Quest for the right Drug
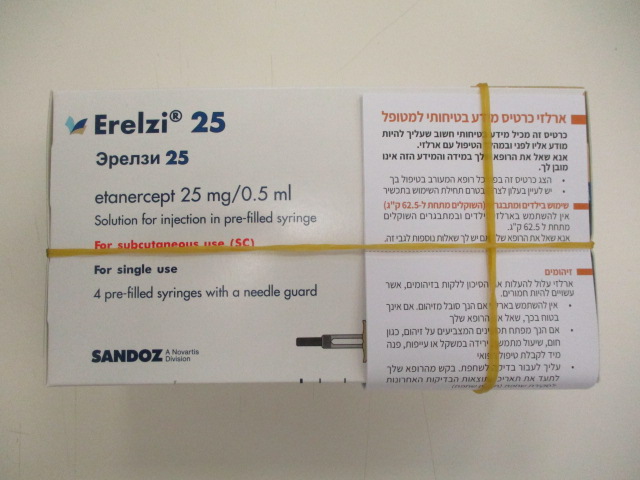
ארלזי 25 ERELZI 25 (ETANERCEPT)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תת-עורי : S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use In order to improve the traceability of biological medicinal products, it is advised that the trademark and the batch number of the administered product should be clearly recorded (or stated) in the patient file. Infections Patients should be evaluated for infections before, during, and after treatment with Erelzi, taking into consideration that the mean elimination half-life of etanercept is approximately 70 hours (range 7 to 300 hours). Serious infections, sepsis, tuberculosis, and opportunistic infections, including invasive fungal infections, listeriosis and legionellosis, have been reported with the use of etanercept (see section 4.8). These infections were due to bacteria, mycobacteria, fungi, viruses and parasites (including protozoa). In some cases, particular fungal and other opportunistic infections have not been recognised, resulting in delay of appropriate treatment and sometimes death. In evaluating patients for infections, the patient’s risk for relevant opportunistic infections (e.g., exposure to endemic mycoses) should be considered. Patients who develop a new infection while undergoing treatment with Erelzi should be monitored closely. Administration of Erelzi should be discontinued if a patient develops a serious infection. The safety and efficacy of etanercept in patients with chronic infections have not been evaluated. Physicians should exercise caution when considering the use of Erelzi in patients with a history of recurring or chronic infections or with underlying conditions that may predispose patients to infections, such as advanced or poorly controlled diabetes. Tuberculosis Cases of active tuberculosis, including miliary tuberculosis and tuberculosis with extra- pulmonary location, have been reported in patients treated with etanercept. Before starting treatment with Erelzi, all patients must be evaluated for both active and inactive (‘latent’) tuberculosis. This evaluation should include a detailed medical history with personal history of tuberculosis or possible previous contact with tuberculosis and previous and/or current immunosuppressive therapy. Appropriate screening tests, i.e., tuberculin skin test and chest X-ray, should be performed in all patients (local recommendations may apply). It is recommended that the conduct of these tests should be recorded in the Patient Safety Information Card. Prescribers are reminded of the risk of false negative tuberculin skin test results, especially in patients who are severely ill or immunocompromised. If active tuberculosis is diagnosed, Erelzi therapy must not be initiated. If inactive (‘latent’) tuberculosis is diagnosed, treatment for latent tuberculosis must be started with anti-tuberculosis therapy before the initiation of Erelzi, and in accordance with local recommendations. In this situation, the benefit/risk balance of Erelzi therapy should be very carefully considered. All patients should be informed to seek medical advice if signs/symptoms suggestive of tuberculosis (e.g., persistent cough, wasting/weight loss, low-grade fever) appear during or after Erelzi treatment. Hepatitis B reactivation Reactivation of hepatitis B in patients who were previously infected with the hepatitis B virus (HBV) and had received concomitant TNF-antagonists, including etanercept, has been reported. This includes reports of reactivation of hepatitis B in patients who were anti-HBc positive but HBsAg negative. Patients should be tested for HBV infection before initiating treatment with Erelzi. For patients who test positive for HBV infection, consultation with a physician with expertise in the treatment of hepatitis B is recommended. Caution should be exercised when administering Erelzi in patients previously infected with HBV. These patients should be monitored for signs and symptoms of active HBV infection throughout therapy and for several weeks following termination of therapy. Adequate data from treating patients infected with HBV with anti-viral therapy in conjunction with TNF- antagonist therapy are not available. In patients who develop HBV infection, Erelzi should be stopped and effective anti-viral therapy with appropriate supportive treatment should be initiated. Worsening of hepatitis C There have been reports of worsening of hepatitis C in patients receiving etanercept. Erelzi should be used with caution in patients with a history of hepatitis C. Concurrent treatment with anakinra Concurrent administration of etanercept and anakinra has been associated with an increased risk of serious infections and neutropenia compared to etanercept alone. This combination has not demonstrated increased clinical benefit. Thus, the combined use of Erelzi and anakinra is not recommended (see sections 4.5 and 4.8). Concurrent treatment with abatacept In clinical studies, concurrent administration of abatacept and etanercept resulted