Quest for the right Drug
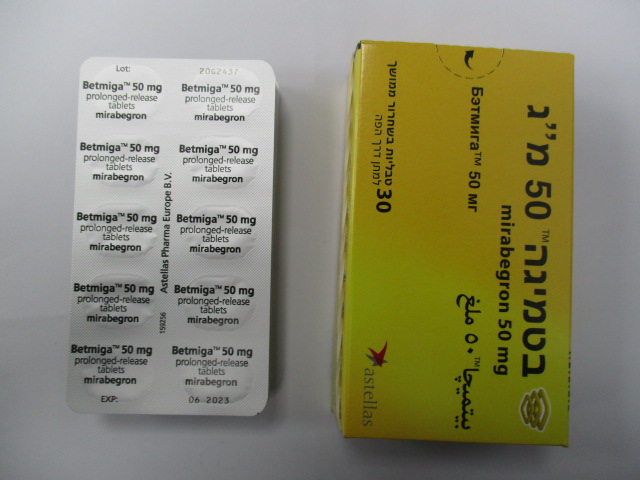
בטמיגה 50 מ"ג BETMIGA 50 MG (MIRABEGRON)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות בשחרור ממושך : TABLETS PROLONGED RELEASE
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Urologicals, urinary antispasmodics ATC code: G04BD12. Mechanism of action Mirabegron is a potent and selective beta 3-adrenoceptor agonist. Mirabegron showed relaxation of bladder smooth muscle in rat and human isolated tissue, increased cyclic adenosine monophosphate (cAMP) concentrations in rat bladder tissue and showed a bladder relaxant effect in rat urinary bladder function models. Mirabegron increased mean voided volume per micturition and decreased the frequency of non-voiding contractions, without affecting voiding pressure, or residual urine in rat models of bladder overactivity. In a monkey model, mirabegron showed decreased voiding frequency. These results indicate that mirabegron enhances urine storage function by stimulating beta 3-adrenoceptors in the bladder. During the urine storage phase, when urine accumulates in the bladder, sympathetic nerve stimulation predominates. Noradrenaline is released from nerve terminals, leading predominantly to beta adrenoceptor activation in the bladder musculature, and hence bladder smooth muscle relaxation. During the urine voiding phase, the bladder is predominantly under parasympathetic nervous system control. Acetylcholine, released from pelvic nerve terminals, stimulates cholinergic M2 and M3 receptors, inducing bladder contraction. The activation of the M2 pathway also inhibits beta 3-adrenoceptor induced increases in cAMP. Therefore beta 3-adrenoceptor stimulation should not interfere with the voiding process. This was confirmed in rats with partial urethral obstruction, where mirabegron decreased the frequency of non-voiding contractions without affecting the voided volume per micturition, voiding pressure, or residual urine volume. Pharmacodynamic effects Urodynamics Betmiga at doses of 50 mg and 100 mg once daily for 12 weeks in men with lower urinary tract symptoms (LUTS) and bladder outlet obstruction (BOO) showed no effect on cystometry parameters and was safe and well tolerated. The effects of mirabegron on maximum flow rate and detrusor pressure at maximum flow rate were assessed in this urodynamic study consisting of 200 male patients with LUTS and BOO. Administration of mirabegron at doses of 50 mg and 100 mg once daily for 12 weeks did not adversely affect the maximum flow rate or detrusor pressure at maximum flow rate. In this study in male patients with LUTS/BOO, the adjusted mean (SE) change from baseline to end of treatment in post void residual volume (mL) was 0.55 (10.702), 17.89 (10.190), 30.77 (10.598) for the placebo, mirabegron 50 mg and mirabegron 100 mg treatment groups. Effect on QT interval Betmiga at doses of 50 mg or 100 mg had no effect on the QT interval individually corrected for heart rate (QTcI interval) when evaluated either by sex or by the overall group. A thorough QT (TQT) study (n = 164 healthy male and n = 153 healthy female volunteers with a mean age of 33 years) evaluated the effect of repeat oral dosing of mirabegron at the indicated dose (50 mg once daily) and two supra-therapeutic doses (100 and 200 mg once daily) on the QTcI interval. The supra-therapeutic doses represent approximately 2.6- and 6.5-fold the exposure of the therapeutic dose, respectively. A single 400 mg dose of moxifloxacin was used as a positive control. Each dose level of mirabegron and moxifloxacin was evaluated in separate treatment arms each including placebo-control (parallel cross-over design). For both males and females administered mirabegron at 50 mg and 100 mg, the upper bound of the one-sided 95% confidence interval did not exceed 10 msec at any time point for the largest time-matched mean difference from placebo in the QTcI interval. In females administered mirabegron at the 50 mg dose, the mean