Quest for the right Drug
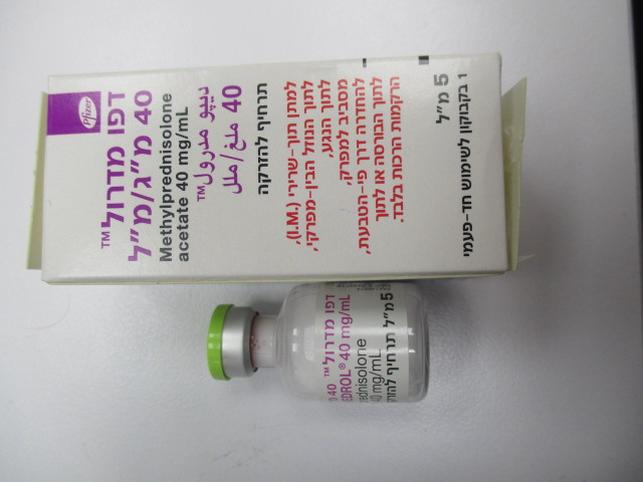
דפו מדרול 40 מ"ג/מ"ל DEPO MEDROL 40 MG/ML (METHYLPREDNISOLONE ACETATE)
תרופה במרשם
תרופה בסל
נרקוטיקה
ציטוטוקסיקה
צורת מתן:
זריקה ליד המפרק, תוך-שרירי, תוך מפרקי, לתוך פצע, לתוך נוזל העצם, להחדרה רקטלית, לרקמות רכות : PERIARTICULAR, I.M, INTRA-ARTICULAR, INTRA-LESIONAL, INTRABURSAL, INTRARECTAL INSTILLATION, SOFT TISSUES
צורת מינון:
תרחיף להזרקה : SUSPENSION FOR INJECTION
עלון לרופא
מינוניםPosology התוויות
Indications תופעות לוואי
Adverse reactions התוויות נגד
Contraindications אינטראקציות
Interactions מינון יתר
Overdose הריון/הנקה
Pregnancy & Lactation אוכלוסיות מיוחדות
Special populations תכונות פרמקולוגיות
Pharmacological properties מידע רוקחי
Pharmaceutical particulars אזהרת שימוש
Special Warning עלון לרופא
Physicians Leaflet
Special Warning : אזהרת שימוש
4.4 Special warnings and precautions for use Warnings and Precautions: Undesirable effects may be minimised by using the lowest effective dose for the minimum period. Frequent patient review is required to appropriately titrate the dose against disease activity (see section 4.2). Depo-Medrol vials are intended for single dose use only. Any multidose use of the product may lead to contamination. Severe medical events have been reported in association with the intrathecal/epidural routes of administration (see section 4.8). Appropriate measures must be taken to avoid intravascular injection. Due to the absence of a true tendon sheath, the Achilles tendon should not be injected with Depo-Medrol. While crystals of adrenal steroids in the dermis suppress inflammatory reactions, their presence may cause disintegration of the cellular elements and physiochemical changes in the ground substance of the connective tissue. The resultant infrequently occurring dermal and/or subdermal changes may form depressions in the skin at the injection site. The degree to which this reaction occurs will vary with the amount of adrenal steroid injected. Regeneration is usually complete within a few months or after all crystals of the adrenal steroid have been absorbed. In order to minimize the incidence of dermal and subdermal atrophy, care must be exercised not to exceed recommended doses in injections. Multiple small injections into the area of the lesion should be made whenever possible. The technique of intra-articular and intramuscular injection should include precautions against injection or leakage into the dermis. Injection into the deltoid muscle should be avoided because of a high incidence of subcutaneous atrophy. Intralesional doses should not be placed too superficially, particularly in easily visible sites in patients with deeply pigmented skins, since there have been rare reports of subcutaneous atrophy and depigmentation. Systemic absorption of methylprednisolone occurs following intra-articular injection of Depo- Medrol. Systemic as well as local effects can therefore be expected. Adrenal cortical atrophy develops during prolonged therapy and may persist for months after stopping treatment. In patients who have received more than physiological doses of systemic corticosteroids (approximately 6 mg methylprednisolone) for greater than 3 weeks, withdrawal should not be abrupt. How dose reduction should be carried out depends largely on whether the disease is likely to relapse as the dose of systemic corticosteroids is reduced. Clinical assessment of disease activity may be needed during withdrawal. If the disease is unlikely to relapse on withdrawal of systemic corticosteroids, but there is uncertainty about HPA suppression, the dose of systemic corticosteroid may be reduced rapidly to physiological doses. Once a daily dose of 6 mg methylprednisolone is reached, dose reduction should be slower to allow the HPA-axis to recover. The following precautions apply for parenteral corticosteroids: Following intra-articular injection, the occurrence of a marked increase in pain accompanied by local swelling, further restriction of joint motion, fever, and malaise are suggestive of 2024-0093542 Page 7 of 21 septic arthritis. If this complication occurs and the diagnosis of sepsis is confirmed, appropriate antimicrobial therapy should be instituted. Local injection of a steroid into a previously infected joint is to be