Quest for the right Drug
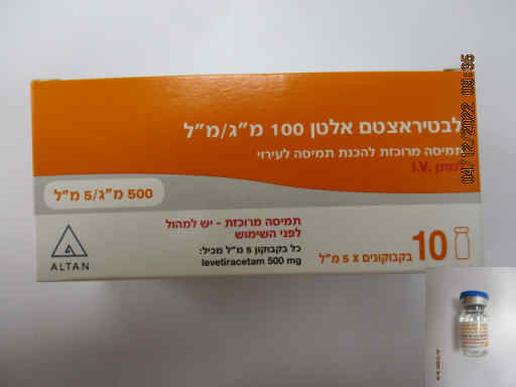
לבטיראצטם אלטן 100 מ"ג/מ"ל LEVETIRACETAM ALTAN 100 MG/ML (LEVETIRACETAM)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: antiepileptics, other antiepileptics, ATC code: N03AX14. The active substance, levetiracetam, is a pyrrolidone derivative (S-enantiomer of α-ethyl-2- oxo-1-pyrrolidine acetamide), chemically unrelated to existing antiepileptic active substances. Mechanism of action The mechanism of action of levetiracetam still remains to be fully elucidated. In vitro and in vivo experiments suggest that levetiracetam does not alter basic cell characteristics and normal neurotransmission. In vitro studies show that levetiracetam affects intraneuronal Ca2+ levels by partial inhibition of N-type Ca2+ currents and by reducing the release of Ca2+ from intraneuronal stores. In addition, it partially reverses the reductions in GABA- and glycine-gated currents induced by zinc and β-carbolines. Furthermore, levetiracetam has been shown in in vitro studies to bind to a specific site in rodent brain tissue. This binding site is the synaptic vesicle protein 2A, believed to be involved in vesicle fusion and neurotransmitter exocytosis. Levetiracetam and related analogues show a rank order of affinity for binding to the synaptic vesicle protein 2A which correlates with the potency of their anti-seizure protection in the mouse audiogenic model of epilepsy. This finding suggests that the interaction between levetiracetam and the synaptic vesicle protein 2A seems to contribute to the antiepileptic mechanism of action of the medicinal product. Pharmacodynamic effects Levetiracetam induces seizure protection in a broad range of animal models of partial and primary generalised seizures without having a pro-convulsant effect. The primary metabolite is inactive. In man, an activity in both partial and generalised epilepsy conditions (epileptiform discharge/photoparoxysmal response) has confirmed the broad spectrum pharmacological profile of levetiracetam. Clinical efficacy and safety Adjunctive therapy in the treatment of partial onset seizures with or without secondary generalisation in adults, adolescents and children from 4 years of age with epilepsy. In adults, levetiracetam efficacy has been demonstrated in 3 double-blind, placebo-controlled studies at 1000 mg, 2000 mg, or 3000 mg/day, given in 2 divided doses, with a treatment duration of up to 18 weeks. In a pooled analysis, the percentage of patients who achieved 50% or greater reduction from baseline in the partial onset seizure frequency per week at stable dose (12/14 weeks) was of 27.7%, 31.6% and 41.3% for patients on 1000, 2000 or 3000 mg levetiracetam respectively and of 12.6% for patients on placebo. Paediatric population In paediatric patients (4 to 16 years of age), levetiracetam efficacy was established in a double-blind, placebo-controlled study, which included 198 patients and had a treatment duration of 14 weeks. In this study, the patients received levetiracetam as a fixed dose of 60 mg/kg/day (with twice a day dosing). 44.6% of the levetiracetam treated patients and 19.6% of the patients on placebo had a 50% or greater reduction from baseline in the partial onset seizure frequency per week. With continued long-term treatment, 11.4% of the patients were seizure-free for at least 6 months and 7.2% were seizure-free for at least 1 year. 35 infants aged less than 1 year with partial onset seizures have been exposed in placebo- control clinical studies of which only 13 were aged < 6 months. Monotherapy in the treatment of partial onset seizures with or without secondary generalisation in patients from 16 years of age with newly diagnosed epilepsy. Efficacy of levetiracetam as monotherapy was established in a double-blind, parallel group, non-inferiority comparison to carbamazepine controlled release (CR) in 576 patients 16 years of age or older with newly or recently diagnosed epilepsy. The patients had to present with unprovoked partial seizures or with generalised tonic-clonic seizures only. The patients were randomized to carbamazepine CR 400 – 1200 mg/day or levetiracetam 1000 – 3000 mg/day, the duration of the treatment was up to 121 weeks depending on the response. Six-month seizure freedom was achieved in 73.0% of levetiracetam-treated patients and 72.8% of carbamazepine-CR treated patients; the adjusted absolute difference between treatments was 0.2% (95% CI: -7.8 8.2). More than half of the subjects remained seizure free for 12 months (56.6% and 58.5% of subjects on levetiracetam and on carbamazepine CR respectively). In a study reflecting clinical practice, the concomitant antiepileptic medication could be withdrawn in a limited number of patients who responded to levetiracetam adjunctive therapy (36 adult patients out of 69). Adjunctive therapy in the treatment of myoclonic seizures in adults and adolescents from 12 years of age with Juvenile Myoclonic Epilepsy. Levetiracetam efficacy was established in a double-blind, placebo-controlled study of 16 weeks duration, in patients 12 years of age and older suffering from idiopathic generalised epilepsy with myoclonic seizures in different syndromes. The majority of patients presented with juvenile myoclonic epilepsy. In this study, levetiracetam, dose was 3000 mg/day given in 2 divided doses. 