in increased incidences of serious adverse events. This combination has not demonstrated increased clinical benefit; such use is not recommended (see section 4.5). Allergic reactions Allergic reactions associated with etanercept administration have been reported commonly. Allergic reactions have included angioedema and urticaria; serious reactions have occurred. If any serious allergic or anaphylactic reaction occurs, Erelzi therapy should be discontinued immediately and appropriate therapy initiated. Immunosuppression The possibility exists for TNF-antagonists, including Erelzi, to affect host defences against infections and malignancies since TNF mediates inflammation and modulates cellular immune responses. In a study of 49 adult patients with rheumatoid arthritis treated with etanercept, there was no evidence of depression of delayed-type hypersensitivity, depression of immunoglobulin levels, or change in enumeration of effector cell populations. Two juvenile idiopathic arthritis patients developed varicella infection and signs and symptoms of aseptic meningitis, which resolved without sequelae. Patients with a significant exposure to varicella virus should temporarily discontinue Erelzi therapy and be considered for prophylactic treatment with Varicella Zoster Immune Globulin. The safety and efficacy of etanercept in patients with immunosuppression have not been evaluated. Malignancies and lymphoproliferative disorders Solid and haematopoietic malignancies (excluding skin cancers) Reports of various malignancies (including breast and lung carcinoma and lymphoma) have been received in the post-marketing period (see section 4.8). In the controlled portions of clinical trials of TNF-antagonists, more cases of lymphoma have been observed among patients receiving a TNF-antagonist compared with control patients. However, the occurrence was rare, and the follow-up period of placebo patients was shorter than for patients receiving TNF-antagonist therapy. In the postmarketing setting, cases of leukaemia have been reported in patients treated with TNF-antagonists. There is an increased background risk for lymphoma and leukaemia in rheumatoid arthritis patients with long-standing, highly active, inflammatory disease, which complicates risk estimation. Based on current knowledge, a possible risk for the development of lymphomas, leukaemia or other haematopoietic or solid malignancies in patients treated with a TNF- antagonist cannot be excluded. Caution should be exercised when considering TNF- antagonist therapy for patients with a history of malignancy or when considering continuing treatment in patients who develop a malignancy. Malignancies, some fatal, have been reported among children, adolescents and young adults (up to 22 years of age) treated with TNF-antagonists (initiation of therapy ≤ 18 years of age), including etanercept, in the postmarketing setting. Approximately half the cases were lymphomas. The other cases represented a variety of different malignancies and included rare malignancies typically associated with immunosuppression. A risk for the development of malignancies in children and adolescents treated with TNF-antagonists cannot be excluded. Skin cancers Melanoma and non-melanoma skin cancer (NMSC) have been reported in patients treated with TNF-antagonists, including etanercept. Postmarketing cases of Merkel cell carcinoma have been reported very infrequently in patients treated with etanercept. Periodic skin examination is recommended for all patients, particularly those with risk factors for skin cancer. Combining the results of controlled clinical trials, more cases of NMSC were observed in patients receiving etanercept compared with control patients, particularly in patients with psoriasis. Vaccinations Live vaccines should not be given concurrently with Erelzi. No data are available on the secondary transmission of infection by live vaccines in patients receiving etanercept. In a double-blind, placebo-controlled, randomised clinical study in adult patients with psoriatic arthritis, 184 patients also received a multivalent pneumococcal polysaccharide vaccine at week 4. In this study, most psoriatic arthritis patients receiving etanercept were able to mount effective B-cell immune response to pneumococcal polysaccharide vaccine, but titres in aggregate were moderately lower, and few patients had two-fold rises in titres compared to patients not receiving etanercept. The clinical significance of this is unknown. Autoantibody formation Treatment with Erelzi may result in the formation of autoimmune antibodies (see section 4.8). Haematologic reactions Rare cases of pancytopenia and very rare cases of aplastic anaemia, some with fatal outcome, have been reported in patients treated with etanercept. Caution should be exercised in patients being treated with Erelzi who have a previous history of blood dyscrasias. All patients and parents/caregivers should be advised that if the patient develops signs and symptoms suggestive of blood dyscrasias or infections (e.g., persistent fever, sore