all four studies was the proportion of patients in each treatment group who achieved the PASI 75 (i.e., at least a 75% improvement in the Psoriasis Area and Severity Index score from baseline) at 12 weeks. Study 1 was a Phase 2 study in patients with active, but clinically stable, plaque psoriasis involving ≥ 10% of the body surface area who were ≥ 18 years old. One hundred and twelve (112) patients were randomised to receive a dose of 25 mg of etanercept (n = 57) or placebo (n = 55) twice a week for 24 weeks. Study 2 evaluated 652 patients with chronic plaque psoriasis using the same inclusion criteria as study 1 with the addition of a minimum psoriasis area and severity index (PASI) of 10 at screening. Etanercept was administered at doses of 25 mg once a week, 25 mg twice a week or 50 mg twice a week for 6 consecutive months. During the first 12 weeks of the double-blind treatment period, patients received placebo or one of the above three etanercept doses. After 12 weeks of treatment, patients in the placebo group began treatment with blinded etanercept (25 mg twice a week); patients in the active treatment groups continued to week 24 on the dose to which they were originally randomised. Study 3 evaluated 583 patients and had the same inclusion criteria as study 2. Patients in this study received a dose of 25 mg or 50 mg etanercept, or placebo twice a week for 12 weeks and then all patients received open-label 25 mg etanercept twice weekly for an additional 24 weeks. Study 4 evaluated 142 patients and had similar inclusion criteria to studies 2 and 3. Patients in this study received a dose of 50 mg etanercept or placebo once weekly for 12 weeks and then all patients received open-label 50 mg etanercept once weekly for an additional 12 weeks. In study 1, the etanercept-treated group had a significantly higher proportion of patients with a PASI 75 response at week 12 (30%) compared to the placebo-treated group (2%) (p < 0.0001). At 24 weeks, 56% of patients in the etanercept-treated group had achieved the PASI 75 compared to 5% of placebo- treated patients. Key results of studies 2, 3 and 4 are shown below. Responses of patients with psoriasis in studies 2, 3 and 4 Study 2 Study 3 Study 4 Etanercept Etanercept Etanercept Placeb Placeb 25 m 50 m 50 m 50 25 mg Placebo o 50 mg BIW o g g g mg Response BIW BIW BIW QW QW (%) n= n= n= n= n= n= n= n= n= n = 193 n = 46 166 162 162 164 164 196 196 96 90 wk wk wk wk wk wk wk wk wk 12 wk 12 wk 12 12 24a 12 24a 12 12 12 24a PASI 50 14 58* 70 74* 77 9 64 * 77* 9 69* 83 PASI 75 4 34* 44 49* 59 3 34 * 49* 2 38* 71 DSGAb, clear or 5 34* 39 49* 55 4 39* 57* 4 39* 64 almost clear * p ≤ 0.0001 compared with placebo a No statistical comparisons to placebo were made at week 24 in studies 2 and 4 because the original placebo group began receiving etanercept 25 mg BIW or 50 mg once weekly from week 13 to week 24. b Dermatologist Static Global Assessment. Clear or almost clear defined as 0 or 1 on a 0 to 5 scale. Among patients with plaque psoriasis who received etanercept, significant responses relative to placebo were apparent at the time of the first visit (2 weeks) and were maintained through 24 weeks of therapy. Study 2 also had a drug withdrawal period during which patients who achieved a PASI improvement of at least 50% at week 24 had treatment stopped. Patients were observed off treatment for the occurrence of rebound (PASI ≥ 150% of baseline) and for the time to relapse (defined as a loss of at least half of the improvement achieved between baseline and week 24). During the withdrawal period, symptoms of psoriasis gradually returned, with a median time to disease relapse of 3 months. No rebound flare of disease and no psoriasis-related serious adverse events were observed. There was some evidence to support a benefit of re-treatment with etanercept in patients initially responding to treatment. In study 3, the majority of patients (77%) who were initially randomised to 50 mg twice weekly and had their etanercept dose decreased at week 12 to 25 mg twice weekly maintained their PASI 75 response through week 36. For patients who received 25 mg twice weekly throughout the study, the PASI 75 response continued to improve between weeks 12 and 36. In study 4, the etanercept-treated group had a higher proportion of patients with PASI 75 at week 12 (38%) compared to the placebo-treated group (2%) (p<0.0001). For patients who received 50 mg once weekly throughout the study, the efficacy responses continued to improve with 71% achieving PASI 75 at week 24. In long-term (up to 34 months) open-label studies where