Quest for the right Drug
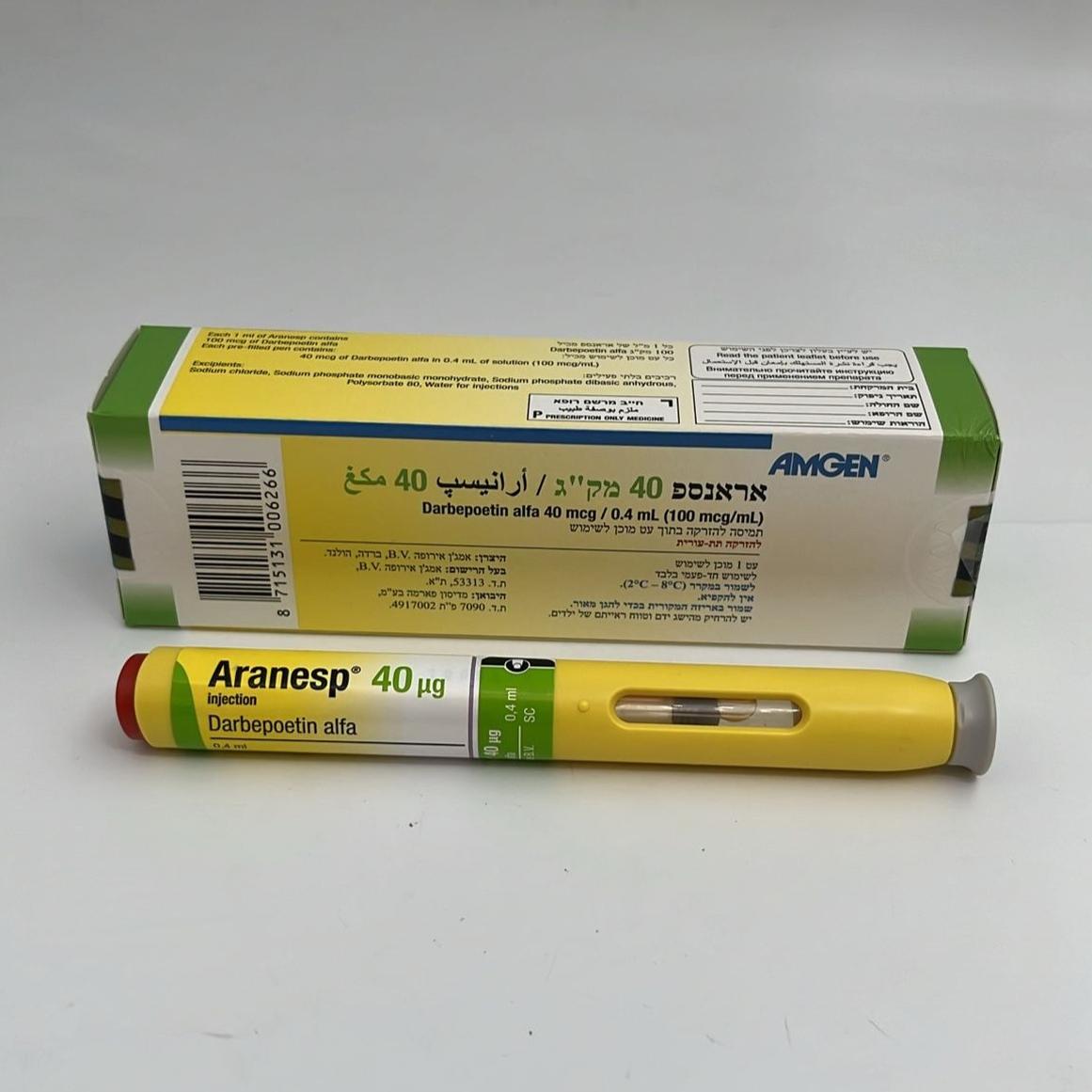
אראנספ 40 מק"ג ARANESP 40 MCG (DARBEPOETIN ALFA)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
תוך-ורידי, תת-עורי : I.V, S.C
צורת מינון:
תמיסה להזרקה : SOLUTION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Pharmacological properties : תכונות פרמקולוגיות
Pharmacodynamic Properties
5.1 Pharmacodynamic Properties Pharmacotherapeutic group: Anti-anemic preparations, other anti-anemic preparations, ATC Code: B03XA02. Mechanism of action Human erythropoietin is an endogenous glycoprotein hormone that is the primary regulator of erythropoiesis through specific interaction with the erythropoietin receptor on the erythroid progenitor cells in the bone marrow. The production of erythropoietin primarily occurs in and is regulated by the kidney in response to changes in tissue oxygenation. Production of endogenous erythropoietin is impaired in patients with chronic renal failure and the primary cause of their anemia is due to erythropoietin deficiency. In patients with cancer receiving chemotherapy the etiology of anemia is multifactorial. In these patients, erythropoietin deficiency and a reduced response of erythroid progenitor cells to endogenous erythropoietin both contribute significantly towards their anemia. Pharmacodynamic effects Darbepoetin alfa stimulates erythropoiesis by the same mechanism as the endogenous hormone. Darbepoetin alfa has five N-linked carbohydrate chains whereas the endogenous hormone and recombinant human erythropoietins (r-HuEPO) have three. The additional sugar residues are molecularly indistinct from those on the endogenous hormone. Due to its increased carbohydrate content darbepoetin alfa has a longer terminal half-life than r-HuEPO and consequently a greater in vivo activity. Despite these molecular changes, darbepoetin alfa retains a very narrow specificity for the erythropoietin receptor. Clinical efficacy and safety Chronic Renal Failure Patients Patients with CRF experienced greater risks for death and serious cardiovascular events when administered ESAs to target higher versus lower hemoglobin levels 13.5 g/dL (8.4 mmol/L) versus 11.3 g/dL (7.1 mmol/L); 14 g/dL (8.7 mmol/L) versus 10 g/dL (6.2 mmol/L) in two clinical studies. In a randomized, double-blind correction study (n = 358) comparing once every two-week and once monthly dosing schedules in patients with CRF not on dialysis, darbepoetin alfa once monthly dosing was non-inferior to once every two-week dosing for correcting anemia. The median (quartile 1, quartile 3) time to achieve hemoglobin correction (≥ 10.0 g/dL and ≥ 1.0 g/dL increase from baseline) was 5 weeks for both once every two-week (3, 7 weeks) and once monthly dosing (3, 9 weeks). During the evaluation period (weeks 29-33), the mean (95% CI) weekly equivalent dose was 0.20 (0.17, 0.24) mcg/kg in the once every two-week arm and 0.27 (0.23, 0.32) mcg/kg in the once monthly arm. In a randomized, double-blind, placebo-controlled study (TREAT) of 4,038 CRF patients not on dialysis with type 2 diabetes and hemoglobin levels ≤ 11 g/dL, patients received either treatment with darbepoetin alfa to target hemoglobin levels of 13 g/dL or placebo (with darbepoetin alfa rescue at hemoglobin less than 9 g/dL). The study did not meet either primary objective of demonstrating a reduction in risk for all-cause mortality or cardiovascular morbidity (darbepoetin alfa vs placebo; HR 1.05, 95% CI (0.94, 1.17)), or all-cause mortality or end stage renal disease (ESRD) (darbepoetin alfa vs placebo; HR 1.06, 95% CI (0.95, 1.19)). Analysis of the individual components of the composite endpoints showed the following HR (95% CI): death 1.05 (0.92, 1.21), congestive heart failure (CHF) 0.89 (0.74, 1.08), myocardial infarction (MI) 0.96 (0.75, 1.23), stroke 1.92 (1.38, 2.68), hospitalization for myocardial ischemia 0.84 (0.55, 1.27), ESRD 1.02 (0.87, 1.18). Pooled post-hoc analyses of clinical studies of ESAs have been performed in chronic renal failure patients (on dialysis, not on dialysis, in diabetic and non-diabetic patients). A tendency towards increased risk estimates for all-cause mortality, cardiovascular and cerebrovascular events associated with higher cumulative ESA doses independent of the diabetes or dialysis status was observed (see sections 4.2 and 4.4). Pediatric population In a randomized clinical study 114 pediatric patients aged 2 to 18 with chronic kidney disease receiving or not receiving dialysis who were anemic (hemoglobin < 10.0 g/dL) and not being treated with an ESA were administered darbepoetin alfa weekly (n = 58) or once every two weeks (n = 56) for the correction of anemia. Hemoglobin concentrations were corrected to ≥ 10 g/dL in > 98% (p < 0.001) of pediatric patients administered darbepoetin alfa once weekly and 84% (p = 0.293) once every two weeks. At the time hemoglobin ≥ 10.0 g/dL was first achieved, the mean (SD) weight-adjusted dose was 0.48 (0.24) mcg/kg (range: 0.0 to 1.7 mcg/kg) weekly for the once weekly group and 0.76 (0.21) mcg/kg (range: 0.3 to 1.5 mcg/kg) biweekly for the once every two-week group. In a clinical study in 124 pediatric patients with chronic kidney disease receiving or not receiving dialysis aged 1 to 18, patients that were stable on epoetin alfa were randomized to receive either darbepoetin alfa administered once weekly (subcutaneously or intravenously) using a dose conversion ratio of 238:1 or to continue with epoetin alfa therapy at the current dose, schedule, and route of administration. The primary efficacy endpoint [change in hemoglobin between baseline and the evaluation period (week 21-28)] was comparable between the two groups. The mean hemoglobin for r-HuEPO and darbepoetin alfa at baseline was 11.1 (SD 0.7) g/dL and 11.3 (SD 0.6) g/dL, respectively. The mean hemoglobin at week 28 for r-HuEPO and darbepoetin alfa was 11.1 (SD 1.4) g/dL and 11.1 (SD 1.1) g/dL, respectively. In an European observational registry study which enrolled 319 pediatric patients with chronic kidney disease (13 (4.1%) patients < 1 year of age, 83 (26.0%) patients 1-< 6 years of age, 90 (28.2%) patients 6-< 12 years of age, and 133 (41.7%) patients ≥ 12 years of age) receiving darbepoetin alfa, mean hemoglobin concentrations ranging between 11.3 and 11.5 g/dL and mean weight-adjusted darbepoetin alfa doses remained relatively constant (between 2.31 mcg/kg month and 2.67 mcg/kg month) over the study period for the entire study population. In these studies, no meaningful differences were identified between the safety profile for pediatric patients and that previously reported for adult patients (see section 4.8). Cancer Patients Receiving Chemotherapy EPO-ANE-3010, a randomized, open-label, multicenter study was conducted in 2,098 anemic women with metastatic breast cancer, who received first line or second line chemotherapy. This was a non inferiority study designed to rule out a 15% risk increase in tumor progression or death of epoetin alfa plus standard of care (SOC) as compared with SOC alone. At the time of clinical data cutoff, the median progression free survival (PFS) per investigator assessment of disease progression was 7.4 months in each arm (HR 1.09, 95% CI: 0.99, 1.20), indicating the study objective was not met. Significantly fewer patients received RBC transfusions in the epoetin alfa plus SOC arm (5.8% versus 11.4%); however, significantly more patients had thrombotic vascular events in the epoetin alfa plus SOC arm (2.8% versus 1.4%). At the final analysis, 1,653 deaths were