throat, bruising, bleeding, paleness) whilst on Erelzi, they should seek immediate medical advice. Such patients should be investigated urgently, including full blood count; if blood dyscrasias are confirmed, Erelzi should be discontinued. Neurological disorders There have been rare reports of CNS demyelinating disorders in patients treated with etanercept (see section 4.8). Additionally, there have been rare reports of peripheral demyelinating polyneuropathies (including Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy, demyelinating polyneuropathy, and multifocal motor neuropathy). Although no clinical trials have been performed evaluating etanercept therapy in patients with multiple sclerosis, clinical trials of other TNF antagonists in patients with multiple sclerosis have shown increases in disease activity. A careful risk/benefit evaluation, including a neurologic assessment, is recommended when prescribing Erelzi to patients with pre-existing or recent onset of demyelinating disease, or to those who are considered to have an increased risk of developing demyelinating disease. Combination therapy In a controlled clinical trial of two years duration in rheumatoid arthritis patients, the combination of etanercept and methotrexate did not result in unexpected safety findings, and the safety profile of etanercept when given in combination with methotrexate was similar to the profiles reported in studies of etanercept and methotrexate alone. Long- term studies to assess the safety of the combination are ongoing. The long-term safety of etanercept in combination with other disease-modifying antirheumatic drugs (DMARD) has not been established. The use of etanercept in combination with other systemic therapies or phototherapy for the treatment of psoriasis has not been studied. Renal and hepatic impairment Based on pharmacokinetic data (see section 5.2), no dose adjustment is needed in patients with renal or hepatic impairment; clinical experience in such patients is limited. Congestive heart failure (Cardiac failure congestive) Physicians should use caution when using Erelzi in patients who have congestive heart failure (CHF). There have been postmarketing reports of worsening of CHF, with and without identifiable precipitating factors, in patients taking etanercept. There have also been rare (< 0.1%) reports of new onset CHF, including CHF in patients without known pre-existing cardiovascular disease. Some of these patients have been under 50 years of age. Two large clinical trials evaluating the use of etanercept in the treatment of CHF were terminated early due to lack of efficacy. Although not conclusive, data from one of these trials suggest a possible tendency toward worsening CHF in those patients assigned to etanercept treatment. Alcoholic hepatitis In a phase II randomised placebo-controlled study of 48 hospitalised patients treated with etanercept or placebo for moderate to severe alcoholic hepatitis, etanercept was not efficacious, and the mortality rate in patients treated with etanercept was significantly higher after 6 months. Consequently, Erelzi should not be used in patients for the treatment of alcoholic hepatitis. Physicians should use caution when using Erelzi in patients who also have moderate to severe alcoholic hepatitis. Wegener's granulomatosis A placebo-controlled trial, in which 89 adult patients were treated with etanercept in addition to standard therapy (including cyclophosphamide or methotrexate, and glucocorticoids) for a median duration of 25 months, has not shown etanercept to be an effective treatment for Wegener’s granulomatosis. The incidence of non-cutaneous malignancies of various types was significantly higher in patients treated with etanercept than in the control group. Etanercept is not recommended for the treatment of Wegener’s granulomatosis. Hypoglycaemia in patients treated for diabetes There have been reports of hypoglycaemia following initiation of etanercept in patients receiving medications for diabetes, necessitating a reduction in anti-diabetic medications in some of these patients. Special populations Elderly In the Phase 3 studies in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis, no overall differences in adverse events, serious adverse events, and serious infections in patients age 65 or older who received etanercept were observed compared with younger patients. However, caution should be exercised when treating the elderly and particular attention paid with respect to occurrence of infections. Paediatric population Vaccinations It is recommended that paediatric patients, if possible, be brought up to date with all immunisations in agreement with current immunisation guidelines prior to initiating Erelzi therapy (see Vaccinations, above). Erelzi contains sodium This medicinal product contains less than 1 mmol sodium (23 mg) per 25mg or 50 mg, that is to say essentially ‘sodium-free’.
Effects on Driving
4.7 Effects on ability to drive and use machines Erelzi has no or negligible influence on the ability to drive and use machines.