difference from placebo on QTcI interval at 5 hours post dose was 3.67 msec (upper bound of the one-sided 95% CI 5.72 msec). In males, the difference was 2.89 msec (upper bound of the one-sided 95% CI 4.90 msec). At a mirabegron dose of 200 mg, the QTcI interval did not exceed 10 msec at any time point in males, while in females the upper bound of the one-sided 95% confidence interval did exceed 10 msec between 0.5–6 hours, with a maximum difference from placebo at 5 hours where the mean effect was 10.42 msec (upper bound of the one-sided 95% CI 13.44 msec). Results for QTcF and QTcIf were consistent with QTcI. In this TQT study, mirabegron increased heart rate on ECG in a dose dependent manner across the 50 mg to 200 mg dose range examined. The maximum mean difference from placebo in heart rate ranged from 6.7 bpm with mirabegron 50 mg up to 17.3 bpm with mirabegron 200 mg in healthy subjects. Effects on pulse rate and blood pressure in patients with OAB In OAB patients (mean age of 59 years) across three 12-week phase 3 double blind, placebo controlled studies receiving Betmiga 50 mg once daily, an increase in mean difference from placebo of approximately 1 bpm for pulse rate and approximately 1 mm Hg or less in systolic blood pressure/ diastolic blood pressure (SBP/DBP) was observed. Changes in pulse rate and blood pressure are reversible upon discontinuation of treatment. Effect on intraocular pressure (IOP) Mirabegron 100 mg once daily did not increase IOP in healthy subjects after 56 days of treatment. In a phase 1 study assessing the effect of Betmiga on IOP using Goldmann applanation tonometry in 310 healthy subjects, a dose of mirabegron 100 mg was non-inferior to placebo for the primary endpoint of the treatment difference in mean change from baseline to day 56 in subject-average IOP; the upper bound of the two-sided 95% CI of the treatment difference between mirabegron 100 mg and placebo was 0.3 mm Hg. Clinical efficacy and safety Efficacy of Betmiga was evaluated in three phase 3 randomized, double blind, placebo controlled, 12- week studies for the treatment of overactive bladder with symptoms of urgency and frequency with or without incontinence. Female (72%) and male (28%) patients with a mean age of 59 years (range 18 – 95 years) were included. The study population consisted of approximately 48% antimuscarinic treatment naïve patients as well as approximately 52% patients previously treated with antimuscarinic medicinal products. In one study, 495 patients received an active control (tolterodine prolonged release formulation). The co-primary efficacy endpoints were (1) change from baseline to end of treatment in mean number of incontinence episodes per 24 hours and (2) change from baseline to end of treatment in mean number of micturitions per 24 hours based on a 3-day micturition diary. Mirabegron demonstrated statistically significant larger improvements compared to placebo for both co-primary endpoints as well as secondary endpoints (see Tables 1 and 2). Table 2: Co-primary and selected secondary efficacy endpoints at end of treatment for pooled studies Pooled studies (046, 047, 074) Placebo Mirabegron Parameter 50 mg Mean number of incontinence episodes per 24 hours (FAS-I) (Co-primary) N 878 862 Mean baseline 2.73 2.71 Mean change from baseline† -1.10 -1.49 Mean difference from placebo† (95% CI) -- -0.40 (-0.58, -0.21) p-value -- < 0.001# Mean number of micturitions per 24 hours (FAS) (Co-primary) n 1328 1324 Mean baseline 11.58 11.70 Mean change from baseline† -1.20 -1.75 Mean difference from placebo† (95% CI) -- -0.55 (-0.75, -0.36) p-value -- < 0.001# Mean volume voided (mL) per micturition (FAS) (Secondary) n 1328 1322 Mean baseline 159.2 159.0 Mean change from baseline† 9.4 21.4 Mean difference from placebo† (95% CI) -- 11.9 (8.3, 15.5) p-value -- < 0.001# Mean level of urgency (FAS) (Secondary) n 1325 1323 Mean baseline 2.39 2.42 Mean change from baseline† -0.15 -0.26 Mean difference from