reported. Median overall survival in the epoetin alfa plus SOC group was 17.8 months compared with 18.0 months in the SOC alone group (HR 1.07, 95% CI: 0.97, 1.18). The median time to progression (TTP) based on investigator-determined progressive disease (PD) was 7.5 months in the epoetin alfa plus SOC group and 7.5 months in the SOC group (HR 1.099, 95% CI: 0.998, 1.210). The median TTP based on IRC-determined PD was 8.0 months in the epoetin alfa plus SOC group and 8.3 months in the SOC group (HR 1.033, 95% CI: 0.924, 1.156). In a prospective, randomized double-blind, placebo-controlled study conducted in 314 lung cancer patients receiving platinum containing chemotherapy there was a significant reduction in transfusion requirements (p < 0.001). Clinical studies have demonstrated that darbepoetin alfa had similar effectiveness when administered as a single injection either once every three weeks, once every two weeks, or weekly without any increase in total dose requirements. The safety and effectiveness of once every three weeks dosing of ARANESP® therapy in reducing the requirement for red blood cell transfusions in patients undergoing chemotherapy was assessed in a randomized, double-blind, multinational study. This study was conducted in 705 anemic patients with non-myeloid malignancies receiving multi-cycle chemotherapy. Patients were randomized to receive ARANESP® at 500 mcg once every three weeks or 2.25 mcg/kg once weekly. In both groups, the dose was reduced by 40% of the previous dose (e.g., for first dose reduction, to 300 mcg in the once every three weeks group and 1.35 mcg/kg in the once weekly group) if hemoglobin increased by more than 1 g/dL in a 14-day period. In the once every three weeks group, 72% of patients required dose reductions. In the once weekly group, 75% of patients required dose reductions. This study supports 500 mcg once every three weeks being comparable to once weekly administration with respect to the incidence of subjects receiving at least one red blood cell transfusion from week 5 to the end of treatment phase. In a prospective, randomized double-blind, placebo-controlled study conducted in 344 anemic patients with lymphoproliferative malignancies receiving chemotherapy there was a significant reduction in transfusion requirements and an improvement in hemoglobin response (p < 0.001). Improvement in fatigue, as measured by the Functional Assessment of Cancer Therapy-fatigue (FACT-fatigue) scale, was also observed. Erythropoietin is a growth factor that primarily stimulates red blood cell production. Erythropoietin receptors may be expressed on the surface of a variety of tumor cells. Survival and tumor progression have been examined in five large controlled studies involving a total of 2,833 patients, of which four were double-blind placebo-controlled studies and one was an open-label study. Two of the studies recruited patients who were being treated with chemotherapy. The target hemoglobin concentration in two studies was > 13 g/dL; in the remaining three studies it was 12- 14 g/dL. In the open-label study there was no difference in overall survival between patients treated with recombinant human erythropoietin and controls. In the four placebo-controlled studies the hazard ratios for overall survival ranged between 1.25 and 2.47 in favor of controls. These studies have shown a consistent unexplained statistically significant excess mortality in patients who have anemia associated with various common cancers who received recombinant human erythropoietin compared to controls. Overall survival outcome in the trials could not be satisfactorily explained by differences in the incidence of thrombosis and related complications between those given recombinant human erythropoietin and those