58.3% of the levetiracetam treated patients and 23.3% of the patients on placebo had at least a 50% reduction in myoclonic seizure days per week. With continued long-term treatment, 28.6% of the patients were free of myoclonic seizures for at least 6 months and 21.0% were free of myoclonic seizures for at least 1 year. Adjunctive therapy in the treatment of primary generalised tonic-clonic seizures in adults and adolescents from 12 years of age with idiopathic generalised epilepsy. Levetiracetam efficacy was established in a 24-week double-blind, placebo-controlled study which included adults, adolescents and a limited number of children suffering from idiopathic generalised epilepsy with primary generalised tonic-clonic (PGTC) seizures in different syndromes (juvenile myoclonic epilepsy, juvenile absence epilepsy, childhood absence epilepsy, or epilepsy with Grand Mal seizures on awakening). In this study, levetiracetam dose was 3000 mg/day for adults and adolescents or 60 mg/kg/day for children, given in 2 divided doses. 72.2% of the levetiracetam treated patients and 45.2% of the patients on placebo had a 50% or greater decrease in the frequency of PGTC seizures per week. With continued long-term treatment, 47.4% of the patients were free of tonic-clonic seizures for at least 6 months and 31.5% were free of tonic-clonic seizures for at least 1 year.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties The pharmacokinetic profile has been characterized following oral administration. A single dose of 1500 mg levetiracetam diluted in 100 ml of a compatible diluent and infused intravenously over 15 minutes is bioequivalent to 1500 mg levetiracetam oral intake, given as three 500 mg tablets. The intravenous administration of doses up to 4000 mg diluted in 100 ml of 0.9% sodium chloride infused over 15 minutes and doses up to 2500 mg diluted in 100 ml of 0.9% sodium chloride infused over 5 minutes was evaluated. The pharmacokinetic and safety profiles did not identify any safety concerns. Levetiracetam is a highly soluble and permeable compound. The pharmacokinetic profile is linear with low intra- and inter-subject variability. There is no modification of the clearance after repeated administration. The time independent pharmacokinetic profile of levetiracetam was also confirmed following 1500 mg intravenous infusion for 4 days with twice daily dosing. There is no evidence for any relevant gender, race or circadian variability. The pharmacokinetic profile is comparable in healthy volunteers and in patients with epilepsy. Adults and adolescents Distribution Peak plasma concentration (Cmax) observed in 17 subjects following a single intravenous dose of 1500 mg infused over 15 minutes was 51 ± 19 µg/ml (arithmetic average ± standard deviation). No tissue distribution data are available in humans. Neither levetiracetam nor its primary metabolite are significantly bound to plasma proteins (< 10%). The volume of distribution of levetiracetam is approximately 0.5 to 0.7 l/kg, a value close to the total body water volume. Biotransformation Levetiracetam is not extensively metabolised in humans. The major metabolic pathway (24% of the dose) is an enzymatic hydrolysis of the acetamide group. Production of the primary metabolite, ucb L057, is not supported by liver cytochrome P450 isoforms. Hydrolysis of the acetamide group was measurable in a large number of tissues including blood cells. The metabolite ucb L057 is pharmacologically inactive. Two minor metabolites were also identified. One was obtained by hydroxylation of the pyrrolidone ring (1.6% of the dose) and the other one by opening of the pyrrolidone ring (0.9% of the dose). Other unidentified components accounted only for 0.6% of the dose. No enantiomeric interconversion was evidenced in vivo for either levetiracetam or its primary metabolite. In vitro, levetiracetam and its primary metabolite have been shown not to inhibit the major human liver cytochrome P450 