placebo† (95% CI) -- -0.11 (-0.16, -0.07) p-value -- < 0.001# Mean number of urgency incontinence episodes per 24 hours (FAS-I) (Secondary) n 858 834 Mean baseline 2.42 2.42 Mean change from baseline† -0.98 -1.38 Mean difference from placebo† (95% CI) -- -0.40 (-0.57, -0.23) p-value -- < 0.001# Mean number of episodes with urgency grades 3 or 4 per 24 hours (FAS) (Secondary) n 1324 1320 Mean baseline 5.61 5.80 Mean change from baseline† -1.29 -1.93 Mean difference from placebo† (95% CI) -- -0.64 (-0.89, -0.39) p-value -- < 0.001# Treatment satisfaction – visual analogue scale (FAS) (Secondary) n 1195 1189 Mean baseline 4.87 4.82 Mean change from baseline† 1.25 2.01 Mean difference from placebo† (95% CI) -- 0.76 (0.52, 1.01) p-value -- < 0.001* Pooled studies consisted of studies 046 (Europe/Australia), 047 (North America [NA]) and 074 (Europe/NA). † Least squares mean adjusted for baseline, gender, and study. * Statistically significantly superior compared to placebo at the 0.05 level without multiplicity adjustment. # Statistically significantly superior compared to placebo at the 0.05 level with multiplicity adjustment. FAS: Full analysis set, all randomized patients who took at least 1 dose of double blind study drug and who had a micturition measurement in the baseline diary and at least 1 post-baseline visit diary with a micturition measurement. FAS-I: Subset of FAS who also had at least 1 incontinence episode in the baseline diary. CI: Confidence Interval Table 3: Co-primary and selected secondary efficacy endpoints at end of treatment for studies 046, 047 and 074 Study 046 Study 047 Study 074 Parameter Placebo Mirabegron Tolterodine Placebo Mirabegron Placebo Mirabegron 50 mg ER 4 mg 50 mg 50 mg Mean number of incontinence episodes per 24 hours (FAS-I) (Co-primary) n 291 293 300 325 312 262 257 Mean 2.67 2.83 2.63 3.03 2.77 2.43 2.51 baseline Mean change from -1.17 -1.57 -1.27 -1.13 -1.47 -0.96 -1.38 baseline† Mean difference -- -0.41 -0.10 -- -0.34 -- -0.42 from placebo† 95% (- (-0.42, (- (- Confidence -- -- -- 0.72, -0.09) 0.21) 0.66, -0.03) 0.76, -0.08) Interval p-value -- 0.003# 0.11 -- 0.026# -- 0.001# Mean number of micturitions per 24 hours (FAS) (Co-primary) n 480 473 475 433 425 415 426 Mean 11.71 11.65 11.55 11.51 11.80 11.48 11.66 baseline Mean change from -1.34 -1.93 -1.59 -1.05 -1.66 -1.18 -1.60 baseline† Mean difference -- -0.60 -0.25 -- -0.61 -- -0.42 from placebo† 95% (- (-0.55, (- (- Confidence -- -- -- 0.90, -0.29) 0.06) 0.98, -0.24) 0.76, -0.08) Interval p-value -- <0.001# 0.11 -- 0.001# -- 0.015# Mean volume voided (mL) per micturition (FAS) (Secondary) n 480 472 475 433 424 415 426 Mean 156.7 161.1 158.6 157.5 156.3 164.0 159.3 baseline Mean change from 12.3 24.2 25.0 7.0 18.2 8.3 20.7 baseline† Mean difference -- 11.9 12.6 -- 11.1 -- 12.4 from placebo† 95% Confidence -- (6.3, 17.4) (7.1, 18.2) -- (4.4, 17.9) -- (6.3, 18.6) Interval p-value -- <0.001# <0.001* -- 0.001# -- <0.001# Mean level of urgency (FAS) (Secondary) n 480 472 473 432 425 413 426 Mean 2.37 2.40 2.41 2.45 2.45 2.36 2.41 baseline Study 046 Study 047 Study 074 Parameter Placebo Mirabegron Tolterodine Placebo Mirabegron Placebo Mirabegron 50 mg ER 4 mg 50 mg 50 mg Mean change from -0.22 -0.31 -0.29 -0.08 -0.19 -0.15 -0.29 baseline† Mean difference -- -0.09 -0.07 -- -0.11 -- -0.14 from placebo† 95% (-0.17, (-0.15, (- (- Confidence -- -- -- -0.02) 0.01) 0.18, -0.04) 0.22, -0.06) Interval p-value -- 0.018* 0.085 -- 0.004* -- <0.001‡ Mean number of urgency incontinence episodes per 24 hours (FAS-I) (Secondary) n 283 286 289 319 297 256 251 Mean 2.43 2.52 2.37 2.56 2.42 2.24 2.33 baseline Mean change from -1.11 -1.46 -1.18 -0.89 -1.32 -0.95 -1.33 baseline† Mean difference -- -0.35 -0.07 -- -0.43 -- -0.39 from placebo† 95% (- (-0.38, (-0.72, (- Confidence -- -- -- 0.65, -0.05) 0.23) -0.15) 0.69, -0.08) Interval p-value -- 0.003* 0.26 -- 0.005* -- 0.002‡ Mean number of episodes with urgency grades 3 or 4 per 24 hours (FAS) (Secondary) n 479 470 472 