פרטי מסגרת הכללה בסל
1. התרופה תינתן לטיפול בחולה הסובל מאחד מאלה: א. ארתריטיס ראומטואידית - כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת, בכפוף לתנאי פסקה 3; ב. ארתריטיס כרוני בצעירים (Juvenile chronic arthritis) - בקטינים שמלאו להם 4 שנים וטרם מלאו להם 17 שנים הסובלים ממהלך מחלה רב מפרקי פעיל ושלא הגיבו לטיפול ב-methotrexate או שאינם מסוגלים לקבל טיפול כאמור; ג. דלקת מפרקים פסוריאטית קשה כאשר התגובה לתכשירים ממשפחת ה-DMARDs איננה מספקת ולאחר כשלון או אי סבילות ל-salazopyrin או methotrexate; ד. אנקילוזינג ספונדילטיס קשה אם החולה לא הגיב לטיפול קונבנציונלי; במקרה של הוריאנט דמוי אנקילוזינג ספונדיליטיס הקשור בפסוריאזיס, תהיה ההוריה כמו באנקילוזינג ספונדיליטיס ראשונית; ה. פסוריאזיס מלווה בוריאנט דמוי אנקילוזינג ספונדיליטיס, אם החולה לא הגיב לטיפול קונבנציונלי; ו. פסוריאזיס - בהתקיים כל אלה: 1. החולה סובל מאחד מאלה: א. מחלה מפושטת מעל ל-50% של שטח גוף או PASI מעל 50. ב. נגעים באזורי גוף רגישים - אזורים אלו יכללו פנים, צוואר, קיפולי עור, כפות ידיים, כפות רגליים, אזור הגניטליה והישבן;2. החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור של 50% לפחות ב-PASI לאחר סיום הטיפול בהשוואה לתחילת הטיפול; בהתייחס לחולה העונה על האמור בפסקת משנה (1)(ב) - החולה קיבל שני טיפולים סיסטמיים לפחות בלא שיפור משמעותי לאחר סיום הטיפול בהשוואה לתחילת הטיפול; 3. התרופה תינתן על פי מרשם של רופא מומחה בדרמטולוגיה. 3. הטיפול בתרופה לחולה העונה על תנאי פסקה (1) (א), יינתן בהתקיים כל אלה: 1. קיימת עדות לדלקת פרקים (RA-Rheumatoid Arthritis) פעילה המתבטאת בשלושה מתוך אלה: א. מחלה דלקתית (כולל כאב ונפיחות) בארבעה פרקים ויותר; ב. שקיעת דם או CRP החורגים מהנורמה באופן משמעותי (בהתאם לגיל החולה); ג. שינויים אופייניים ל-RA בצילומי רנטגן של הפרקים הנגועים; ד. פגיעה תפקודית המוגדרת כהגבלה משמעותית בתפקודו היומיומי של החולה ובפעילותו בעבודה. 2. לאחר מיצוי הטיפול בתרופות השייכות למשפחת ה-NSAIDs ובתרופות השייכות למשפחת ה-DMARDs. לעניין זה יוגדר מיצוי הטיפול כהעדר תגובה קלינית לאחר טיפול קו ראשון בתרופות אנטי דלקתיות ממשפחת ה-NSAIDs וטיפול קו שני ב-3 תרופות לפחות ממשפחת ה-DMARDs שאחת מהן מתוטרקסאט, במשך 3 חודשים רצופים לפחות. 3. הטיפול יינתן באישור רופא מומחה בראומטולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| juvenile idiopathic rheumatoid arthritis | ADALIMUMAB, ETANERCEPT | |||
| Psoriatic arthritis | ADALIMUMAB, USTEKINUMAB, SECUKINUMAB, ETANERCEPT, INFLIXIMAB | |||
| Psoriasis | EFALIZUMAB, ADALIMUMAB, IXEKIZUMAB, USTEKINUMAB, SECUKINUMAB, ALEFACEPT, ETANERCEPT, INFLIXIMAB | |||
| Rheumatoid arthritis | TOFACITINIB, CERTOLIZUMAB PEGOL, TOCILIZUMAB, SARILUMAB, ABATACEPT, ETANERCEPT, INFLIXIMAB | |||
| Ankylosing spondylitis | ADALIMUMAB, CERTOLIZUMAB PEGOL, USTEKINUMAB, SECUKINUMAB, ETANERCEPT, INFLIXIMAB |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
01.08.22 - עלון לצרכן 18.11.21 - עלון לצרכן אנגלית 18.11.21 - עלון לצרכן עברית 18.11.21 - עלון לצרכן ערבית 16.02.24 - עלון לצרכן עברית 11.07.24 - עלון לצרכן עברית 07.09.20 - החמרה לעלון 28.03.21 - החמרה לעלון 18.11.21 - החמרה לעלון 29.11.22 - החמרה לעלון 16.02.24 - החמרה לעלון 11.07.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ארלזי 25