Quest for the right Drug
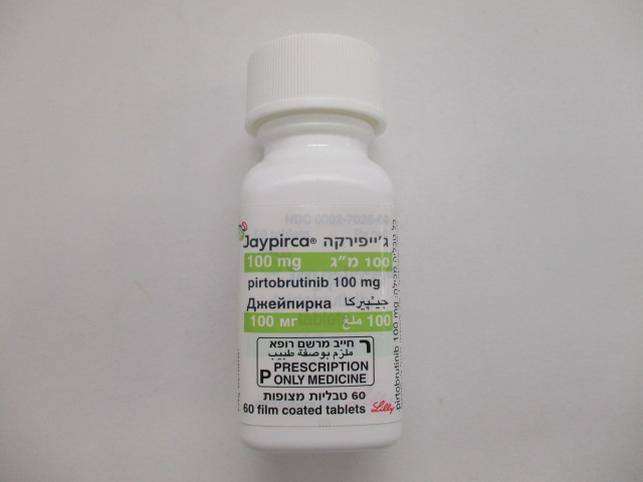
ג'ייפירקה 100 מ"ג JAYPIRCA 100 MG (PIRTOBRUTINIB)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
פומי : PER OS
צורת מינון:
טבליות מצופות פילם : FILM COATED TABLETS
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Adverse reactions : תופעות לוואי
7 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in the labeling: • Infections [see Warnings and Precautions (6.1)] • Hemorrhage [see Warnings and Precautions (6.2)] • Cytopenias [see Warnings and Precautions (6.3)] • Atrial Fibrillation and Atrial Flutter [see Warnings and Precautions (6.4)] • Second Primary Malignancies [see Warnings and Precautions (6.5)] • Hepatotoxicity, including DILI [see Warnings and Precautions (6.6)] 7.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be compared to rates in the clinical trials of another drug and may not reflect the rates observed in the general patient population. The data in the WARNINGS AND PRECAUTIONS reflect exposure to JAYPIRCA as a single-agent, administered at 200 mg once daily in 593 patients with hematologic malignancies in the BRUIN study. Among these 593 patients, the median duration of exposure was 10 months, 62% were exposed for at least 6 months and 45% were exposed for at least one year. In this pooled safety population, the most common (≥ 20%) adverse reactions, including laboratory abnormalities, were decreased neutrophil count (46%), decreased hemoglobin (39%), fatigue (32%), decreased lymphocyte count (31%), musculoskeletal pain (30%), decreased platelet count (29%), diarrhea (24%), COVID-19 (22%), bruising (21%), and cough (20%). Mantle Cell Lymphoma BRUIN The safety of JAYPIRCA was evaluated in the BRUIN trial in patients with MCL who received a prior BTK inhibitor [see Clinical Studies (14.1)]. The trial required a platelet count ≥ 50 x 109/L, absolute neutrophil count ≥ 0.75 x 109/L, hepatic transaminases ≤ 2.5 times upper limit of normal (ULN), and an ECOG performance status of 0 to 2. The trial excluded patients with active central nervous system (CNS) involvement by lymphoma, significant cardiovascular disease, major bleeding or grade ≥ 3 arrhythmia with a prior BTK inhibitor, prolonged QTc interval, or need for a strong CYP3A inhibitor or inducer or strong P-gp inhibitor. Patients received JAYPIRCA 200 mg orally once daily until disease progression or unacceptable toxicity (n = 128); 36% were exposed for 6 months or longer and 10% were exposed for at least one year. The median number of prior therapies was 3 (range: 1-9). The median age was 71 years (range: 46 to 88 years) and 80% of patients were male. Race was reported for all patients; 78% were White, 14% were Asian, 2.3% were Black, and 2.3% were Hispanic or Latino. Serious adverse reactions occurred in 38% of patients who received JAYPIRCA. Serious adverse reactions that occurred in ≥ 2% of patients were pneumonia (14%), COVID-19 (4.7%), musculoskeletal pain (3.9%), hemorrhage (2.3%), pleural effusion (2.3%), and sepsis (2.3%). Fatal adverse reactions within 28 days of the last dose of JAYPIRCA occurred in 7% of patients, most commonly due to infections (4.7%) including COVID-19 (3.1% of all patients). Adverse reactions led to dose reductions in 4.7%, treatment interruption in 32%, and permanent discontinuation of JAYPIRCA in 9%. Adverse reactions that resulted in dosage modification in > 5% of patients included pneumonia and neutropenia. Adverse reactions which resulted in permanent discontinuation of JAYPIRCA in > 1% of patients included pneumonia. The most common adverse reactions (≥ 15%), excluding laboratory terms, were fatigue, musculoskeletal pain, diarrhea, edema, dyspnea, pneumonia, and bruising. Table 2 summarizes select adverse reactions in BRUIN. Table 2: Adverse Reactions (≥ 10%) in Patients with MCL Who Received JAYPIRCA JAYPIRCA 200 mg once daily N = 128 Adverse Reactions a All Grades (%) Grade 3-4 (%) General Disorders Fatigue 29 1.6 Edema 18 0.8 Fever 13 - Musculoskeletal and Connective Tissue Disorders Musculoskeletal pain 27 3.9 Arthritis or arthralgia 12 0.8 Gastrointestinal Disorders Diarrhea 19 - Constipation 13 - Abdominal pain 11 0.8 Nausea 11 - Respiratory, thoracic, and mediastinal disorders Dyspnea 17 2.3 Cough 14 - Injury Bruising 16 - Infections