432 424 413 426 Mean 5.78 5.72 5.79 5.61 5.90 5.42 5.80 baseline Mean change from -1.65 -2.25 -2.07 -0.82 -1.57 -1.35 -1.94 baseline† Mean difference -- -0.60 -0.42 -- -0.75 -- -0.59 from placebo† 95% (- (- (- (- Confidence -- -- -- 1.02, -0.18) 0.84, -0.00) 1.20, -0.30) 1.01, -0.16) Interval p-value -- 0.005* 0.050* -- 0.001* -- 0.007‡ Treatment satisfaction – visual analogue scale (FAS) (Secondary) n 428 414 425 390 387 377 388 Mean 4.11 3.95 3.87 5.5 5.4 5.13 5.13 baseline Mean change from 1.89 2.55 2.44 0.7 1.5 1.05 1.88 baseline† Mean difference -- 0.66 0.55 -- 0.8 -- 0.83 from placebo† 95% -- (0.25, 1.07) (0.14, 0.95) -- (0.4, 1.3) -- (0.41, 1.25) Study 046 Study 047 Study 074 Parameter Placebo Mirabegron Tolterodine Placebo Mirabegron Placebo Mirabegron 50 mg ER 4 mg 50 mg 50 mg Confidence Interval p-value -- 0.001* 0.008* -- <0.001* -- <0.001* † Least squares mean adjusted for baseline, gender and geographical region. * Statistically significantly superior compared with placebo at the 0.05 level without multiplicity adjustment. # Statistically significantly superior compared with placebo at the 0.05 level with multiplicity adjustment. ‡ Not statistically significantly superior compared to placebo at the 0.05 level with multiplicity adjustment. FAS: Full analysis set, all randomized patients who took at least 1 dose of double blind study drug and who had a micturition measurement in the baseline diary and at least 1 post-baseline visit diary with a micturition measurement. FAS-I: Subset of FAS who also had at least 1 incontinence episode in the baseline diary. Betmiga 50 mg once daily was effective at the first measured time point of week 4, and efficacy was maintained throughout the 12-week treatment period. A randomized, active controlled, long term study demonstrated that efficacy was maintained throughout a 1-year treatment period. Subjective improvement in health-related quality of life measurements In the three 12-week phase 3 double blind, placebo controlled studies, treatment of the symptoms of OAB with mirabegron once daily resulted in a statistically significant improvement over placebo on the following health-related quality of life measures: treatment satisfaction and symptom bother. Efficacy in patients with or without prior OAB antimuscarinic therapy Efficacy was demonstrated in patients with and without prior OAB antimuscarinic therapy. In addition mirabegron showed efficacy in patients who previously discontinued OAB antimuscarinic therapy due to insufficient effect (see Table 3). Table 4: Co-primary efficacy endpoints for patients with prior OAB antimuscarinic therapy Pooled studies (046, 047, 074) Study 046 Placebo Mirabegron Placebo Mirabegron Tolterodine Parameter 50 mg 50 mg ER 4 mg Patients with prior OAB antimuscarinic therapy Mean number of incontinence episodes per 24 hours (FAS-I) N 518 506 167 164 160 Mean baseline 2.93 2.98 2.97 3.31 2.86 Mean change from baseline† -0.92 -1.49 -1.00 -1.48 -1.10 Mean difference from placebo† -- -0.57 -- -0.48 -0.10 95% Confidence Interval -- (-0.81, -0.33) -- (-0.90, -0.06) (-0.52, 0.32) Mean number of micturitions per 24 hours (FAS) N 704 688 238 240 231 Mean baseline 11.53 11.78 11.90 11.85 11.76 Mean change from baseline† -0.93 -1.67 -1.06 -1.74 -1.26 Mean difference from placebo† -- -0.74 -- -0.68 -0.20 95% Confidence Interval -- (-1.01, -0.47) -- (-1.12, -0.25) (-0.64, 0.23) Patients with prior OAB antimuscarinic therapy who discontinued due to insufficient effect Mean number of incontinence episodes per 24 hours (FAS-I) N 336 335 112 105 102 Mean baseline 3.03 2.94 3.15 3.50 2.63 Mean change from baseline† -0.86 -1.56 -0.87 -1.63 -0.93 Mean difference from placebo† -- -0.70 -- -0.76 -0.06 95% Confidence Interval -- (-1.01, -0.38) -- (-1.32, -0.19) (-0.63, 0.50) Mean number of micturitions per 24 hours (FAS) N 466 464 159 160 155 Mean baseline 11.60 11.67 11.89 11.49 11.99 Mean change from baseline† -0.86 -1.54 -1.03 -1.62 -1.11 Mean difference from