avoided. Intra-articular corticosteroids are associated with a substantially increased risk of inflammatory response in the joint, particularly bacterial infection introduced with the injection. Charcot-like arthropathies have been reported particularly after repeated injections. Appropriate examination of any joint fluid present is necessary to exclude any bacterial infection, prior to injection. Corticosteroids should not be injected into unstable joints. Sterile technique is necessary to prevent infections or contamination. The slower rate of absorption by intramuscular administration should be recognised. Immunosuppressant Effects/Increased Susceptibility to Infections Corticosteroids may increase susceptibility to infection, may mask some signs of infection, and new infections may appear during their use. Suppression of the inflammatory response and immune function increases the susceptibility to fungal, viral and bacterial infections and their severity. The clinical presentation may often be atypical and may reach an advanced stage before being recognised. With increasing doses of corticosteroids, the rate of occurrence of infectious complications increases. Do not use intra-synovially, intrabursally or intratendinous administration for local effect in the presence of acute infection. Persons who are on drugs which suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in non-immune children or adults on corticosteroids. Chickenpox is of serious concern since this normally minor illness may be fatal in immunosuppressed patients. Patients (or parents of children) without a definite history of chickenpox should be advised to avoid close personal contact with chickenpox or herpes zoster and if exposed they should seek urgent medical attention. Passive immunization with varicella/zoster immunoglobin (VZIG) is needed by exposed non-immune patients who are receiving systemic corticosteroids or who have used them within the previous 3 months; this should be given within 10 days of exposure to chickenpox. If a diagnosis of chickenpox is confirmed, the illness warrants specialist care and urgent treatment. Corticosteroids should not be stopped and the dose may need to be increased. Live vaccines should not be given to individuals with impaired immune responsiveness. The antibody response to other vaccines may be diminished. The use of Depo- Medrol in active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate antituberculous regimen. If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary as reactivation of the disease may occur. During prolonged corticosteroid therapy, these patients should receive chemoprophylaxis. The role of corticosteroids in septic shock has been controversial, with early studies reporting both beneficial and detrimental effects. More recently, supplemental corticosteroids have been suggested to be beneficial in patients with established septic shock who exhibit adrenal 2024-0093542 Page 8 of 21 insufficiency. However, their routine use in septic shock is not recommended. A systematic review of short-course high-dose corticosteroids did not support their use. However, meta- analyses and a review suggest that longer courses (5-11 days) of low-dose corticosteroids might reduce mortality, especially in patients with vasopressor-dependent septic shock. Immune System Effects Allergic reactions may occur. Because rare instances of skin reactions and anaphylactic/anaphylactoid reactions have occurred in patients receiving corticosteroid therapy, appropriate precautionary measures should be taken prior to administration, especially when the patient has a history of drug allergy. Endocrine Effects Pharmacologic doses of corticosteroids administered for prolonged periods may result in hypothalamic-pituitary-adrenal (HPA) suppression (secondary adrenocortical insufficiency). The degree and duration of adrenocortical insufficiency produced is variable among patients and depends on the dose, frequency, time of administration, and duration of glucocorticoid therapy. This effect may be minimized by use of alternate-day therapy. In addition, acute adrenal insufficiency leading to a fatal outcome may occur if glucocorticoids are withdrawn abruptly. Drug-induced secondary adrenocortical insufficiency may therefore be minimized by