Quest for the right Drug
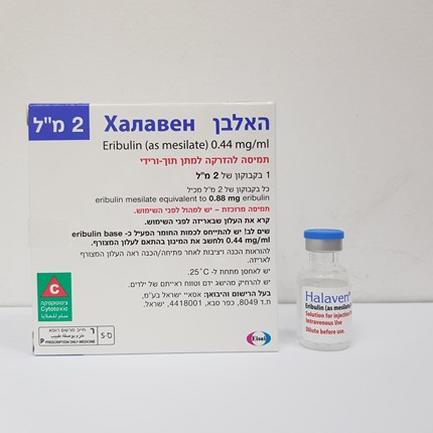
האלבן HALAVEN (ERIBULIN AS MESILATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי : I.V
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic properties Pharmacotherapeutic group: Other antineoplastic agents, ATC code: L01XX41 Eribulin mesilate is a microtubule dynamics inhibitor belonging to the halichondrin class of antineoplastic agents. It is a structurally simplified synthetic analogue of halichondrin B, a natural product isolated from the marine sponge Halichondria okadai. Eribulin inhibits the growth phase of microtubules without affecting the shortening phase and sequesters tubulin into non-productive aggregates. Eribulin exerts its effects via a tubulin-based antimitotic mechanism leading to G2/M cell-cycle block, disruption of mitotic spindles, and, ultimately, apoptotic cell death after prolonged and irreversible mitotic blockage. Clinical efficacy Breast cancer The efficacy of HALAVEN in breast cancer is primarily supported by two randomized Phase 3 comparative studies. The 762 patients in the pivotal Phase 3 EMBRACE study (Study 305) had locally recurrent or metastatic breast cancer, and had previously received at least two and a maximum of five chemotherapy regimens, including an anthracycline and a taxane (unless contraindicated). Patients must have progressed within 6 months of their last chemotherapeutic regimen. The HER2 status of the patients was: 16.1% positive, 74.2% negative and 9.7% unknown, whilst 18.9% of patients were triple negative. They were randomized 2:1 to receive either HALAVEN, or treatment of physician’s choice (TPC), which consisted of 97% chemotherapy (26% vinorelbine, 18% gemcitabine, 18% capecitabine, 16% taxane, 9% anthracycline, 10% other chemotherapy), or 3% hormonal therapy. The study met its primary endpoint with an overall survival (OS) result that was statistically significantly better in the eribulin group compared to TPC at 55% of events. This result was confirmed with an updated overall survival analysis carried out at 77% of events. Study 305 - Updated Overall Survival ( ITT Population) Efficacy Parameter HALAVEN TPC 1.0 (n=508) (n=254) HALAVEN 0.9 Overall Survival PROPORTION OF PATIENTS ALIVE 0.8 Number of Events 386 203 0.7 Median (months) 13.2 10.5 Treatment of 0.6 Hazard Ratio (95% CI)a 0.805 (0.677, 0.958) Physician’s Choice (TPC) 0.5 Nominal P value 0.014b (log rank) 0.4 a Cox proportional hazard b Stratified by geographic region, HER2/neu status, 0.3 and prior capecitabine therapy. 0.2 0.1 0.0 TIME (months) NUMBER OF PATIENTS AT RISK HALAVEN 508 406 274 142 54 11 0 TPC 254 178 106 61 26 5 0 By independent review, the median progression free survival (PFS) was 3.7 months for eribulin compared to 2.2 months for the TPC arm (HR 0.865, 95% CI: 0.714, 1.048, p=0.137). In response evaluable patients, the objective response rate by the RECIST criteria was 12.2% (95% CI: 9.4%, 15.5%) by independent review for the eribulin arm compared to 4.7% (95% CI: 2.3%, 8.4%) for the TPC arm. The positive effect on OS was seen in both taxane-refractory and non-refractory groups of patients . In the OS update, the HR for eribulin versus TPC was 0.90 (95% CI: 0.71, 1.14) in favour of eribulin for taxane-refractory patients and 0.73 (95% CI: 0.56, 0.96) for patients not taxane-refractory. The positive effect on OS was seen both in capecitabine-naïve and in capecitabine pre-treated patient groups. The updated OS analysis showed a survival benefit for the eribulin group compared to TPC both in capecitabine pre-treated patients with a HR of 0.787 (95% CI: 0.645, 0.961), and for the capecitabine-naïve patients with a corresponding HR of 0.865 (95% CI: 0.606, 1.233). The second Phase 3 study in earlier line metastatic breast