placebo† -- -0.67 -- -0.59 -0.08 95% Confidence Interval -- (-0.99, -0.36) -- (-1.15, -0.04) (-0.64, 0.47) Pooled studies consisted of 046 (Europe/Australia), 047 (North America [NA]) and 074 (Europe/NA). † Least squares mean adjusted for baseline, gender, study, subgroup, and subgroup by treatment interaction for Pooled Studies and least squares mean adjusted for baseline, gender, geographical region, subgroup, and subgroup by treatment interaction for Study 046. FAS: Full analysis set, all randomized patients who took at least 1 dose of double blind study drug and who had a micturition measurement in the baseline diary and at least 1 post-baseline visit diary with a micturition measurement. FAS-I: Subset of FAS who also had at least 1 incontinence episode in the baseline diary. Paediatric population The European Medicines Agency has deferred the obligation to submit the results of studies with Betmiga in one or more subsets of the paediatric population in “Treatment of idiopathic overactive bladder” and “Treatment of neurogenic detrusor overactivity” (see section 4.2 for information on paediatric use).
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Absorption After oral administration of mirabegron in healthy volunteers mirabegron is absorbed to reach peak plasma concentrations (Cmax) between 3 and 4 hours. The absolute bioavailability increased from 29% at a dose of 25 mg to 35% at a dose of 50 mg. Mean Cmax and AUC increased more than dose proportionally over the dose range. In the overall population of males and females, a 2-fold increase in dose from 50 mg to 100 mg mirabegron increased Cmax and AUCtau by approximately 2.9- and 2.6-fold, respectively, whereas a 4-fold increase in dose from 50 mg to 200 mg mirabegron increased Cmax and AUCtau by approximately 8.4- and 6.5-fold. Steady state concentrations are achieved within 7 days of once daily dosing with mirabegron. After once daily administration, plasma exposure of mirabegron at steady state is approximately double that seen after a single dose. Effect of food on absorption Co-administration of a 50 mg tablet with a high-fat meal reduced mirabegron Cmax and AUC by 45% and 17%, respectively. A low-fat meal decreased mirabegron Cmax and AUC by 75% and 51%, respectively. In the phase 3 studies, mirabegron was administered with or without food and demonstrated both safety and efficacy. Therefore, mirabegron can be taken with or without food at the recommended dose. Distribution Mirabegron is extensively distributed. The volume of distribution at steady state (Vss) is approximately 1670 L. Mirabegron is bound (approximately 71%) to human plasma proteins, and shows moderate affinity for albumin and alpha-1 acid glycoprotein. Mirabegron distributes to erythrocytes. In vitro erythrocyte concentrations of 14C-mirabegron were about 2-fold higher than in plasma. Biotransformation Mirabegron is metabolised via multiple pathways involving dealkylation, oxidation, (direct) glucuronidation, and amide hydrolysis. Mirabegron is the major circulating component following a single dose of 14C-mirabegron. Two major metabolites were observed in human plasma; both are phase 2 glucuronides representing 16% and 11% of total exposure. These metabolites are not pharmacologically active. Based on in vitro studies, mirabegron is unlikely to inhibit the metabolism of co-administered medicinal products metabolised by the following cytochrome P450 enzymes: CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 and CYP2E1 because mirabegron did not inhibit the activity of these enzymes at clinically relevant concentrations. Mirabegron did not induce CYP1A2 or CYP3A. Mirabegron is predicted not to cause clinically relevant inhibition of OCT-mediated drug transport. Although in vitro studies suggest a role for CYP2D6 and CYP3A4 in the oxidative metabolism of mirabegron, in vivo results indicate that these isozymes play a limited role in the overall elimination. In vitro and ex vivo studies have