gradual reduction of dosage. This type of relative insufficiency may persist for months after discontinuation of therapy; therefore, in any situation of stress occurring during that period, hormone therapy should be reinstituted. Salt and/or a mineralocorticoid are only needed if mineralocorticoid secretion is impaired. A steroid “withdrawal syndrome,” seemingly unrelated to adrenocortical insufficiency, may also occur following abrupt discontinuance of glucocorticoids. This syndrome includes symptoms such as: anorexia, nausea, vomiting, lethargy, headache, fever, joint pain, desquamation, myalgia, weight loss, and/or hypotension. These effects are thought to be due to the sudden change in glucocorticoid concentration rather than to low corticosteroid levels. Abrupt withdrawal of systemic corticosteroid treatment, which has continued up to 3 weeks is appropriate if it considered that the disease is unlikely to relapse. Abrupt withdrawal of doses up to 32 mg daily of methylprednisolone for 3 weeks is unlikely to lead to clinically relevant HPA-axis suppression, in the majority of patients. In the following patient groups, gradual withdrawal of systemic corticosteroid therapy should be considered even after courses lasting 3 weeks or less: • Patients who have had repeated courses of systemic corticosteroids, particularly if taken for greater than 3 weeks. • When a short course has been prescribed within one year of cessation of long-term therapy (months or years). • Patients who may have reasons for adrenocortical insufficiency other than exogenous corticosteroid therapy. • Patients receiving doses of systemic corticosteroid greater than 32 mg daily of methylprednisolone. • Patients repeatedly taking doses in the evening. Because glucocorticoids can produce or aggravate Cushing’s syndrome, glucocorticoids should be avoided in patients with Cushing’s disease. There is an enhanced effect of corticosteroids on patients with hypothyroidism. 2024-0093542 Page 9 of 21 Thyrotoxic Periodic Paralysis (TPP) can occur in patients with hyperthyroidism and with methylprednisolone-induced hypokalaemia. TPP must be suspected in patients treated with methylprednisolone presenting signs or symptoms of muscle weakness, especially in patients with hyperthyroidism. If TPP is suspected, levels of blood potassium must be immediately monitored and adequately managed to ensure the restoration of normal levels of blood potassium. Metabolism and Nutrition Corticosteroids, including methylprednisolone, can increase blood glucose, worsen pre- existing diabetes, and predispose those on long-term corticosteroid therapy to diabetes mellitus. Psychiatric Effects Patients and/or carers should be warned that potentially severe psychiatric adverse reactions may occur with systemic steroids (see section 4.8). Symptoms typically emerge within a few days or weeks of starting treatment. Risks may be higher with high doses/systemic exposure (see section 4.5), although dose levels do not allow prediction of the onset, type, severity or duration of reactions. Most reactions recover after either dose reduction or withdrawal, although specific treatment may be necessary. Patients/carers should be encouraged to seek medical advice if worrying psychological symptoms develop, especially if depressed mood or suicidal ideation is suspected. Patients/carers should be alert to possible psychiatric disturbances that may occur either during or immediately after dose tapering/withdrawal of systemic steroids, although such reactions have been reported infrequently. Particular care is required when considering the use of systemic corticosteroids in patients with existing or previous history of severe affective disorders in themselves or in their first degree relatives. These would include depressive or manic-depressive illness and previous steroid psychosis. Nervous System Effects Corticosteroids should be used with caution in patients with seizure disorders. Corticosteroids should be used with caution in patients with myasthenia gravis (also see myopathy statement in Musculoskeletal Effects section). There have been reports of epidural lipomatosis in patients taking corticosteroids, typically with long-term use at high doses. Ocular Effects Visual disturbance may be reported with systemic