cancer, Study 301, was an open-label, randomized, study in patients (n=1102) with locally advanced or metastatic breast cancer to investigate the efficacy of HALAVEN monotherapy compared to capecitabine monotherapy in terms of OS and PFS as co-primary endpoint. Patients had previously received up to three prior chemotherapy regimens, including both an anthracycline and a taxane and a maximum of two for advanced disease, with the percentage who had received 0, 1 or 2 prior chemotherapy treatments for metastatic breast cancer being 20.0%, 52.0% or 27.2% respectively. The HER2 status of the patients was: 15.3% positive, 68.5% negative and 16.2% unknown, whilst 25.8% of patients were triple negative. Study 301 - Overall Survival (ITT Population) Efficacy Parameter OS in ITT Population HALAVEN Capecitabine 1.0 (n=554) (n=548) HALAVEN Number of Events 446 459 0.9 Median (months) 15.9 14.5 0.8 PROBABILITY OF SURVIVAL Hazard Ratio (95% CI)a 0.879 (0.770, 1.003) 0.7 Capecitabine P value (log rank) 0.056b 0.6 a Cox proportional hazard b Stratified by geographic region, HER2/neu status 0.5 0.4 0.3 0.2 0.1 0.0 TIME (months) NUMBER OF PATIENTS AT RISK HALAVEN 554 530 505 464 423 378 349 320 268 243 214 193 173 151 133 119 99 77 52 38 32 26 22 15 13 9 7 2 2 0 Capecitabine 548 513 466 426 391 352 308 277 242 214 191 175 155 135 122 108 81 62 42 33 27 23 17 13 12 10 2 2 1 0 Progression free survival assessed by independent review was similar between eribulin and capecitabine with medians of 4.1 months vs 4.2 months (HR 1.08; [95% CI: 0.932, 1.250]) respectively. Objective response rate as assessed by independent review was also similar between eribulin and capecitabine; 11.0% (95% CI: 8.5, 13.9) in the eribulin group and 11.5% (95% CI: 8.9, 14.5) in the capecitabine group. The overall survival in patients in HER2 negative and HER2 positive patients in the eribulin and control groups in Study 305 and Study 301 is shown below: Study 305 Updated Overall Survival ITT Population Efficacy Parameter HER2 Negative HER2 Positive HALAVEN TPC HALAVEN TPC (n = 373) (n = 192) (n = 83) (n = 40) Number of Events 285 151 66 37 Median months 13.4 10.5 11.8 8.9 Hazard Ratio (95% CI) 0.849 (0.695, 1.036) 0.594 (0.389, 0.907) p-value (log rank) 0.106 0.015 Study 301 Overall Survival ITT Population Efficacy Parameter HER2 Negative HER2 Positive HALAVEN Capecitabine HALAVEN Capecitabine (n = 375) (n = 380) (n = 86) (n = 83) Number of Events 296 316 73 73 Median months 15.9 13.5 14.3 17.1 Hazard Ratio (95% CI) 0.838 (0.715, 0.983) 0.965 (0.688, 1.355) p-value (log rank) 0.030 0.837 Note: Concomitant anti-HER2 therapy was not included in Study 305 and Study 301. Liposarcoma In liposarcoma the efficacy of eribulin is supported by the pivotal Phase 3 sarcoma study (Study 309). The patients in this study (n=452) had locally recurrent, inoperable and/or metastatic soft tissue sarcoma of one of two subtypes – leiomyosarcoma or liposarcoma. Patients had received at least two prior chemotherapy regimens, one of which must have been an anthracycline (unless contraindicated). Patients must have progressed within 6 months of their last chemotherapeutic regimen. They were randomized 1:1 to receive either eribulin 1.23 mg/m2 on days 1 and 8 of a 21 day cycle or dacarbazine 850 mg/m2, 1000 mg/m2 or 1200 mg/m2 (dose determined by the investigator prior to randomization), every 21 days. In Study 309, a statistically significant improvement in OS was observed in patients randomized to the eribulin arm compared to the control arm. This translated into a 2 month improvement in median OS (13.5 months for eribulin treated patients vs. 11.5 months for dacarbazine treated patients). There was no significant difference in progression-free survival or overall response rate between the