etanercept was given without interruption, clinical responses were sustained and safety was comparable to shorter-term studies. An analysis of clinical trial data did not reveal any baseline disease characteristics that would assist clinicians in selecting the most appropriate dosing option (intermittent or continuous). Consequently, the choice of intermittent or continuous therapy should be based upon physician judgment and individual patient needs. Antibodies to etanercept Antibodies to etanercept have been detected in the sera of some subjects treated with etanercept. These antibodies have generally been non-neutralising and transient. There appears to be no correlation between antibody development and clinical response or adverse events. Paediatric population Paediatric patients with juvenile idiopathic arthritis The safety and efficacy of etanercept were assessed in a two-part study in 69 children with polyarticular-course juvenile idiopathic arthritis who had a variety of juvenile idiopathic arthritis onset types (polyarthritis, pauciarthritis, systemic onset). Patients aged 4 to 17 years with moderately to severely active polyarticular-course juvenile idiopathic arthritis refractory to, or intolerant of, methotrexate were enrolled; patients remained on a stable dose of a single nonsteroidal anti- inflammatory drug and/or prednisone (< 0.2 mg/kg/day or 10 mg maximum). In part 1, all patients received 0.4 mg/kg (maximum 25 mg per dose) etanercept subcutaneously twice weekly. In part 2, patients with a clinical response at day 90 were randomised to remain on etanercept or receive placebo for four months and assessed for disease flare. Responses were measured using the ACR Pedi 30, defined as 30% improvement in at least three of six and 30% worsening in no more than one of six JRA core set criteria, including active joint count, limitation of motion, physician and patient/parent global assessments, functional assessment, and erythrocyte sedimentation rate (ESR). Disease flare was defined as a 30% worsening in three of six JRA core set criteria and 30% improvement in not more than one of the six JRA core set criteria and a minimum of two active joints. In part 1 of the study, 51 of 69 (74%) patients demonstrated a clinical response and entered part 2. In part 2, 6 of 25 (24%) patients remaining on etanercept experienced a disease flare compared to 20 of 26 (77%) patients receiving placebo (p = 0.007). From the start of part 2, the median time to flare was 116 days for patients who received etanercept and 28 days for patients who received placebo. Of patients who demonstrated a clinical response at 90 days and entered part 2 of the study, some of the patients remaining on etanercept continued to improve from month 3 through month 7, while those who received placebo did not improve. In an open-label, safety extension study, 58 paediatric patients from the above study (from the age of 4 years at time of enrolment) continued to receive etanercept for up to 10 years. Rates of serious adverse events and serious infections did not increase with long-term exposure. Long-term safety of etanercept monotherapy (n = 103), etanercept plus methotrexate (n = 294), or methotrexate monotherapy (n = 197) were assessed for up to 3 years in a registry of 594 children aged 2 to 18 years with juvenile idiopathic arthritis, 39 of whom were 2 to 3 years of age. Overall, infections were more commonly reported in patients treated with etanercept compared to methotrexate alone (3.8 versus 2%), and the infections associated with etanercept use were of a more severe nature. In another open-label single-arm study, 60 patients with extended oligoarthrits (15 patients aged 2 to 4, 23 patients aged 5 to 11 and 22 patients aged 12 to 17 years old), 38 patients with enthesitis-related arthritis (12 to 17 years old), and 29 patients with psoriatic arthritis (12 to 17 years old) were treated with etanercept at a dose of 0.8 mg/kg (up to a maximum of 50 mg per dose) administered weekly for 12 weeks. In each of the JIA subtypes, the majority of patients met ACR Pedi 30 criteria and demonstrated clinical improvement in secondary endpoints such as number of tender joints and physician global assessment. The safety profile was consistent with that observed in other JIA studies. Studies have not been done in patients with juvenile idiopathic arthritis to assess the effects of continued etanercept therapy in patients who do not respond within 3 months of initiating etanercept therapy. Additionally, studies have not been conducted to assess the effects of discontinuing or