in the control group. In a randomized, double-blind, placebo-controlled phase 3 study 2,549 adult patients with anemia receiving chemotherapy for the treatment of advanced stage non-small cell lung cancer (NSCLC), were randomized 2:1 to darbepoetin alfa or placebo and treated to a maximum Hb of 12 g/dL. The results showed non-inferiority for the primary endpoint of overall survival with a median survival for darbepoetin alfa versus placebo of 9.5 and 9.3 months, respectively (stratified HR 0.92; 95% CI: 0.83– 1.01). The secondary endpoint of progression free survival was 4.8 and 4.3 months, respectively (stratified HR 0.95; 95% CI: 0.87–1.04), ruling out the pre-defined 15% risk increase. A systematic review has also been performed involving more than 9,000 cancer patients participating in 57 clinical trials. Meta-analysis of overall survival data produced a hazard ratio point estimate of 1.08 in favor of controls (95% CI: 0.99, 1.18; 42 trials and 8,167 patients). An increased relative risk of thromboembolic events (RR 1.67, 95% CI: 1.35, 2.06; 35 trials and 6,769 patients) was observed in patients treated with recombinant human erythropoietin. There is therefore consistent evidence to suggest that there may be significant harm to patients with cancer who are treated with recombinant human erythropoietin. The extent to which these outcomes might apply to the administration of recombinant human erythropoietin to patients with cancer, treated with chemotherapy to achieve hemoglobin concentrations less than 13 g/dL, is unclear because few patients with these characteristics were included in the data reviewed. A patient-level data analysis has also been performed on more than 13,900 cancer patients (chemo-, radio-, chemoradio-, or no therapy) participating in 53 controlled clinical trials involving several epoetins. Meta-analysis of overall survival data produced a hazard ratio point estimate of 1.06 in favor of controls (95% CI: 1.00, 1.12; 53 trials and 13,933 patients) and for the cancer patients receiving chemotherapy, the overall survival hazard ratio was 1.04 (95% CI: 0.97, 1.11; 38 trials and 10,441 patients). Meta-analyses also indicate consistently a significantly increased relative risk of thromboembolic events in cancer patients receiving recombinant human erythropoietin (see section 4.4).
Pharmacokinetic Properties
5.2 Pharmacokinetic Properties Due to its increased carbohydrate content the level of darbepoetin alfa in the circulation remains above the minimum stimulatory concentration for erythropoiesis for longer than the equivalent molar dose of r-HuEPO, allowing darbepoetin alfa to be administered less frequently to achieve the same biological response. Chronic Renal Failure Patients The pharmacokinetics of darbepoetin alfa has been studied clinically in chronic renal failure patients following intravenous and subcutaneous administration. The terminal half-life of darbepoetin alfa is 21 hours (SD 7.5) when administered intravenously. Clearance of darbepoetin alfa is 1.9 mL/hr/kg (SD 0.56) and the volume of distribution (Vss) is approximately equal to plasma volume (50 mL/kg). Bioavailability is 37% with subcutaneous administration. Following monthly administration of darbepoetin alfa, at subcutaneous doses ranging from 0.6 to 2.1 mcg/kg, the terminal half-life was 73 hours (SD 24). The longer terminal half-life of darbepoetin alfa administered subcutaneously compared to intravenously is due to subcutaneous absorption kinetics. In clinical studies, minimal accumulation was observed with either route of administration. In preclinical studies it has been shown that renal clearance is minimal (up to 2% of total clearance), and does not affect the serum half-life. Data from 809 patients receiving ARANESP® in