and topical corticosteroid use. If a patient presents with symptoms such as blurred vision or other visual disturbances, the patient should be considered for referral to an ophthalmologist for evaluation of possible causes which may include cataract, glaucoma or rare diseases such as central serous chorioretinopathy (CSCR) which have been reported after use of systemic and topical corticosteroids. Central serous chorioretinopathy, may lead to retinal detachment. Prolonged use of corticosteroids may produce posterior subcapsular cataracts and nuclear cataracts (particularly in children), exophthalmos, or increased intraocular pressure, which may result in glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to fungi or viruses. Corticosteroids should be used cautiously in patients with ocular herpes simplex, because of possible corneal perforation. 2024-0093542 Page 10 of 21 Cardiac Effects Adverse effects of glucocorticoids on the cardiovascular system, such as dyslipidaemia and hypertension, may predispose treated patients with existing cardiovascular risk factors to additional cardiovascular effects, if high doses and prolonged courses are used. Accordingly, corticosteroids should be employed judiciously in such patients and attention should be paid to risk modification and additional cardiac monitoring if needed. Systemic corticosteroids should be used with caution, and only if strictly necessary, in cases of congestive heart failure. Vascular Effects Corticosteroids should be used with caution in patients with hypertension. Thrombosis including venous thromboembolism has been reported to occur with corticosteroids. As a result corticosteroids should be used with caution in patients who have or may be predisposed to thromboembolic disorders. Gastrointestinal Effects High doses of corticosteroids may produce acute pancreatitis. There is no universal agreement on whether corticosteroids per se are responsible for peptic ulcers encountered during therapy; however, glucocorticoid therapy may mask the symptoms of peptic ulcer so that perforation or haemorrhage may occur without significant pain. Glucocorticoid therapy may mask peritonitis or other signs or symptoms associated with gastrointestinal disorders such as perforation, obstruction or pancreatitis. In combination with NSAIDs, the risk of developing gastrointestinal ulcers is increased. Corticosteroids should be used with caution in nonspecific ulcerative colitis, if there is a probability of impending perforation, abscess or other pyogenic infection. Caution must also be used in diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, when steroids are used as direct or adjunctive therapy. Hepatobiliary Effects Drug induced liver injury including acute hepatitis or liver enzyme increase can result from cyclical pulsed IV methylprednisolone (usually at initial dose > 1 g / day). Rare cases of hepatotoxicity have been reported. The time to onset can be several weeks or longer. In the majority of case reports resolution of the adverse events has been observed after treatment was discontinued. Therefore, appropriate monitoring is required. Corticosteroids should be used with caution in patients with liver failure or cirrhosis. Musculoskeletal Effects An acute myopathy has been reported with the use of high doses of corticosteroids, most often occurring in patients with disorders of neuromuscular transmission (e.g., myasthenia gravis), or in patients receiving concomitant therapy with anticholinergics, such as neuromuscular blocking drugs (e.g., pancuronium). This acute myopathy is generalized, may involve ocular and respiratory muscles, and may result in quadriparesis. Elevations of creatine kinase may occur. Clinical improvement or recovery after stopping corticosteroids may require weeks to years. Osteoporosis is a common but infrequently recognized adverse effect associated with a long- term use of large doses of glucocorticoid. Renal and Urinary Disorders 2024-0093542 Page 11 of 21 Caution is required in patients with systemic sclerosis because an increased incidence of scleroderma renal crisis has been observed with corticosteroids, including methylprednisolone. Blood pressure and renal function (s-creatinine) should therefore be routinely checked. When renal crisis