isoforms (CYP3A4, 2A6, 2C9, 2C19, 2D6, 2E1 and 1A2), glucuronyl transferase (UGT1A1 and UGT1A6) and epoxide hydroxylase activities. In addition, levetiracetam does not affect the in vitro glucuronidation of valproic acid. In human hepatocytes in culture, levetiracetam had little or no effect on CYP1A2, SULT1E1 or UGT1A1. Levetiracetam caused mild induction of CYP2B6 and CYP3A4. The in vitro data and in vivo interaction data on oral contraceptives, digoxin and warfarin indicate that no significant enzyme induction is expected in vivo. Therefore, the interaction of Levetiracetam Altan 100 mg/ml with other substances, or vice versa, is unlikely. Elimination The plasma half-life in adults was 7±1 hours and did not vary either with dose, route of administration or repeated administration. The mean total body clearance was 0.96 ml/min/kg. The major route of excretion was via urine, accounting for a mean 95% of the dose (approximately 93% of the dose was excreted within 48 hours). Excretion via faeces accounted for only 0.3% of the dose. The cumulative urinary excretion of levetiracetam and its primary metabolite accounted for 66% and 24% of the dose, respectively during the first 48 hours. The renal clearance of levetiracetam and ucb L057 is 0.6 and 4.2 ml/min/kg respectively indicating that levetiracetam is excreted by glomerular filtration with subsequent tubular reabsorption and that the primary metabolite is also excreted by active tubular secretion in addition to glomerular filtration. Levetiracetam elimination is correlated to creatinine clearance. Elderly In the elderly, the half-life is increased by about 40% (10 to 11 hours). This is related to the decrease in renal function in this population (see section 4.2). Renal impairment The apparent body clearance of both levetiracetam and of its primary metabolite is correlated to the creatinine clearance. It is therefore recommended to adjust the maintenance daily dose of Levetiracetam Altan 100 mg/ml, based on creatinine clearance in patients with moderate and severe renal impairment (see section 4.2). In anuric end-stage renal disease adult subjects the half-life was approximately 25 and 3.1 hours during interdialytic and intradialytic periods, respectively. The fractional removal of levetiracetam was 51% during a typical 4-hour dialysis session. Hepatic impairment In subjects with mild and moderate hepatic impairment, there was no relevant modification of the clearance of levetiracetam. In most subjects with severe hepatic impairment, the clearance of levetiracetam was reduced by more than 50% due to a concomitant renal impairment (see section 4.2). Paediatric population Children (4 to 12 years) The pharmacokinetics in paediatric patients has not been investigated after intravenous administration. However, based on the pharmacokinetic characteristics of levetiracetam, the pharmacokinetics in adults after intravenous administration and the pharmacokinetics in children after oral administration, the exposure (AUC) of levetiracetam is expected to be similar in paediatric patients aged 4 to 12 years after intravenous and oral administration. Following single oral dose administration (20 mg/kg) to epileptic children (6 to 12 years), the half-life of levetiracetam was 6.0 hours. The apparent body weight adjusted clearance was approximately 30% higher than in epileptic adults. Following repeated oral dose administration (20 to 60 mg/kg/day) to epileptic children (4 to 12 years), levetiracetam was rapidly absorbed. Peak plasma concentration was observed 0.5 to 1.0 hour after dosing. Linear and dose proportional increases were observed for peak plasma concentrations and area under the curve. The elimination half-life was approximately 5 hours. The apparent body clearance was 1.1 ml/min/kg.

פרטי מסגרת הכללה בסל
א. התרופה האמורה תינתן לטיפול באפילפסיה. ב. מתן התרופה ייעשה לפי המלצת רופא מומחה בנוירולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| א. התרופה האמורה תינתן לטיפול באפילפסיה. ב. מתן התרופה ייעשה לפי המלצת רופא מומחה בנוירולוגיה. | 01/03/2021 | נוירולוגיה | אפילפסיה | |
| א. התרופה האמורה תינתן לטיפול באפילפסיה , ורק אם החולה אינו מאוזן על ידי טיפול בתרופה אנטי אפילפטית אחת אחרת כגון Carbamazepine, Valproic acid, Phenytoin, Primidone . ב. מתן התרופה ייעשה לפי המלצת רופא מומחה בנוירולוגיה. | 23/01/2011 | נוירולוגיה | אפילפסיה | |
| א. לטיפול באפילפסיה, ורק אם החולה אינו מאוזן (לפחות ארבעה התקפים בחודש) בשלושה קווי טיפול קודמים. ב. מתן התרופה ייעשה לפי המלצת רופא מומחה בנוירולוגיה | 15/05/2006 | נוירולוגיה | אפילפסיה |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
15/05/2006
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