reducing the recommended dose of etanercept following its long-term use in patients with JIA. Paediatric patients with plaque psoriasis The efficacy of etanercept was assessed in a randomised, double-blind, placebo-controlled study in 211 paediatric patients aged 4 to 17 years with moderate to severe plaque psoriasis (as defined by an sPGA score ≥ 3, involving ≥ 10% of the BSA, and PASI ≥ 12). Eligible patients had a history of receiving phototherapy or systemic therapy, or were inadequately controlled on topical therapy. Patients received etanercept 0.8 mg/kg (up to 50 mg) or placebo once weekly for 12 weeks. At week 12, more patients randomised to etanercept had positive efficacy responses (e.g., PASI 75) than those randomised to placebo. Paediatric Plaque Psoriasis Outcomes at 12 Weeks Etanercept 0.8 mg/kg Once Placebo Weekly (N = 105) (N = 106) PASI 75, n (%) 60 (57%)a 12 (11%) PASI 50, n (%) 79 (75%)a 24 (23%) sPGA “clear” or “minimal”, n (%) 56 (53%)a 14 (13%) Abbreviation: sPGA-static Physician Global Assessment a p < 0.0001 compared with placebo After the 12-week double-blind treatment period, all patients received etanercept 0.8 mg/kg (up to 50 mg) once weekly for additional 24 weeks. Responses observed during the open-label period were similar to those observed in the double-blind period. During a randomised withdrawal period, significantly more patients re-randomised to placebo experienced disease relapse (loss of PASI 75 response) compared with patients re-randomised to etanercept. With continued therapy, responses were maintained up to 48 weeks. The long-term safety and effectiveness of etanercept 0.8 mg/kg (up to 50 mg) once weekly was assessed in an open-label extension study of 181 paediatric subjects with plaque psoriasis for up to 2 years beyond the 48 week study discussed above. Long-term experience with etanercept was generally comparable to the original 48-week study and did not reveal any new safety findings.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Etanercept serum values were determined by an Enzyme-Linked Immunosorbent Assay (ELISA) method, which may detect ELISA-reactive degradation products, as well as the parent compound. Absorption Etanercept is slowly absorbed from the site of subcutaneous injection, reaching maximum concentration approximately 48 hours after a single dose. The absolute bioavailability is 76%. With twice-weekly doses, it is anticipated that steady-state concentrations are approximately twice as high as those observed after single doses. After a single subcutaneous dose of 25 mg etanercept, the average maximum serum concentration observed in healthy volunteers was 1.65 ± 0.66 μg/ml, and the area under the curve was 235 ± 96.6 μg × hr/ml. Mean serum concentration profiles at steady state in treated RA patients were Cmax of 2.4 mg/l vs. 2.6 mg/l, Cmin of 1.2 mg/l vs. 1.4 mg/l, and partial AUC of 297 mg × hr/l vs. 316 mg × hr/l for 50 mg etanercept once weekly (n = 21) vs. 25 mg etanercept twice weekly (n = 16), respectively. In an open-label, single-dose, two-treatment, crossover study in healthy volunteers, etanercept administered as a single 50 mg/ml injection was found to be bioequivalent to two simultaneous injections of 25 mg/ml. In a population pharmacokinetics analysis in ankylosing spondylitis patients, the etanercept steady state AUCs were 466 μg × hr/ml and 474 μg × hr/ml for 50 mg etanercept once weekly (n = 154) and 25 mg twice weekly (n = 148), respectively. Distribution A biexponential curve is required to describe the concentration time curve of etanercept. The central volume of distribution of etanercept is 7.6 L, while the volume of distribution at steady-state is 10.4 L. Elimination Etanercept is cleared slowly from the body. The half-life is long, approximately 70 hours. Clearance is approximately 0.066 l/hr in patients with rheumatoid arthritis, somewhat lower than the value of 0.11 l/hr observed in healthy volunteers. Additionally, the pharmacokinetics of etanercept in rheumatoid arthritis patients, ankylosing spondylitis and plaque psoriasis patients are similar. There is no apparent pharmacokinetic difference between males and females. Linearity Dose proportionality has not been formally evaluated, but there is no apparent saturation of clearance across the dosing range. Special populations Renal impairment Although there is elimination of radioactivity in urine after administration of radiolabelled etanercept to patients and volunteers, increased etanercept concentrations were not observed in patients with acute renal failure. The presence of renal impairment