Quest for the right Drug
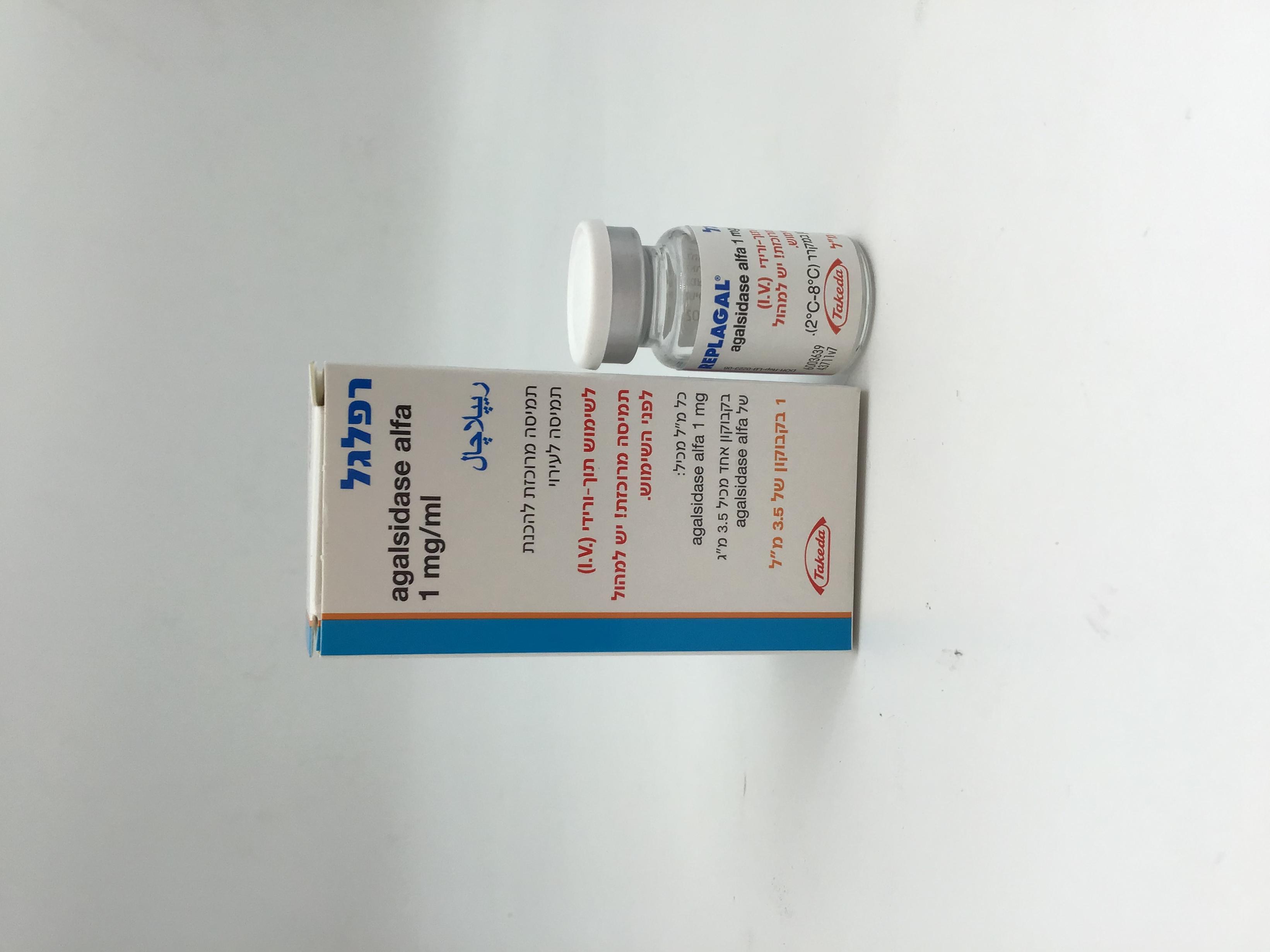
רפלגל REPLAGAL (AGALSIDASE ALFA)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תרכיז להכנת תמיסה לאינפוזיה : CONCENTRATE FOR SOLUTION FOR INFUSION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other alimentary tract and metabolism products - Enzymes. ATC code: A16AB03. Mechanism of action Fabry Disease is a glycosphingolipid storage disorder that is caused by deficient activity of the lysosomal enzyme α-galactosidase A, resulting in accumulation of globotriaosylceramide (Gb3 or GL- 3, also known as ceramidetrihexoside (CTH)), the glycosphingolipid substrate for this enzyme. Agalsidase alfa catalyses the hydrolysis of Gb3, cleaving a terminal galactose residue from the molecule. Treatment with the enzyme has been shown to reduce accumulation of Gb3 in many cell types including endothelial and parenchymal cells. Agalsidase alfa has been produced in a human cell line to provide for a human glycosylation profile that can influence uptake by mannose-6-phosphate receptors on the surface of target cells. The selection of 0.2 mg/kg dose (infused over 40 minutes) for the registration clinical studies was intended to temporarily saturate the ability of the mannose-6-phosphate receptors to internalize the agalsidase alfa in the liver and allow distribution of enzyme to other relevant organ tissues. Data with patients indicates that at least 0.1mg/kg is required to achieve a pharmacodynamics response. Clinical efficacy and safety The safety and efficacy of Replagal was assessed in two randomised, double blind, placebo controlled studies and open label extension studies, in a total of forty patients with a diagnosis of Fabry Disease based on clinical and biochemical evidence. Patients received the recommended dosage of 0.2 mg/kg of Replagal. Twenty-five patients completed the first study and entered an extension study. After 6 months of therapy there was a significant reduction in pain in the Replagal treated patients compared with placebo (p=0.021), as measured by the Brief Pain Inventory (a validated pain measurement scale). This was associated with a significant reduction in chronic neuropathic pain medication use and number of days on pain medication. In subsequent studies, in male paediatric patients above the age of 7, a reduction in pain was observed after 9 and 12 months of Replagal therapy compared to pre-treatment baseline. This pain reduction persisted through 4 years of Replagal therapy in 9 patients (in patients 7 – 18 years of age). Twelve to 18 months of treatment with Replagal resulted in improvement in quality of life (QoL), as measured by validated instruments. After 6 months of therapy Replagal stabilised renal function compared with a decline in placebo treated patients. Kidney biopsy specimens revealed a significant increase in the fraction of normal glomeruli and a significant decrease in the fraction of glomeruli with mesangial widening in patients treated with Replagal in contrast to the patients treated with placebo. After 12 to 18 months of maintenance therapy, Replagal improved renal function as measured by inulin based glomerular filtration rate by 8.7 ± 3.7 ml/min. (p=0.030). Longer term therapy (48-54 months) resulted in stabilisation of GFR in male patients with normal baseline GFR (≥ 90 mL/min/1.73 m2) and with mild to moderate renal dysfunction (GFR 60 to < 90 mL/min/1.73 m2), and in slowing of the rate of decline in renal function and progression to end-stage renal disease in male Fabry patients with more severe renal dysfunction (GFR 30 to < 60 mL/min/1.73 m2). In a second study, fifteen patients with left ventricular hypertrophy completed a 6 month placebo-controlled study and entered an extension study. Treatment with Replagal resulted in an 11.5 g decrease in left ventricular mass as measured by magnetic resonance imaging (MRI) in the controlled study, while patients receiving placebo exhibited an increase in left ventricular mass of 