treatment arms in the overall population. Treatment effects of eribulin were limited to patients with liposarcoma (45% dedifferentiated, 37% myxoid/round cell and 18% pleomorphic in Study 309) based on pre-planned subgroup analyses of OS and PFS. There was no difference in efficacy between eribulin and dacarbazine in patients with advanced or metastatic leiomyosarcoma. Study 309 Study 309 Study 309 Liposarcoma Subgroup Leiomyosarcoma Subgroup ITT Population HALAVEN Dacarbazine HALAVEN Dacarbazine HALAVEN Dacarbazine (n=71) (n=72) (n=157) (n=152) (n=228) (n=224) Overall survival Number of 52 63 124 118 176 181 Events Median 15.6 8.4 12.7 13.0 13.5 11.5 months Hazard Ratio 0.511 (0.346, 0.753) 0.927 (0.714, 1.203) 0.768 (0.618, 0.954) (95% CI) Nominal p- 0.0006 0.5730 0.0169 value Progression-free survival Number of 57 59 140 129 197 188 Events Median 2.9 1.7 2.2 2.6 2.6 2.6 months Hazard Ratio 0.521 (0.346, 0.784) 1.072 (0.835, 1.375) 0.877 (0.710, 1.085) (95% CI) Nominal p- 0.0015 0.5848 0.2287 value Study 309 - Overall Survival in the Liposarcoma Subgroup PROBABILITY OF SURVIVAL Time (months) NUMBER OF PATIENTS AT RISK: HALAVEN 71 63 51 43 39 34 30 20 15 12 7 4 2 0 Dacarbazine 72 59 42 33 22 17 12 11 6 3 2 0 0 0 Study 309 – Progression Free Survival in the Liposarcoma Subgroup PROBABILITY OF SURVIVAL HALAVEN Dacarbazine Time (months) NUMBER OF PATIENTS AT RISK: HALAVEN 71 28 17 12 9 3 1 0 Dacarbazine 72 15 5 2 1 0 0 0 Paediatric population Breast Cancer Soft Tissue Sarcoma Efficacy of eribulin was assessed but not established in three open-label studies: Study 113 was a Phase 1, open-label, multicentre, dose-finding study that assessed eribulin in paediatric patients with refractory or recurrent solid tumours and lymphomas but excluding CNS tumours. A total of 22 paediatric patients (age range: 3 to 17 years) were enrolled and treated. The patients were administered eribulin intravenously on Days 1 and 8 of a 21-day cycle at three dose levels (0.97, 1.23 and 1.58 mg/m2). The maximum tolerated dose (MTD)/recommended Phase 2 dose (RP2D) of eribulin was determined as 1.23 mg/m2 on Days 1 and 8 of a 21-day cycle. Study 223 was a Phase 2, open-label, multicentre study that assessed the safety and preliminary activity of eribulin in paediatric patients with refractory or recurrent rhabdomyosarcoma (RMS), non- rhabdomyosarcoma soft tissue sarcoma (NRSTS) or Ewing sarcoma (EWS). Twenty-one paediatric patients (age range: 2 to 17 years) were enrolled and treated with eribulin at a dose of 1.23 mg/m2 intravenously on Days 1 and 8 of a 21-day cycle (the RP2D from Study 113). No patient achieved confirmed partial response (PR) or complete response (CR). Study 213 was a Phase 1/2, open-label, multicentre study to evaluate the safety and efficacy of eribulin in combination with irinotecan hydrochloride in paediatric patients with relapsed/refractory solid tumours and lymphomas but excluding CNS tumours (Phase 1), and to assess the efficacy of the combination treatment in paediatric patients with relapsed/refractory RMS, NRSTS and EWS (Phase 2). A total of 40 paediatric patients were enrolled and treated in this study. In Phase 1, 13 paediatric patients (age range: 4 to 17 years) were enrolled and treated; the RP2D was determined as eribulin 1.23 mg/m2 on Days 1 and 8 with irinotecan hydrochloride 40 mg/m2 on Days 1 to 5 of a 21-day cycle. In Phase 2, 27 paediatric patients (age range: 4 to 17 years) were enrolled and treated at the RP2D. Three patients had confirmed PR (1 patient in each of the RMS, NRSTS, and EWS histology cohorts). The objective response rate (ORR) was 11.1%. No new safety signals were observed in the three paediatric studies (see section 4.8); however, due to the small patient populations no firm conclusions can be made.