should not require a change in dosage. Hepatic impairment Increased etanercept concentrations were not observed in patients with acute hepatic failure. The presence of hepatic impairment should not require a change in dosage. Elderly The impact of advanced age was studied in the population pharmacokinetic analysis of etanercept serum concentrations. Clearance and volume estimates in patients aged 65 to 87 years were similar to estimates in patients less than 65 years of age. Paediatric population Paediatric patients with juvenile idiopathic arthritis In a polyarticular-course juvenile idiopathic arthritis trial with etanercept, 69 patients (aged 4 to 17 years) were administered 0.4 mg etanercept/kg twice weekly for three months. Serum concentration profiles were similar to those seen in adult rheumatoid arthritis patients. The youngest children (4 years of age) had reduced clearance (increased clearance when normalised by weight) compared with older children (12 years of age) and adults. Simulation of dosing suggests that while older children (10-17 years of age) will have serum levels close to those seen in adults, younger children will have appreciably lower levels. Paediatric patients with plaque psoriasis Patients with paediatric plaque psoriasis (aged 4 to 17 years) were administered 0.8 mg/kg (up to a maximum dose of 50 mg per week) of etanercept once weekly for up to 48 weeks. The mean serum steady-state trough concentrations ranged from 1.6 to 2.1 mcg/ml at weeks 12, 24, and 48. These mean concentrations in patients with paediatric plaque psoriasis were similar to the concentrations observed in patients with juvenile idiopathic arthritis (treated with 0.4 mg/kg etanercept twice weekly, up to maximum dose of 50 mg per week). These mean concentrations were similar to those seen in adult patients with plaque psoriasis treated with 25 mg etanercept twice-weekly.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול בחולה הסובל מאחד מאלה: א. ארתריטיס ראומטואידית - כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת, בכפוף לתנאי פסקה 3; ב. ארתריטיס כרוני בצעירים (Juvenile chronic arthritis) - בקטינים שמלאו להם 4 שנים וטרם מלאו להם 17 שנים הסובלים ממהלך מחלה רב מפרקי פעיל ושלא הגיבו לטיפול ב-methotrexate או שאינם מסוגלים לקבל טיפול כאמור; ג. דלקת מפרקים פסוריאטית קשה כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת ולאחר כשלון או אי סבילות ל-salazopyrin או methotrexate; ד. אנקילוזינג ספונדילטיס קשה אם החולה לא הגיב לטיפול קונבנציונלי; במקרה של הוריאנט דמוי אנקילוזינג ספונדיליטיס הקשור בפסוריאזיס, תהיה ההוריה כמו באנקילוזינג ספונדיליטיס ראשונית; ה. פסוריאזיס מלווה בוריאנט דמוי אנקילוזינג ספונדיליטיס, אם החולה לא הגיב לטיפול קונבנציונלי; ו. פסוריאזיס - בהתקיים כל אלה: 1. החולה סובל מאחד מאלה: א. מחלה מפושטת מעל ל-50% של שטח גוף או PASI מעל 50. ב. נגעים באזורי גוף רגישים - אזורים אלו יכללו פנים, צוואר, קיפולי עור, כפות ידיים, כפות רגליים, אזור הגניטליה והישבן;2. החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור של 50% לפחות ב-PASI לאחר סיום הטיפול בהשוואה לתחילת הטיפול; בהתייחס לחולה העונה על האמור בפסקת משנה (1)(ב) - החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור משמעותי לאחר סיום הטיפול בהשוואה לתחילת הטיפול; 3. התרופה תינתן על פי מרשם של רופא מומחה בדרמטולוגיה. 3. הטיפול בתרופה לחולה העונה על תנאי פסקה (1) (א), יינתן בהתקיים כל אלה: 1. קיימת עדות לדלקת פרקים (RA-Rheumatoid Arthritis) פעילה המתבטאת בשלושה מתוך אלה: א. מחלה דלקתית (כולל כאב ונפיחות) בארבעה פרקים ויותר; ב. שקיעת דם או CRP החורגים מהנורמה באופן משמעותי (בהתאם לגיל החולה); ג. שינויים אופייניים ל-RA בצילומי רנטגן של הפרקים הנגועים; ד. פגיעה תפקודית המוגדרת כהגבלה משמעותית בתפקודו היומיומי של החולה ובפעילותו בעבודה. 2. לאחר מיצוי הטיפול בתרופות השייכות למשפחת ה-NSAIDs ובתרופות השייכות למשפחת ה-DMARDs. לעניין זה יוגדר מיצוי הטיפול כהעדר תגובה קלינית לאחר טיפול קו ראשון בתרופות אנטי דלקתיות ממשפחת ה-NSAIDs וטיפול קו שני ב-3 תרופות לפחות ממשפחת ה-DMARDs שאחת מהן מתוטרקסאט, במשך 3 חודשים רצופים לפחות. 3. הטיפול יינתן באישור רופא מומחה בראומטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| juvenile idiopathic rheumatoid arthritis | ADALIMUMAB, ETANERCEPT | |||
| Psoriatic arthritis | ADALIMUMAB, ETANERCEPT, INFLIXIMAB, USTEKINUMAB, SECUKINUMAB | |||
| Psoriasis | ADALIMUMAB, ALEFACEPT, ETANERCEPT, INFLIXIMAB, EFALIZUMAB, USTEKINUMAB, SECUKINUMAB, IXEKIZUMAB | |||
| Rheumatoid arthritis | ETANERCEPT, INFLIXIMAB, ABATACEPT, TOCILIZUMAB, TOFACITINIB, CERTOLIZUMAB PEGOL, SARILUMAB | |||
| Ankylosing spondylitis | ADALIMUMAB, ETANERCEPT, INFLIXIMAB, USTEKINUMAB, SECUKINUMAB, CERTOLIZUMAB PEGOL |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