shown the involvement from butyrylcholinesterase, UGT and possibly alcohol dehydrogenase (ADH) in the metabolism of mirabegron, in addition to CYP3A4 and CYP2D6. CYP2D6 polymorphism In healthy subjects who are genotypically poor metabolisers of CYP2D6 substrates (used as a surrogate for CYP2D6 inhibition), mean Cmax and AUCinf of a single 160 mg dose of a mirabegron IR formulation were 14% and 19% higher than in extensive metabolisers, indicating that CYP2D6 genetic polymorphism has minimal impact on the mean plasma exposure to mirabegron. Interaction of mirabegron with a known CYP2D6 inhibitor is not expected and was not studied. No dose adjustment is needed for mirabegron when administered with CYP2D6 inhibitors or in patients who are CYP2D6 poor metabolisers. Elimination Total body clearance (CLtot) from plasma is approximately 57 L/h. The terminal elimination half-life (t1/2) is approximately 50 hours. Renal clearance (CLR) is approximately 13 L/h, which corresponds to nearly 25% of CLtot. Renal elimination of mirabegron is primarily through active tubular secretion along with glomerular filtration. The urinary excretion of unchanged mirabegron is dose-dependent and ranges from approximately 6.0% after a daily dose of 25 mg to 12.2% after a daily dose of 100 mg. Following the administration of 160 mg 14C-mirabegron to healthy volunteers, approximately 55% of the radiolabel was recovered in the urine and 34% in the faeces. Unchanged mirabegron accounted for 45% of the urinary radioactivity, indicating the presence of metabolites. Unchanged mirabegron accounted for the majority of the faecal radioactivity. Age The Cmax and AUC of mirabegron and its metabolites following multiple oral doses in elderly volunteers (≥ 65 years) were similar to those in younger volunteers (18–45 years). Gender The Cmax and AUC are approximately 40% to 50% higher in females than in males. Gender differences in Cmax and AUC are attributed to differences in body weight and bioavailability. Race The pharmacokinetics of mirabegron are not influenced by race. Renal impairment Following single dose administration of 100 mg Betmiga in volunteers with mild renal impairment (eGFR-MDRD 60 to 89 mL/min/1.73 m2), mean mirabegron Cmax and AUC were increased by 6% and 31% relative to volunteers with normal renal function. In volunteers with moderate renal impairment (eGFR-MDRD 30 to 59 mL/min/1.73 m2), Cmax and AUC were increased by 23% and 66%, respectively. In volunteers with severe renal impairment (eGFR-MDRD 15 to 29 mL/min/1.73 m2), mean Cmax and AUC values were 92% and 118% higher. Mirabegron has not been studied in patients with end stage renal disease (GFR < 15 mL/min/1.73 m2 or patients requiring haemodialysis). Hepatic impairment Following single dose administration of 100 mg Betmiga in volunteers with mild hepatic impairment (Child-Pugh Class A), mean mirabegron Cmax and AUC were increased by 9% and 19% relative to volunteers with normal hepatic function. In volunteers with moderate hepatic impairment (Child-Pugh Class B), mean Cmax and AUC values were 175% and 65% higher. Mirabegron has not been studied in patients with severe hepatic impairment (Child-Pugh Class C).

פרטי מסגרת הכללה בסל
התרופה תינתן לטיפול בתסמונת שלפוחית שתן פעילה ביתר (overactive bladder syndrome)
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| התרופה תינתן לטיפול בתסמונת שלפוחית שתן פעילה ביתר (overactive bladder syndrome) | 01/03/2021 | אורולוגיה | Overactive bladder |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2021
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
רישום
153 47 34113 01
מחיר
0 ₪
מידע נוסף
עלון מידע לצרכן
23.07.19 - עלון לצרכן אנגלית 23.07.19 - עלון לצרכן עברית 04.02.18 - עלון לצרכן ערבית 23.07.19 - עלון לצרכן ערבית 30.08.24 - עלון לצרכן אנגלית 30.08.24 - עלון לצרכן עברית 30.08.24 - עלון לצרכן ערבית 26.09.24 - עלון לצרכן אנגלית 26.09.24 - עלון לצרכן ערבית 04.11.24 - עלון לצרכן עברית 23.07.19 - החמרה לעלוןלתרופה במאגר משרד הבריאות
בטמיגה 50 מ"ג