Pharmacokinetic Properties
5.2 Pharmacokinetic properties Distribution The pharmacokinetics of eribulin are characterized by a rapid distribution phase followed by a prolonged elimination phase, with a mean terminal half-life of approximately 40 h. It has a large volume of distribution (range of means 43 to 114 l/m2). Eribulin is weakly bound to plasma proteins. The plasma protein binding of eribulin (100-1000 ng/ml) ranged from 49% to 65% in human plasma. Biotransformation Unchanged eribulin was the major circulating species in plasma following administration of 14C-eribulin to patients. Metabolite concentrations represented <0.6% of parent compound, confirming that there are no major human metabolites of eribulin. Elimination Eribulin has a low clearance (range of means 1.16 to 2.42 l/h/m2). No significant accumulation of eribulin is observed on weekly administration. The pharmacokinetic properties are not dose or time dependent in the range of eribulin doses of 0.22 to 3.53 mg/m2. Eribulin is eliminated primarily by biliary excretion. The transport protein involved in the excretion is presently unknown. Preclinical in vitro studies indicate that eribulin is transported by Pgp. However it has been shown that at clinically relevant concentrations eribulin is not a Pgp inhibitor in vitro. Additionally, in vivo, concomitant administration of ketoconazole, a Pgp inhibitor, has no effect on eribulin exposure (AUC and Cmax). In vitro studies have also indicated that eribulin is not a substrate for OCT1. After administration of 14C-eribulin to patients, approximately 82% of the dose was eliminated in faeces and 9% in urine indicating that renal clearance is not a significant route of eribulin elimination. Unchanged eribulin represented most of the total radioactivity in faeces and urine. Hepatic impairment A study evaluated the pharmacokinetics of eribulin in patients with mild (Child-Pugh A; n=7) and moderate (Child-Pugh B; n=4) hepatic impairment due to liver metastases. Compared to patients with normal hepatic function (n=6), eribulin exposure increased 1.8-fold and 3-fold in patients with mild and moderate hepatic impairment, respectively. Administration of HALAVEN at a dose of 0.97 mg/m2 to patients with mild hepatic impairment and 0.62 mg/m2 to patients with moderate hepatic impairment resulted in a somewhat higher exposure than after a dose of 1.23 mg/m2 to patients with normal hepatic function. HALAVEN was not studied in patients with severe hepatic impairment (Child-Pugh C). There is no study in patients with hepatic impairment due to cirrhosis. See section 4.2 for dosage recommendation. Renal impairment Increased eribulin exposure was seen in some patients with moderately or severely impaired renal function, with high between-subject variability. The pharmacokinetics of eribulin were evaluated in a Phase 1 study in patients with normal renal function (Creatinine clearance: ≥ 80 ml/min; n=6), moderate (30-50 ml/min; n=7) or severe (15-<30 ml/min; n=6) renal impairment. Creatinine clearance was estimated with the Cockcroft-Gault formula. A 1.5-fold (90% CI: 0.9-2.5) higher dose-normalised AUC(0-inf) was observed in patients with moderate and severe renal impairment. See section 4.2 for treatment recommendations. Paediatric population Eribulin plasma concentrations were collected from 83 paediatric patients (age range: 2 to 17 years), with refractory/relapsed and recurrent solid tumours and lymphomas, who received eribulin in Studies 113, 213 and 223. Eribulin PK in paediatric patients was comparable to adult patients with STS and patients with other types of tumour. Eribulin exposure in paediatric patients was similar to exposure in adult patients. Concomitant irinotecan did not have an effect on eribulin PK in paediatric patients with refractory/relapsed and recurrent solid tumours.

פרטי מסגרת הכללה בסל
א. התרופה תינתן לטיפול במקרים האלה:1. סרטן שד מתקדם מקומי או גרורתי מסוג TNBC (triple negative breast cancer) בחולה שמחלתו התקדמה לאחר קו טיפול כימותרפי קודם למחלתו המתקדמת.2. ליפוסרקומה לא נתיחה בחולה בגיר שקיבל טיפול קודם שכלל תרופה ממשפחת האנתראציקלינים למחלתו המתקדמת או הגרורתית.ב. מתן התרופה האמורה ייעשה לפי מרשם של מומחה באונקולוגיה.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| ליפוסרקומה לא נתיחה בחולה בגיר שקיבל טיפול קודם שכלל תרופה ממשפחת האנתראציקלינים למחלתו המתקדמת או הגרורתית. | 21/01/2016 | |||
| סרטן שד מתקדם מקומי או גרורתי מסוג TNBC (triple negative breast cancer) בחולה שמחלתו התקדמה לאחר קו טיפול כימותרפי קודם למחלתו המתקדמת. | 21/01/2016 |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
21/01/2016
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