Pneumonia 16 b 14 Upper respiratory tract infections 10 0.8 Nervous system disorders Peripheral neuropathy 14 0.8 Dizziness 10 - Skin and subcutaneous disorders Rash 14 - Vascular disorders Hemorrhage 11 c 3.1 a Each term listed includes other related terms. b includes 1 fatality from COVID-19 pneumonia c includes 1 fatality from hemorrhage Clinically relevant adverse reactions in < 10% include vision changes, memory changes, headache, urinary tract infection, herpesvirus infection, and tumor lysis syndrome. Table 3 summarizes laboratory abnormalities in BRUIN. Table 3: Select Laboratory Abnormalities (≥ 10%) That Worsened from Baseline in Patients with MCL Who Received JAYPIRCA JAYPIRCA a 200 mg once daily Laboratory Abnormality All Grades (%) Grade 3 or 4 (%) Hematology Hemoglobin decreased 42 9 Platelet count decreased 39 14 Neutrophil count decreased 36 16 Lymphocyte count decreased 32 15 Chemistry Creatinine increased 30 1.6 Calcium decreased 19 1.6 AST increased 17 1.6 Potassium decreased 13 1.6 Sodium decreased 13 - Lipase increased 12 4.4 Alkaline phosphatase increased 11 - ALT increased 11 1.6 Potassium increased 11 0.8 a The denominator used to calculate the rate varied from 90 to 127 based on the number of patients with a baseline value and at least one post- treatment value. Grade 4 laboratory abnormalities in > 5% of patients included neutrophils decreased (10%), platelets decreased (7%), and lymphocytes decreased (6%). Lymphocytosis: Upon initiation of JAYPIRCA, a temporary increase in lymphocyte counts (defined as absolute lymphocyte count increased ≥ 50% from baseline and a post-baseline value ≥ 5,000/µL) occurred in 34% of MCL patients in BRUIN. The median time to onset of lymphocytosis was 1.1 weeks, with 75% of cases occurring within 2.1 weeks, and the median duration was 11 weeks. Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma BRUIN The safety of JAYPIRCA was evaluated in the BRUIN trial in 110 patients with CLL/SLL, with 98% receiving at least two prior lines of systemic therapy including a BTK inhibitor and a BCL-2 inhibitor [see Clinical Studies (14.2)]. The trial required a platelet count ≥ 50 x 109/L, absolute neutrophil count ≥ 0.75 x 109/L, hepatic transaminases ≤ 2.5 times upper limit of normal (ULN), and an ECOG performance status of 0 to 2. The trial excluded patients with active central nervous system (CNS) involvement by lymphoma, significant cardiovascular disease, major bleeding, uncontrolled or symptomatic arrhythmias, prolonged QTc interval, or need for a strong CYP3A inhibitor or inducer or strong P-gp inhibitor. Patients received JAYPIRCA 200 mg orally once daily until disease progression or unacceptable toxicity (N = 110); 60% were exposed for at least 1 year and 14% were exposed for at least two years. The median age was 68 years (range: 41 to 88 years) and 67% of patients were male. Race was reported in 110 (100%) patients; of these patients, 89% were White, 4.5% were Black, 1.8% were Asian, and 1.8% were Hispanic or Latino. The median number of prior therapies was 5 (range: 1-11). Serious adverse reactions occurred in 56% of patients who received JAYPIRCA. Serious adverse reactions that occurred in ≥ 5% of patients were pneumonia (18%), COVID-19 (9%), sepsis (7%), and febrile neutropenia (7%). Fatal adverse reactions within 28 days of the last dose of JAYPIRCA occurred in 11% of patients, most commonly due to infections (10%), including sepsis (5%) and COVID-19 (2.7%). Adverse reactions led to dose reductions in 3.6%, treatment interruption in 42%, and permanent discontinuation of JAYPIRCA in 9%. Adverse reactions which resulted in dose reductions of JAYPIRCA in > 1% of patients included neutropenia. Adverse reactions which resulted in treatment interruptions of JAYPIRCA in > 5% of patients included pneumonia, neutropenia, febrile neutropenia, and COVID-19. Adverse reactions which resulted in permanent discontinuation of JAYPIRCA in > 1% of patients included second primary malignancy, COVID-19, and sepsis. The most common adverse reactions (≥ 20%), excluding laboratory terms, were fatigue, bruising, cough, musculoskeletal pain, COVID-19, diarrhea, pneumonia, abdominal pain, dyspnea, hemorrhage, edema, nausea, pyrexia, and headache. Table 4 summarizes select adverse reactions for