European clinical studies were analyzed to assess the dose required to maintain hemoglobin; no difference was observed between the average weekly dose administered via the intravenous or subcutaneous routes of injection. The pharmacokinetics of darbepoetin alfa in pediatric patients (2 to 16 years) with CRF who were either receiving or not receiving dialysis was assessed for sampling periods up to 2 weeks (336 hours) after one or two subcutaneous or intravenous doses. Where the same sampling duration was used, observed pharmacokinetic data and population pharmacokinetic modelling demonstrated that the pharmacokinetics of darbepoetin alfa was similar for pediatric and adult patients with CRF. In a phase 1 pharmacokinetic study, following intravenous administration, an approximate 25% difference between pediatric and adult patients in the area under the curve from time 0 to infinity (AUC[0-∞]) was observed; however, this difference was less than the 2-fold range in AUC(0-∞) observed for the pediatric patients. AUC (0-∞) was similar between adult and pediatric patients with CRF following subcutaneous administration. Half-life was also similar between adult and pediatric patients with CRF following both intravenous and subcutaneous administration. Cancer Patients Receiving Chemotherapy Following subcutaneous administration of 2.25 mcg/kg to adult cancer patients a mean peak concentration of 10.6 ng/mL (SD 5.9) of darbepoetin alfa was reached at a mean time of 91 hours (SD 19.7). These parameters were consistent with dose linear pharmacokinetics over a wide dose range (0.5 to 8 mcg/kg weekly and 3 to 9 mcg/kg every two weeks). Pharmacokinetic parameters did not change on multiple dosing over 12 weeks (dosing every week or every two weeks). There was an expected moderate (< 2 fold) increase in serum concentration as steady state was approached, but no unexpected accumulation upon repeated administration. A pharmacokinetic study in patients with chemotherapy-induced anemia treated with 6.75 mcg/kg darbepoetin alfa administered SC every 3 weeks in combination with chemotherapy was conducted which allowed for full characterization of the terminal half-life. In this study, mean (SD) terminal half-life was 74 (SD 27) hours.

פרטי מסגרת הכללה בסל
התרופה תינתן בכל אחד מאלה: 1. אנמיה חמורה (severe anemia) בחולי אי ספיקה כלייתית כרונית. 2. חולים אנמיים הסובלים ממחלה ממאירה והמקבלים טיפול פעיל ייעודי במחלתם וכן לחולים הסובלים ממיאלומה נפוצה (multiple myeloma) או מהתסמונת המיאלודיספלסטית (myelodisplastic syndrome) שנתקיימו בהם כל אלה: 1. אחד מהתנאים האלה: א. רמת המוגלובין נמוכה מ-8 גרם %. ב. החולה מרותק למיטתו בגלל אנמיה המלווה במחלת לב איסכמית או באי ספיקה לבבית. ג. החולה נזקק לקבלת שתי מנות דם לפחות פעם בשבועיים במשך חודשיים. 2. נשללה סיבה אחרת לאנמיה שאינה קשורה לטיפול הייעודי במחלתם האמורה לעיל ובכלל זה דימום, חוסר ברזל, חוסר חומצה פולית, חוסר ויטמין B12 והמוליזה. 3. רמת אריתרופואטין בנסיוב נמוכה מ-100 mu/ml.
מסגרת הכללה בסל
התוויות הכלולות במסגרת הסל
| התוויה | תאריך הכללה | תחום קליני | Class Effect | מצב מחלה |
|---|---|---|---|---|
| EPOETIN THETA (R-HUEPO) | ||||
| METHOXY POLYETHYLENE GLYCOL-EPOETIN BETA | ||||
| EPOETIN ALFA | ||||
| EPOETIN BETA | ||||
| DARBEPOETIN ALFA | ||||
| oncology | ||||
| CKD |
שימוש לפי פנקס קופ''ח כללית 1994
לא צוין
תאריך הכללה מקורי בסל
01/04/2004
הגבלות
תרופה מוגבלת לרישום ע'י רופא מומחה או הגבלה אחרת
מידע נוסף
עלון מידע לצרכן
22.03.18 - עלון לצרכן 14.06.21 - עלון לצרכן אנגלית 14.06.21 - עלון לצרכן אנגלית 14.06.21 - עלון לצרכן אנגלית 14.06.21 - עלון לצרכן עברית 14.06.21 - עלון לצרכן עברית 14.06.21 - עלון לצרכן ערבית 14.06.21 - עלון לצרכן ערבית 14.06.21 - עלון לצרכן ערבית 28.11.11 - החמרה לעלון 11.07.12 - החמרה לעלון 20.04.21 - החמרה לעלון 14.06.21 - החמרה לעלוןלתרופה במאגר משרד הבריאות
אראנספ 40 מק"ג