21.8 g. In addition, in the first study involving 25 patients, Replagal effected a significant reduction in cardiac mass after 12 to 18 months of maintenance therapy (p<0.001). Replagal was also associated with improved myocardial contractility, a decrease in mean QRS duration and a concomitant decrease in septal thickness on echocardiography. Two patients with right bundle branch block in the studies conducted reverted to normal following therapy with Replagal. Subsequent open label studies demonstrated significant reduction from baseline in left ventricular mass by echocardiography in both male and female Fabry patients over 24 to 36 months of Replagal treatment. The reductions in LV mass observed by echocardiography in both male and female Fabry patients over 24 to 36 months of Replagal treatment were associated with meaningful symptom improvement as measured using the NYHA and CCS in Fabry patients with severe heart failure or anginal symptoms at baseline. Compared with placebo, treatment with Replagal also reduced accumulation of Gb3. After the first 6 months of therapy mean decreases of approximately 20 - 50 % were observed in plasma, urine sediment, liver, kidney, and heart biopsy samples. After 12 to 18 months treatment a reduction of 50 – 80% was observed in plasma and urine sediment. The metabolic effects were also associated with clinically significant weight gain, increased sweating and increased energy. Consistent with the clinical effects of Replagal, treatment with the enzyme reduced accumulation of Gb3 in many cell types, including renal glomerular and tubular epithelial cells, renal capillary endothelial cells (cardiac and dermal capillary endothelial cells were not examined) and cardiac myocytes. In male paediatric Fabry patients plasma Gb3 decreased 40-50% after 6 months of Replagal therapy 0.2 mg/kg and this reduction persisted after a total 4 years of treatment in 11 patients. Infusion of Replagal at home may be considered for patients who are tolerating their infusions well. Paediatric population In male paediatric Fabry patients ≥ 7 years of age, hyperfiltration can be the earliest manifestation of renal involvement in the disease. Reduction in their hypernormal eGFRs was observed within 6 months of initiating Replagal therapy. After one year of treatment with agalsidase alfa 0.2 mg/kg every other week, the abnormally high eGFR decreased from 143.4 ± 6.8 to 121.3 ± 5.6 mL/min/1.73 m2 in this subgroup and these eGFRs stabilized in the normal range during 4 years of Replagal 0.2 mg/kg therapy, as did the eGFRs of the non-hyperfiltrators. In male paediatric patients ≥ 7 years of age, heart rate variability was abnormal at baseline and improved after 6 months of Replagal therapy in 15 boys and the improvement was sustained through 6.5 years of Replagal 0.2 mg/kg therapy in an open-label long-term extension study in 9 boys. Among 9 boys with left ventricular mass (LVMI) indexed to height2.7 within the normal range for children (<39 g/m2.7 in boys) at baseline, LVMI remained stable at levels below the left ventricular hypertrophy (LVH) threshold throughout the 6.5 years of treatment. In a second study, in 14 patients ≥ 7 years of age, the results regarding heart rate variability were consistent with previous findings. In this study, only one patient had LVH at baseline and remained stable over time. For patients between 0 and 7 years of age, limited data indicate no specific safety issues. Study in patients switching from agalsidase beta to Replagal (agalsidase alfa) 100 patients [(naïve (n=29); or previously treated with agalsidase beta who switched to Replagal (n=71)) were treated for up to 30 months in an open label, uncontrolled study. An analysis showed that serious adverse events were reported in 39.4% of those patients who switched from agalsidase beta compared to 31.0% in those who were naïve to therapy prior to study entry. Patients switched from agalsidase beta to Replagal had a safety profile consistent with that