patients treated on BRUIN. Table 4: Adverse Reactions (≥ 10%) in Patients with CLL/SLL Who Received JAYPIRCA JAYPIRCA 200 mg once daily N = 110 Adverse Reactions a All Grades (%) Grade 3-4 (%) General Disorders Fatigue 36 2.7 Edema 21 0 Pyrexia 20 2.7 Injury Bruising 36 0 Fall 14 0.9 Respiratory, thoracic, and mediastinal disorders Cough 33 0 Dyspnea 22 2.7 Mucositis 12 0.9 Musculoskeletal and Connective Tissue Disorders Musculoskeletal pain 32 0.9 Arthritis or arthralgia 19 1.8 Infections COVID-19 28b 7 Pneumonia 27c 16 Upper respiratory tract infections 13 2.7 Respiratory tract infection 11 1.8 Gastrointestinal Disorders Diarrhea 26 0 Abdominal pain 25 2.7 Nausea 21 0 Constipation 14 0 Vascular disorders JAYPIRCA 200 mg once daily N = 110 Adverse Reactions a All Grades (%) Grade 3-4 (%) Hemorrhage 22d 2.7 Hypertension 12 5 Nervous system disorders Headache 20 0.9 Peripheral neuropathy 16 3.6 Dizziness 15 0 Neurological changes 12e 2.7 Skin and subcutaneous disorders Rash 19 0.9 Psychiatric disorders Insomnia 14 0 Neoplasms benign, malignant and unspecified Second primary malignancy 13f 2.7 Renal and urinary disorders Renal insufficiency 12g 6 Metabolism and nutrition disorders Decreased appetite 12 0 Cardiac disorders Supraventricular tachycardia 10h 5 a Each term listed includes other related terms. b Includes COVID-19 pneumonia. Includes 1 fatalities from COVID-19 and 2 fatalities from COVID-19 pneumonia c Includes COVID-19 pneumonia. Includes 2 fatalities from COVID-19 pneumonia and 1 fatality from pneumonia d Includes preferred terms hemorrhage, intracranial hemorrhage, and gastrointestinal hemorrhage e Includes preferred terms memory impairment, confusional state, encephalopathy, mental status changes f Includes preferred terms second primary malignancy and nonmelanoma skin cancers. 1 fatality from metastatic malignant melanoma g Includes preferred terms renal failure, chronic kidney disease, acute kidney injury h Includes preferred terms supraventricular tachycardia, sinus tachycardia, atrial fibrillation Clinically relevant adverse reactions in < 10% include vision changes, lower respiratory tract infection, urinary tract infection, herpesvirus infection, and tumor lysis syndrome. Table 5 summarizes laboratory abnormalities in BRUIN. Table 5: Select Laboratory Abnormalities (≥ 20%) That Worsened from Baseline in Patients with CLL/SLL Who Received JAYPIRCA JAYPIRCA a 200 mg once daily Laboratory Abnormality All Grades (%) Grade 3 or 4 (%) Hematology Neutrophil count decreased 63 45 Hemoglobin decreased 48 19 JAYPIRCA a 200 mg once daily Laboratory Abnormality All Grades (%) Grade 3 or 4 (%) Platelet count decreased 30 15 Lymphocyte count decreased 23 8 Chemistry Calcium decreased 40 2.8 Sodium decreased 30 0 ALT increased 23 2.8 AST increased 23 1.9 Creatinine increased 23 0 Lipase increased 21 7 Alkaline phosphatase increased 21 0 a The denominator used to calculate the rate varied from 83 to 108 based on the number of patients with a baseline value and at least one post-treatment value. Grade 4 laboratory abnormalities in > 5% of patients included neutrophils decreased (23%). **Lymphocytosis: Upon initiation of JAYPIRCA, a temporary increase in lymphocyte counts (defined as absolute lymphocyte count increased ≥ 50% from baseline and a post-baseline value ≥ 5,000/µL) occurred in 64% of CLL/SLL patients in BRUIN. The median time to onset of lymphocytosis was 1.1 weeks, with 75% of cases occurring within 1.1 weeks, and the median duration was 19 weeks. Reporting of suspected adverse reactions Reporting suspected adverse reactions after authorization of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Any suspected adverse events should be reported to the Ministry of Health according to the National Regulation by using an online form https://sideeffects.health.gov.il

שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
לא צוין
הגבלות
לא צוין
מידע נוסף
עלון מידע לצרכן
30.01.24 - עלון לצרכן עברית 14.02.24 - עלון לצרכן עברית 21.03.24 - עלון לצרכן אנגלית 21.03.24 - עלון לצרכן ערבית 20.06.24 - עלון לצרכן עברית 02.08.24 - עלון לצרכן אנגלית 11.08.24 - עלון לצרכן ערבית 10.10.24 - עלון לצרכן עברית 11.11.24 - עלון לצרכן אנגלית 11.11.24 - עלון לצרכן ערבית 20.06.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
ג'ייפירקה 100 מ"ג