is suspected, blood pressure should be carefully controlled. Corticosteroids should be used with caution in patients with renal insufficiency. Investigations Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. Dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion. Care should be taken for patients receiving cardioactive drugs such as digoxin because of steroid induced electrolyte disturbance/potassium loss (see section 4.8). Injury, Poisoning and Procedural Complications Systemic corticosteroids are not indicated for, and therefore should not be used to treat, traumatic brain injury, a multicenter study revealed an increased mortality at 2 weeks and 6 months after injury in patients administered methylprednisolone sodium succinate compared to placebo. A causal association with methylprednisolone sodium succinate treatment has not been established. Other Corticosteroids should be used with caution in patients with a predisposition to thrombophlebitis. Co-treatment with CYP3A inhibitors, including cobicistat-containing products, is expected to increase the risk of systemic side-effects. The combination should be avoided unless the benefit outweighs the increased risk of systemic corticosteroid side-effects, in which case patients should be monitored for systemic corticosteroid side-effects (see section 4.5). Aspirin and nonsteroidal anti-inflammatory agents should be used cautiously in conjunction with corticosteroids. Pheochromocytoma crisis, which can be fatal, has been reported after administration of systemic corticosteroids. Corticosteroids should only be administered to patients with suspected or identified pheochromocytoma after an appropriate risk/benefit evaluation. In post marketing experience tumour lysis syndrome (TLS) has been reported in patients with malignancies, including haematological malignancies and solid tumours, following the use of systemic corticosteroids alone or in combination with other chemotherapeutic agents. Patients at high risk of TLS, such as patients with tumours that have a high proliferative rate, high tumour burden and high sensitivity to cytotoxic agents, should be monitored closely and appropriate precautions should be taken. Depo-Medrol contains less than 1 mmol sodium (23 mg) per vial, that is to say essentially ‘sodium-free’. Paediatric population Corticosteroids cause growth retardation in infancy, childhood and adolescence which may be irreversible. Growth and development of infants and children on prolonged corticosteroid 2024-0093542 Page 12 of 21 therapy should be carefully observed. Treatment should be limited to the minimum dosage for the shortest possible time. The use of such a regimen should be restricted to those most serious indications. Infants and children on prolonged corticosteroid therapy are at special risk from raised intracranial pressure. High doses of corticosteroids may produce pancreatitis in children.
Effects on Driving
4.7 Effects on ability to drive and use machines The effect of corticosteroids on the ability to drive or use machinery has not been systematically evaluated. Undesirable effects, such as dizziness, vertigo, visual disturbances, and fatigue are possible after treatment with corticosteroids. If affected, patients should not drive or operate machinery. 2024-0093542 Page 15 of 21

שימוש לפי פנקס קופ''ח כללית 1994
Rheumatoid arthritis, osteoarthritis, other arthritic conditions by intra-articular injection, inflammatory, allergic & rheumatic conditions requiring a glucocorticoid effect, in patients for whom treatment with oral corticosteroid is not feasible
תאריך הכללה מקורי בסל
01/01/1995
הגבלות
תרופה שאושרה לשימוש כללי בקופ'ח
מידע נוסף
עלון מידע לצרכן
24.10.12 - עלון לצרכן 02.05.16 - עלון לצרכן 16.08.18 - עלון לצרכן 18.12.18 - עלון לצרכן 25.07.22 - עלון לצרכן אנגלית 25.07.22 - עלון לצרכן עברית 25.07.22 - עלון לצרכן ערבית 23.06.23 - עלון לצרכן עברית 06.12.23 - עלון לצרכן אנגלית 05.12.23 - עלון לצרכן עברית 06.12.23 - עלון לצרכן ערבית 12.04.24 - עלון לצרכן עברית 05.09.24 - עלון לצרכן אנגלית 05.09.24 - עלון לצרכן ערבית 25.11.24 - עלון לצרכן עברית 10.09.20 - החמרה לעלון 19.01.21 - החמרה לעלון 25.10.21 - החמרה לעלון 21.09.23 - החמרה לעלון 12.04.24 - החמרה לעלון 08.07.24 - החמרה לעלון 25.11.24 - החמרה לעלוןלתרופה במאגר משרד הבריאות
דפו מדרול 40 מ"ג/מ"ל