observed in other clinical experience. Infusion related reactions have been experienced by 9 patients of the naïve population (31.0%) compared to 27 patients of the switched population (38.0%). Study with various dosing regimen In an open-label randomised study, there were no statistically significant differences between adult patients treated for 52 weeks with 0.2 mg/kg intravenously every other week (n=20) and those treated with 0.2 mg/kg weekly (n=19) in mean change from baseline LVMI or other endpoints (cardiac functional status, renal function, and pharmacodynamic activity). In each treatment group, LVMI remained stable over the treatment period of the study. The overall incidence of SAEs by treatment group did not show any obvious effect of treatment regimen on the SAE profile of the different treatment groups. Immunogenicity Antibodies to agalsidase alfa have not been shown to be associated with any clinically significant effects on safety (e.g. infusion reactions) or efficacy.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Single doses ranging from 0.007 - 0.2 mg enzyme per kg body weight were administered to adult male patients as 20 - 40 minute intravenous infusions while female patients received 0.2 mg enzyme per kg body weight as 40 minute infusions. The pharmacokinetic properties were essentially unaffected by the dose of the enzyme. Following a single intravenous dose of 0.2 mg/kg, agalsidase alfa had a biphasic distribution and elimination profile from the circulation. Pharmacokinetic parameters were not significantly different between male and female patients. Elimination half-lives were 108 ± 17 minutes in males compared to 89 ± 28 minutes in females and volume of distribution was approximately 17% body weight in both sexes. Clearance normalised for body weight was 2.66 and 2.10 ml/min/kg for males and females, respectively. Based on the similarity of pharmacokinetic properties of agalsidase alfa in both males and females, tissue distribution in major tissues and organs is also expected to be comparable in male and female patients. Following six months of Replagal treatment 12 of 28 male patients showed altered pharmacokinetics including an apparent increase in clearance. These changes were associated with the development of low titre antibodies to agalsidase alfa but no clinically significant effects on safety or efficacy were observed in the patients studied. Based on the analysis of pre- and post-dose liver biopsies in males with Fabry Disease, the tissue half- life has been estimated to be in excess of 24 hours and hepatic uptake of the enzyme estimated to be 10% of administered dose. Agalsidase alfa is a protein. It is not expected to bind to proteins. It is expected that its metabolic degradation will follow the pathways of other proteins, i.e. peptide hydrolysis. Agalsidase alfa is unlikely to be a candidate for drug- drug interactions. Renal impairment Renal elimination of agalsidase alfa is considered to be a minor clearance pathway since pharmacokinetic parameters are not altered by impaired renal function. Hepatic impairment As metabolism is expected to occur by peptide hydrolysis, impaired liver function is not expected to affect the pharmacokinetics of agalsidase alfa in a clinically significant manner. Paediatric population In children (aged 7-18 years), Replagal administered at 0.2 mg/kg was cleared faster from the circulation than in adults. Mean clearance of Replagal in children aged (7-11 years), in adolescents (aged 12-18 years), and adults was 4.2 ml/min/kg, 3.1 ml/min/kg, and 2.3 ml/min/kg, respectively. Pharmacodynamic data suggest that at a dose of 0.2 mg/kg Replagal, the reductions in plasma Gb3 are more or less comparable between adolescents and young children (see section 5.1).

מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| AGALSIDASE ALFA | ||||
| AGALSIDASE BETA |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/03/2002
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
